Abstract
Background:
Among patients undergoing high-risk cancer surgery, little is known regarding how much time is spent away from home, either the hospital or in a skilled nursing facility, in the year following surgery.
Study Design:
This is a retrospective cohort study using Medicare Inpatient claims and the Minimum Data Set (MDS) to look at beneficiaries ages 65 and older undergoing cystectomy, pancreaticoduodenectomy, gastrectomy and esophagectomy from 2010–2012. Overall adjusted percentage of time spent at home, in the hospital, and in a facility was modeled for the year following surgery.
Results:
A total of 37,748 beneficiaries underwent high-risk cancer surgery during the study period and 28.3% died within 1 year. On average, beneficiaries had 1.5 ± 2.0 hospital readmissions, spent 13.9 ± 26.2 days in the hospital, had 1.5 ± 1.0 admissions to a facility and spent 37.2 ± 50.6 days in a facility in the year after surgery. Among beneficiaries who were alive and dead at one year, 13% and 25% of time was spent away from home, respectively. Beneficiaries who were initially discharged to a facility following surgery and died within 1 year spent 39% of their final year in the hospital and/or a facility.
Conclusion:
Time spent away from home in the hospital and/or nursing facility in the year following high-risk cancer surgery is substantial among Medicare beneficiaries. This information is crucial in counseling patients on post-operative expectations and may additionally influence pre-operative decision-making.
Keywords: Cystectomy, gastrectomy, pancreaticoduodenectomy, esophagectomy, Medicare, skilled nursing facility
Introduction
Many cancer diagnoses in older adults are associated with a poor prognosis. While many choose to undergo high-risk surgery for their cancer diagnoses, the recovery following such surgery can be long and arduous. The overwhelming majority of these patients survive the hospital admission during which the surgery is performed, however, greater than 10% will be discharged to skilled or assisted living facility,1,2 and 10–22% will be readmitted to the hospital within 30-days.3–9
While these statistics during the early postoperative period are staggering, little is known about where these individuals spend their time beyond the 30-day postoperative period. High rates of complications following these procedures, upwards of 20–50%,10–13 make it likely that patients will continue to require high levels of care, potentially requiring time spent in either in the hospital or in a skilled or assisted living facility. However, the amount of time is spent outside of the home in such institutions after high risk cancer surgery is currently unknown.
In order to address this knowledge gap, we conducted a retrospective cohort study of Medicare beneficiaries undergoing cystectomy, pancreaticoduodenectomy, gastrectomy and esophagectomy using Medicare claims data and the Minimum Data Set (MDS) for Nursing Home Residents from 2010 to 2012. Findings from this study will provide important information to assist in setting realistic post-operative expectations and planning, in addition to contributing important information related to healthcare utilization and cost related to the care for patients undergoing these procedures.
Materials and Methods
Subjects and Databases
We identified a cohort of Medicare beneficiaries undergoing cystectomy, pancreaticoduodenectomy, gastrectomy and esophagectomy from 2010–2012 using the Medicare Inpatient files. These files contain data on all fee-for-service inpatient hospitalizations for Medicare beneficiaries ages 65 and older. Individuals were identified using International Classification of Diseases, Ninth Revision (ICD-9), procedure codes with corresponding ICD-9 diagnosis codes for cancer (Supplemental Table). The Minimum Data Set (MDS) for Nursing Home Residents was used to determine time spent in a nursing home. The MDS is a quarterly mandatory assessment of all nursing home residents in the United States who receive Medicare or Medicaid benefits and is linked to the Medicare Inpatient Files.
Outcome measures
Our primary outcome of interest was the proportion of days that each beneficiary spent at home, in the hospital, and in a skilled or assisted living facility in the year following the surgical episode of care (starting from the discharge date of the index surgical encounter). The number of days spent in the hospital was calculated from the admission and discharge dates of all hospital encounters found in the Medicare Inpatient file. The number of days in the skilled or assisted living facility was obtained from the Minimum Data Set for Nursing Homes (MDS), which also includes admission and discharge dated to the facility. Date of death was abstracted from the Medicare Inpatient and Denominator data files.
Covariates
Demographic information on age, gender, race, discharge disposition, comorbidity, hospital length of hospital stay and calendar year were obtained from the Medicare Inpatient files. Discharge disposition from the encounter related to the index surgical procedure was reported either as to home without assistance or to a facility (including to a skilled nursing facility, other type of inpatient facility, hospice or other discharge destination). Comorbidity was calculated by the Charlson Comorbidity Index score, as previously described in the literature.14
Statistical Analysis
In order to account for beneficiaries who died within one year of surgery, we calculated the percent of time spent in the hospital and in a skilled or assisted living facility. To do this, we used the number of days in the hospital, or the number of days in the facility, as the numerator and the total number of days alive in the year following surgery as the denominator to calculate percentage of days in the hospital or facility, respectively. This calculation allowed us to obtain a percentage of time spent in each location, while accounting for the amount of time that each individual was alive during the study period. The percentage of time spent at home was then calculated by subtracting the percentage of days in the hospital and the percentage of days in a facility from 100% via the following formula:
Results were fit via a generalized linear model adjusting for procedure type (cystectomy, pancreaticoduodenectomy, gastrectomy and esophagectomy), age, gender, race, Charlson Comorbidity Index score, hospital length of stay, discharge disposition, and calendar year. Results are reported as stacked bar graphs illustrating percentage of time spent in each setting.
