Abstract
Trazodone is a serotonin receptor antagonist and reuptake inhibitor used extensively as an anxiolytic in human and small animal veterinary medicine. The aims of this study were to determine the pharmacokinetics of oral trazodone in experimental horses and to evaluate the effect of oral trazodone in clinical horses. Six experimental horses were administered trazodone at 7.5 or 10 mg/kg. Plasma concentrations of trazodone and its metabolite (m‐CPP) were determined via UPLC‐MS/MS. Noncompartmental pharmacokinetic analysis, sedation and ataxia scores were determined. Trazodone was rapidly absorbed after oral administration with a maximum concentration of 2.5–4.1 μg/ml and half‐life of the terminal phase of approximately 7 hr. The metabolite was present at low levels in all horses, representing only 2.5% of the total area under the curve. In experimental horses, concentration‐dependent sedation and ataxia were noted, lasting up to 12 hr. For clinical cases, medical records of horses treated with trazodone for various abnormal behaviours were reviewed and data were summarized. Trazodone was successful in modifying behavioural problems to some degree in 17 of 18 clinical cases. Tolerance and subsequent lack of drug effect occurred in two of 18 clinical cases following 14 or 21 days of use. In both populations of horses, adverse effects attributed to trazodone include oversedation, muscle fasciculations and transient arrhythmias.
Keywords: adverse drug reaction, equine, sedative, serotonin antagonist and reuptake inhibitor
1. INTRODUCTION
Stall rest is prescribed for many horses following orthopaedic injuries, surgeries and severe illness. Some horses do not tolerate confinement well, due to temperament issues, separation or situational anxiety or a lack of acclimation. These horses may walk incessantly, weave, crib, rear, buck or kick the stall walls. These behaviour problems may contribute to delayed wound healing, new injury, recrudescence of illness, as well as damage to the stall and distress for owners. Management techniques such as environmental or social enrichment and free choice access to feed are often attempted, but may not be successful or appropriate for all cases. Herbal and supplemental calming products are available, using various amino acids as well as magnesium for effect; however, there is little scientific data available to judge these products and they are not always effective. If environmental enrichment and supplemental calming agents do not work, medications are often tried. Of these, the most commonly used agents are acepromazine, fluphenazine and reserpine, all of which carry an unacceptable risk of adverse events. The adverse effects ascribed to these drugs make it necessary to find a safer alternative for management of stall rest.
Trazodone hydrochloride is a triazolopyridine derivative and member of the phenylpiperazine class of drugs. It is classified as a serotonin antagonist and reuptake inhibitor based on its primary pharmacologic mechanism of action to antagonize serotonin 2A receptors and its secondary mechanism to inhibit serotonin reuptake (Stahl, 2013). Trazodone and its active metabolite, m‐chlorophenylpiperazine (m‐CPP), also have agonistic effects at serotonin 1 receptors (Odagaki, Toyoshima, & Yamauchi, 2005). Trazodone has been used extensively in small animal medicine as an anxiolytic, with or without other behaviour modifying drugs (Gruen & Sherman, 2008; Orlando, Case, Thomson, Griffith, & Sherman, 2016; Stevens et al., 2016). The successful use of this drug in other veterinary species makes it an attractive alternative for use in horses, and worthy of study in this species, as a reduction in anxiety in stall‐rested horses will improve animal welfare.
Currently, there is one published report on trazodone in adult horses (Knych, Mama