In order to better understand which beneficiaries died within 1-year and which were discharged to a facility following surgery, we performed separate relative risk regression models with Poisson distribution for the following independent variables: procedure type, age, gender, race, Charlson Comorbidity Index score, hospital length of stay, discharge disposition (where appropriate), and procedure year. For all analyses, p=0.05 on two-sided significance test with a 5% α level was considered statistically significant. Analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc).
Results
Summary characteristics of the study cohort are presented in Table 1. There were a total of 37,748 individuals in the cohort who underwent gastrectomy (25.9%), cystectomy (37.9%), pancreaticoduodenectomy (28.7%), and esophagectomy (7.5%). Overall, 10,700 (28.3%) of the study cohort died within one year of surgery. Subjects who died in the year following surgery were more likely, compared to subjects who were alive at one year after surgery, to have had a pancreaticoduodenectomy (33.1% compared to 27.0%, p<0.0001), to be older (mean age 75.8 ± 6.6 years compared to 74.3 ± 6.1 years, p<0.0001), to be black (10.0% compared to 8.3%, p<0.0001), to be discharged to a facility (33.6% compared to 18.6%, p<0.0001), and to have a higher Charlson Comorbidity Index score (9.7% had a score >4 compared to 5.0%, p<0,0001). These individuals also had longer hospital lengths of stay during the hospitalization wherein the index surgical procedure occurred (mean 15.4 ± 12.6 days compared to 11.1 ± 8.2 days, p<0.0001), had more hospital readmissions (mean 2.0 ± 2.1 compared to 1.3 ± 1.9, p<0.0001) and spent more days in the hospital in the year following surgery (19.7 ± 27.0 compared to 11.5 ± 25.4, p<0.0001). Individuals who died in the year following surgery had a similar number of admissions to a facility, compared to those who were alive 1-year following surgery, (1.5 ± 0.9 compared to 1.5 ± 1.0, p=0.2127) and spent fewer total number of days in a facility (31.6 ± 37.0 days compared to 41.0 ± 57.8 days, p<0.0001).
Table 1.
Patient characteristics up to 1 year after surgery.
| Characteristics | Entire Cohort N=37,748 | Subjects Alive at 1 year n=27,048 | Subjects dead at 1 year n=10,700 | P |
|---|---|---|---|---|
| Type of surgery/procedure, n (%) | ||||
| Gastrectomy | 9791 (25.9) | 7102 (26.3) | 2689 (25.1) | <.0001 |
| Cystectomy | 14294 (37.9) | 10571 (39.1) | 3723 (34.8) | |
| Pancreaticoduodenectomy | 10845 (28.7) | 7299 (27.0) | 3546 (33.1) | |
| Esophagectomy | 2818 (7.5) | 2076 (7.7) | 742 (6.9) | |
| Age (years), n (%) | ||||
| 65–69 | 11448 (30.3) | 8723 (32.3) | 2725 (25.5) | <.0001 |
| 70–74 | 8304 (22.0) | 6142 (22.7) | 2162 (20.2) | |
| 75–79 | 9133 (24.2) | 6485 (24.0) | 2648 (24.7) | |
| 80–84 | 6035 (16.0) | 3994 (14.8) | 2041 (19.1) | |
| ≥ 85 | 2828 (7.5) | 1704 (6.3) | 1124 (10.5) | |
| Mean ± SD | 74.8 ± 6.3 | 74.3 ± 6.1 | 75.8 ± 6.6 | <.0001 |
| Gender, n (%) | ||||
| Male | 25021 (66.3) | 17954 (66.4) | 7067 (66.0) | 0.5391 |
| Female | 12727 (33.7) | 9094 (33.6) | 3633 (34.0) | |
| Race, n (%) | ||||
| White | 31778 (84.2) | 22782 (84.2) | 8996 (84.1) | <.0001 |
| Black | 3314 (8.8) | 2248 (8.3) | 1066 (10.0) | |
| Other | 2656 (7.0) | 2018 (7.5) | 638 (6.0) | |
| Disposition after hospitalization, n (%) | ||||
| Home (no assistance) | 29125 (77.2) | 22015 (81.4) | 7110 (66.4) | <.0001 |
| Facility (SNF, Hospice, Inpatient) | 8623 (22.8) | 5033 (18.6) | 3590 (33.6) | |
| Charlson Comorbidity Index Score, n (%) | ||||
| 0–1 | 17525 (46.4) | 13620 (50.4) | 3905 (36.5) | <.0001 |
| 2–4 | 17831 (47.2) | 12079 (44.7) | 5752 (53.8) | |
| >4 | 2392 (6.3) | 1349 (5.0) | 1043 (9.7) | |
| Hospital length of stay (LOS) in days, Mean ± SD | 12.3 ± 9.9 | 11.1 ± 8.2 | 15.4 ± 12.6 | <.0001 |
| Number of hospital admissions, Mean ± SD | 1.5 ± 2.0 | 1.3 ± 1.9 | 2.0 ± 2.1 | <.0001 |
| Number of days spent in hospital after index admission, Mean ± SD | 13.9 ± 26.2 | 11.5 ± 25.4 | 19.7 ± 27.0 | <.0001 |
| Number of SNF admissions, Mean ± SD | 1.5 ± 1.0 | 1.5 ± 1.0 | 1.5 ± 0.9 | 0.2127 |
| Number of days in SNF, Mean ± SD | 37.2 ± 50.6 | 41.0 ± 57.8 | 31.6 ± 37.0 | <.0001 |
| Death within 1 year, cumulative n (%) | ||||
| 1 month | 1364 (3.6) | -- | 1364 (12.7) | |
| 3 months | 3278 (8.7) | -- | 3278 (30.6) | |
| 6 months | 6018 (15.9) | -- | 6018 (56.2) | |
| 9 months | 8514 (22.6) | -- | 8514 (79.6) | |
Figure 1 illustrates the percentage of time spent at home, in the hospital, and in a facility among individuals were alive versus dead at one year following surgery. Subjects who were dead one year after surgery spent 75.5% of their time at home (compared to 87.1% of time spent at home for the subjects who were alive). They also spent a higher percentage of time in the hospital (16.8% compared to 7.2%) and in a facility (7.7% compared to 5.7%).
Figure 1.
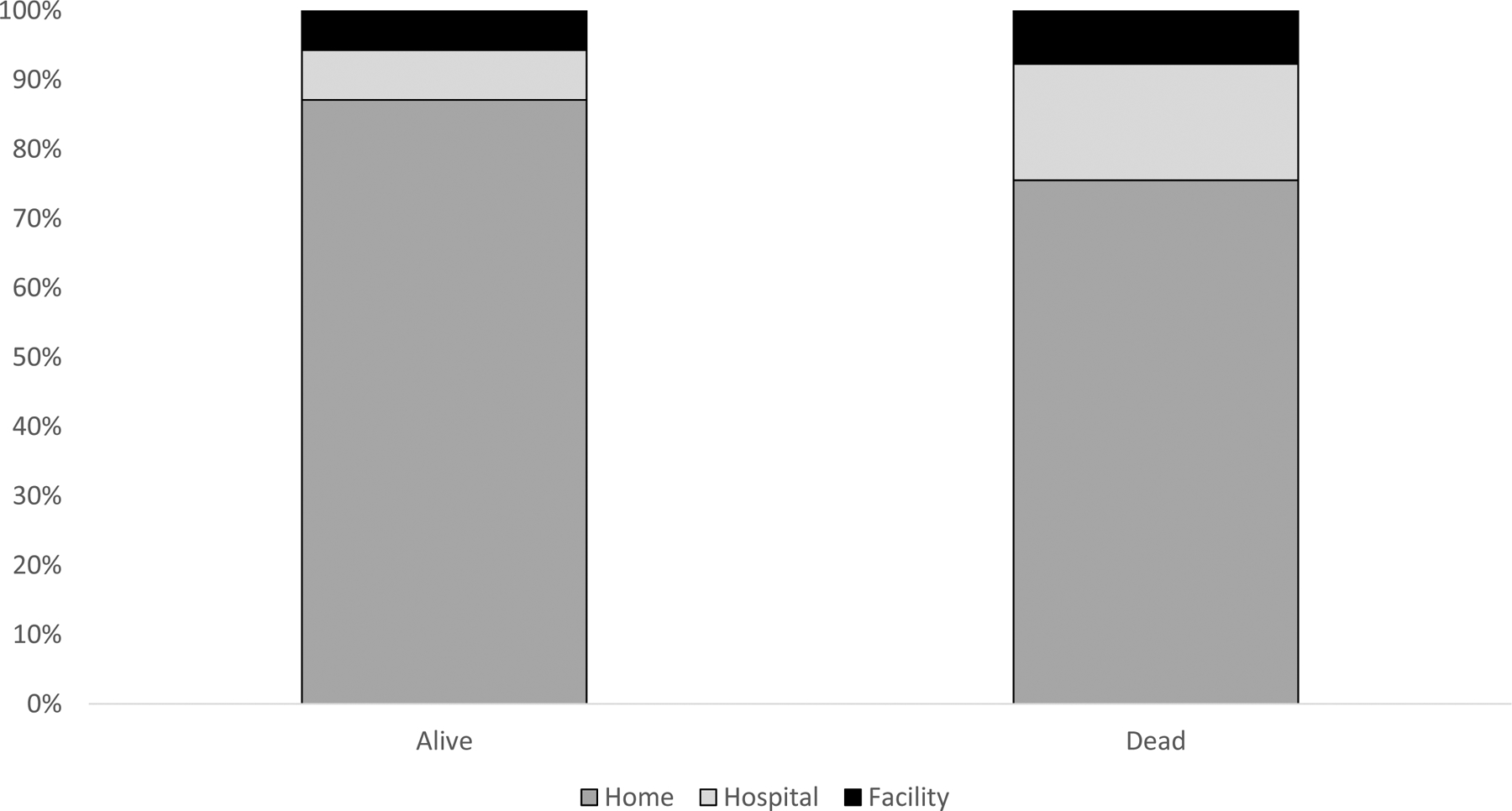
Percentage of time spent at home, in the hospital and in a facility during the year following major cancer surgery. Data are adjusted for procedure type, age, gender, race, Charlson Score, and calendar year.
Table 2 shows results for a model depicting the relative risk of subjects who died within 1 year following surgery. Increased relative risk of death at 1-year was associated with having a pancreaticoduodenectomy [adjusted RR 1.25 (95% CI 1.20–1.30)] or a cystectomy [aRR 1.15 (95% CI 1.10–1.20)] compared to a gastrectomy, with older age [aRR 1.11 (95% CI 1.06–1.16) for ages 75–79, aRR 1.20 (95% CI 1.14–1.26) for ages 80–85, and aRR 1.31 (95% CI 1.24–1.39) for ages ≥85 years, all compared to ages 65–69], with black race [aRR 1.07 (95% CI 1.02–1.13), compared to white race], with increasing Charlson Comorbidity Index score [aRR 1.36 (95% CI 1.31–1.41) for scores 2–3, aRR 1.59 (95% CI 1.50–1.68) for scores >4, compared to scores 0–1], with longer hospital length of stay during the index hospitalization [aRR 1.24 (95% CI 1.17–1.31) for 9–13 days, aRR 1.57 (95% CI 1.49–1.65) for ≥14 days, compared to 1–6 days], and with those who were discharged to a facility rather than to home [aRR 1.77 (95% CI 1.71–1.83)]. Female gender [aRR 0.91 (95% CI 0.88–0.94)] and race other than white or black [aRR 0.88 (0.82–0.94)] were associated with decreased risk of death within one year following surgery.
Table 2.
Risk factor analysis of mortality within 12 months. Adjusted for calendar year.
| Basic Statistics | Univariate Model RR | Multivariate Model RR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Observed N=37748 | Subject Deaths n=10700 | P | RR & 95% CI | P | Global P | RR & 95% CI | P | Global P |
| Type of surgery/procedure | |||||||||
| Gastrectomy | 9791 (25.9) | 2689 (27.5) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| Cystectomy | 14294 (37.9) | 3723 (26.0) | 0.95 (0.91 – 0.99) | 0.0143 | 1.15 (1.10 – 1.20) | <.0001 | |||
| Pancreaticoduodenectomy | 10845 (28.7) | 3546 (32.7) | 1.19 (1.14 – 1.24) | <.0001 | 1.25 (1.20 – 1.30) | <.0001 | |||
| Esophagectomy | 2818 (7.5) | 742 (26.3) | 0.96 (0.89 – 1.03) | 0.2357 | 0.96 (0.89 – 1.03) | 0.2136 | |||
| Age (years) | |||||||||
| 65–69 | 11448 (30.3) | 2725 (23.8) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| 70–74 | 8304 (22.0) | 2162 (26.0) | 1.09 (1.04 – 1.15) | 0.0003 | 1.05 (1.00 – 1.10) | 0.0500 | |||
| 75–79 | 9133 (24.2) | 2648 (29.0) | 1.22 (1.16 – 1.28) | <.0001 | 1.11 (1.06 – 1.16) | <.0001 | |||
| 80–84 | 6035 (16.0) | 2041 (33.8) | 1.42 (1.35 – 1.49) | <.0001 | 1.20 (1.14 – 1.26) | <.0001 | |||
| ≥85 | 2828 (7.5) | 1124 (39.7) | 1.67 (1.58 – 1.77) | <.0001 | 1.31 (1.24 – 1.39) | <.0001 | |||
| Gender | |||||||||
| Male | 25021 (66.3) | 7067 (28.2) | 0.5391 | Ref. | 0.5396 | Ref. | <.0001 | ||
| Female | 12727 (33.7) | 3633 (28.5) | 1.01 (0.98 – 1.05) | 0.5389 | 0.91 (0.88 – 0.94) | <.0001 | |||
| Race | |||||||||
| White | 31778 (84.2) | 8996 (28.3) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| Black | 3314 (8.8) | 1066 (32.2) | 1.14 (1.08 – 1.20) | <.0001 | 1.07 (1.02 – 1.13) | 0.0063 | |||
| Other | 2656 (7.0) | 638 (24.0) | 0.85 (0.79 – 0.91) | <.0001 | 0.88 (0.82 – 0.94) | 0.0002 | |||
| Charlson Comorbidity Index Score | |||||||||
| 0 to 1 | 17525 (46.4) | 3905 (22.3) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| 2 to 3 | 17831 (47.2) | 5752 (32.3) | 1.45 (1.40 – 1.50) | <.0001 | 1.36 (1.31 – 1.41) | <.0001 | |||
| >4 | 2392 (6.3) | 1043 (43.6) | 1.96 (1.86 – 2.06) | <.0001 | 1.59 (1.50 – 1.68) | <.0001 | |||
| Hospital length of stay (days) | |||||||||
| 1–6 | 7619 (20.2) | 1494 (19.6) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| 7–8 | 9458 (25.1) | 2073 (21.9) | 1.12 (1.05 – 1.19) | 0.0002 | 1.06 (1.00 – 1.12) | 0.0565 | |||
| 9–13 | 10360 (27.4) | 2853 (27.5) | 1.40 (1.33 – 1.48) | <.0001 | 1.24 (1.17 – 1.31) | <.0001 | |||
| ≥14 | 10311 (27.3) | 4280 (41.5) | 2.12 (2.01 – 2.23) | <.0001 | 1.57 (1.49 – 1.65) | <.0001 | |||
| Discharge disposition | |||||||||
| Home (no assistance) | 28166 (74.6) | 6157 (21.9) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| Facility (SNF, Hospice, Inpatient) | 9582 (25.4) | 4543 (47.4) | 2.17 (2.10 – 2.24) | <.0001 | 1.77 (1.71 – 1.83) | <.0001 | |||
Since discharge to a facility was strongly associated with increased risk of death in the year following surgery, we decided to look more closely into which factors were associated with this finding. Table 3 shows the results of a model predicting relative risk of discharge to a facility following high-risk cancer surgery. Increased relative risk of this outcome was associated with having a cystectomy [aRR 1.52 (95% CI 1.44–1.60)], esophagectomy [aRR 1.27 (95% CI 1.17–1.39)], or pancreaticoduodenectomy [aRR 1.15 (95% CI 1.09–1.21)], compared to a gastrectomy, with older age [aRR 1.27 (95% CI 1.18–1.36) for ages 70–74, aRR 1.76 (95% CI 1.65–1.87) for ages 75–79, aRR 2.27 (95% CI 2.13–2.41) for ages 80–85, and aRR 2.75 (95% CI 2.57–2.95) for ages ≥ 85 years, compared to ages 65–69], with female gender [aRR 1.40 (95% CI 1.34–1.46)], with black race [aRR 1.09 (95% CI 1.02–1.16)], with increasing Charlson Comorbidity Index score [aRR 1.37 (95% CI 1.30–1.43) for scores of 2–3, aRR 2.40 (95% CI 2.26–2.55) for scores >4 compared to scores of 0–1], and with increasing length of hospital stay [aRR 1.58 (95% CI 1.46–1.72) for 7–8 days, 2.00 (95% CI 1.85–2.16) for 9–13 days, and aRR 2.81 (95% CI 2.60–3.02) for ≥ 14 days, compared to 1–6 days].
Table 3.
Risk factor analysis of discharge to a facility. Adjusted for calendar year.
| Basic Statistics | Univariate Model RR | Multivariate Model RR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Entire Cohort N=37748 | Discharged n=7416 | P | RR & 95% CI | P | Global P | RR & 95% CI | P | Global P |
| Type of surgery/procedure | |||||||||
| Gastrectomy | 9791 (25.9) | 1861 (19.0) | 0.1184 | Ref. | 0.1148 | Ref. | <.0001 | ||
| Cystectomy | 14294 (37.9) | 2843 (19.9) | 1.05 (0.99 – 1.10) | 0.0902 | 1.52 (1.44 – 1.60) | <.0001 | |||
| Pancreaticoduodenectomy | 10845 (28.7) | 2182 (20.1) | 1.06 (1.00 – 1.12) | 0.0445 | 1.15 (1.09 – 1.21) | <.0001 | |||
| Esophagectomy | 2818 (7.5) | 530 (18.8) | 0.99 (0.91 – 1.08) | 0.8119 | 1.27 (1.17 – 1.39) | <.0001 | |||
| Age (years) | |||||||||
| 65–69 | 11448 (30.3) | 1373 (12.0) | Ref. | <.0001 | Ref. | <.0001 | |||
| 70–74 | 8304 (22.0) | 1281 (15.4) | 1.29 (1.20 – 1.38) | <.0001 | 1.27 (1.18 – 1.36) | <.0001 | |||
| 75–79 | 9133 (24.2) | 2004 (21.9) | 1.83 (1.72 – 1.95) | <.0001 | 1.76 (1.65 – 1.87) | <.0001 | |||
| 80–84 | 6035 (16.0) | 1734 (28.7) | 2.40 (2.25 – 2.55) | <.0001 | 2.27 (2.13 – 2.41) | <.0001 | |||
| ≥85 | 2828 (7.5) | 1024 (36.2) | 3.02 (2.82 – 3.24) | <.0001 | 2.75 (2.57 – 2.95) | <.0001 | |||
| Gender | |||||||||
| Male | 25021 (66.3) | 4372 (17.5) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| Female | 12727 (33.7) | 3044 (23.9) | 1.37 (1.31 – 1.43) | <.0001 | 1.40 (1.34 – 1.46) | <.0001 | |||
| Race | |||||||||
| White | 31778 (84.2) | 6185 (19.5) | <.0001 | Ref. | <.0001 | Ref. | 0.0331 | ||
| Black | 3314 (8.8) | 749 (22.6) | 1.16 (1.09 – 1.24) | <.0001 | 1.09 (1.02 – 1.16) | 0.0130 | |||
| Other | 2656 (7.0) | 482 (18.1) | 0.93 (0.86 – 1.01) | 0.1017 | 0.97 (0.90 – 1.05) | 0.4802 | |||
| Charlson Comorbidity Index Score | |||||||||
| 0 to 1 | 17525 (46.4) | 2656 (15.2) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| 2 to 3 | 17831 (47.2) | 3715 (20.8) | 1.37 (1.31 – 1.44) | <.0001 | 1.37 (1.30 – 1.43) | <.0001 | |||
| >4 | 2392 (6.3) | 1045 (43.7) | 2.88 (2.72 – 3.05) | <.0001 | 2.40 (2.26 – 2.55) | <.0001 | |||
| Hospital length of stay (days) | |||||||||
| 1–6 | 7619 (20.2) | 716 (9.4) | <.0001 | Ref. | <.0001 | Ref. | <.0001 | ||
| 7–8 | 9458 (25.1) | 1488 (15.7) | 1.67 (1.54 – 1.82) | <.0001 | 1.58 (1.46 – 1.72) | <.0001 | |||
| 9–13 | 10360 (27.4) | 2103 (20.3) | 2.16 (2.00 – 2.34) | <.0001 | 2.00 (1.85 – 2.16) | <.0001 | |||
| ≥14 | 10311 (27.3) | 3109 (30.2) | 3.21 (2.97 – 3.46) | <.0001 | 2.81 (2.60 – 3.02) | <.0001 | |||
Figure 2 illustrates the percentage of days spent at home, in the hospital and in a facility in the year following surgery based on whether or not subjects who were dead at one year were discharged to a facility or discharged home following the index surgery. Subjects who were discharged to a facility spent 61.4% (compared to 86.7%) of their time in the year following surgery at home. Additionally, they spent 25.5% of their time in the hospital (compared to 10.0%) and 13.1% of their time in a facility (compared to 3.3%).
Figure 2.
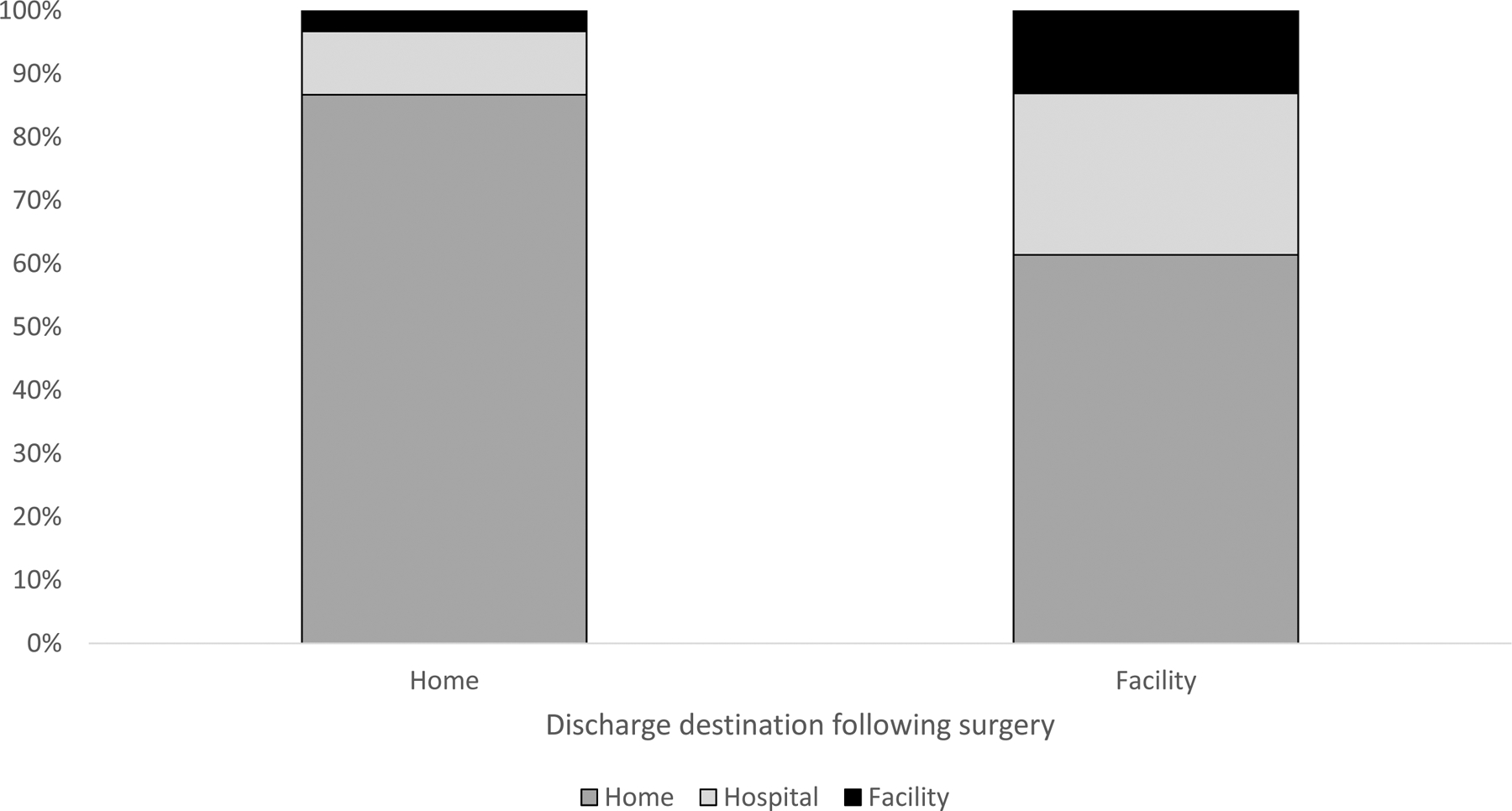
Percentage of time spent at home, in the hospital and in a facility during the year following major cancer surgery among individuals who died during this period. Data are stratified by discharge destination (i.e., to home or to a facility) and are adjusted for procedure type, age, gender, race, Charlson Score, and calendar year.
Discussion
Among Medicare beneficiaries undergoing high-risk cancer surgery, the time spent away from home (i.e., in the hospital or in a facility) in the year following surgery is high −13% among beneficiaries who were alive at 1-year after surgery and 25% among beneficiaries who died in the year following surgery. Discharge to a facility, among other predictors, was associated with an increased relative risk of death during the year after surgery, and beneficiaries who were discharged to facility and who died in the year following surgery ended up spending, on average, 39% of their final year of life in the hospital and/or in a facility.
The existing literature is mainly limited to 30-day readmissions and to initial hospital discharge destination following these high-risk cancer surgeries. One study using data from the Healthcare Cost and Utilization Project’s State Impatient Database (HCUP-SID) examined patients undergoing similarly high-risk abdominal surgery (including open abdominal aortic aneurysm repair, cystectomy, esophagectomy, and pancreatectomy) and found that 19.4% of patients were discharged to a skilled nursing facility,3 which is similar to the rate of 22.8% found in this study. Another study looked at 30-day readmission intensity in cystectomy patients using Surveillance, Epidemiology, and End Results (SEER)-Medicare data and found that 77% of readmissions occurred within the first week of discharge.15 This study, however, was limited to 30 days of follow up, and therefore, was not able to assess readmissions over the course of the year following surgery, as was done in our study. Thirty-day readmission rates have been extensively studied and have been found to range from 13–19% across all types of high-risk cancer surgery included in this study.4,5,7,8
Our study is novel in its aim to document the amount of time spent away from home (i.e., in a hospital and/or in a facility) for the entire year following surgery. We found that regardless of whether a patient survived this crucial year, that they spent considerable amount of time in a setting other than their home. This was most notable among beneficiaries who were initially discharged to a facility and who died within one year of surgery. This subset of the population, on average, spent 39% of their time away from their homes: 25.5% in a hospital and 13.1% in a facility. Beneficiaries who were alive at one year spent 12.9% of their time away from their homes: 7.2% in the hospital and 5.7% in a facility. Therefore, even those beneficiaries who lived at least the full year after surgery ended up spending almost 13% of this year (beyond the time of their initial surgical admission) in some type of institution. Overall, patients undergoing high-risk cancer surgery had 1.5 ± 2.0 hospital readmissions, spent 13.9 ± 26.2 days in the hospital, had 1.5 ± 1.0 admissions to a facility and spent 37.2 ± 50.6 days in a facility in the year after surgery. These data are novel and important to consider when counseling patients and setting expectations for surgical recovery.
This study should be interpreted with certain limitations in mind. First, based on the limitations associated with using Medicare claims data, we are limited in our understanding of the causes, intensity, and severity related to the time spent in the hospital and other facilities. However, our goal in this study was to gain a better understanding of the amount of time spent in each setting, therefore, our outcomes are informative on their own. Second, we did not evaluate patients who had like cancer diagnoses and did not undergo surgery. This level of analysis was not possible using the Inpatient data files that we had, therefore, we cannot determine how patients undergoing these types of high-risk surgeries may or may not differ compared to similar patients who did not undergo surgery due to overall health status, cancer stage or extent or patient preference. A different study looking at these patients would be necessary to draw any conclusions regarding difference or similarities between these groups.
Conclusions
Our findings indicate that Medicare beneficiaries spend a significant amount of time living in settings other their homes (i.e., in the hospital or in a nursing facility) in the year following high-risk cancer surgery. These findings provide new and important information to patients, their families and physicians that go far beyond 30-day outcomes, indicating that the post-operative course may be long and arduous for many older individuals. This information is important in counseling patients and families to help guide realistic expectations following surgery.
Supplementary Material
Acknowledgments
Anne M. Suskind receives funding from the National Institute on Aging (NIH-NIA R01AG058616-01)
Emily Finlayson receives funding from the National Institute on Aging (R01AG04425, R21AG054208, P30AG44281) of the National Institutes of Health and the Patient Centered Outcomes Research Institute (1502-27462), and is a founding shareholder of Ooney, Inc.
References
- 1.Taub DA, Dunn RL, Miller DC, Wei JT, Hollenbeck BK. Discharge practice patterns following cystectomy for bladder cancer: evidence for the shifting of the burden of care. The Journal of urology. 2006;176(6 Pt 1):2612–2617; discussion 2617–2618. [DOI] [PubMed] [Google Scholar]
- 2.Mahvi DA, Pak LM, Urman RD, Gold JS, Whang EE. Discharge destination following pancreaticoduodenectomy: A NSQIP analysis of predictive factors and post-discharge outcomes. American journal of surgery. 2018. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs BL, He C, Li BY, et al. Variation in readmission expenditures after high-risk surgery. The Journal of surgical research. 2017;213:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acher AW, Squires MH, Fields RC, et al. Readmission Following Gastric Cancer Resection: Risk Factors and Survival. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2016;20(7):1284–1294. [DOI] [PubMed] [Google Scholar]
- 5.Ammori JB, Navale S, Schiltz N, Koroukian SM. Predictors of 30-day readmissions after gastrectomy for malignancy. The Journal of surgical research. 2018;224:176–184. [DOI] [PubMed] [Google Scholar]
- 6.Rosemurgy AS, Luberice K, Paul H, et al. Readmissions after pancreaticoduodenectomy: efforts need to focus on patient expectations and nonhospital medical care. The American surgeon. 2012;78(8):837–843. [PubMed] [Google Scholar]
- 7.Sutton JM, Wilson GC, Wima K, et al. Readmission After Pancreaticoduodenectomy: The Influence of the Volume Effect Beyond Mortality. Annals of surgical oncology. 2015;22(12):3785–3792. [DOI] [PubMed] [Google Scholar]
- 8.Zafar SN, Shah AA, Nembhard C, et al. Readmissions After Complex Cancer Surgery: Analysis of the Nationwide Readmissions Database. Journal of oncology practice / American Society of Clinical Oncology. 2018;14(6):e335–e345. [DOI] [PubMed] [Google Scholar]
- 9.Chen SY, Molena D, Stem M, Mungo B, Lidor AO. Post-discharge complications after esophagectomy account for high readmission rates. World J Gastroenterol. 2016;22(22):5246–5253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nassour I, Wang SC, Porembka MR, et al. Robotic Versus Laparoscopic Pancreaticoduodenectomy: a NSQIP Analysis. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2017;21(11):1784–1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lavallee LT, Schramm D, Witiuk K, et al. Peri-operative morbidity associated with radical cystectomy in a multicenter database of community and academic hospitals. PloS one. 2014;9(10):e111281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamilton TD, Mahar AL, Haas B, et al. The impact of advanced age on short-term outcomes following gastric cancer resection: an ACS-NSQIP analysis. Gastric Cancer. 2018;21(4):710–719. [DOI] [PubMed] [Google Scholar]
- 13.Liu JB, Berian JR, Liu Y, Ko CY, Weber SM. Trends in perioperative outcomes of hospitals performing major cancer surgery. J Surg Oncol. 2018;118(4):694–703. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of clinical epidemiology. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 15.Skolarus TA, Jacobs BL, Schroeck FR, et al. Understanding hospital readmission intensity after radical cystectomy. The Journal of urology. 2015;193(5):1500–1506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


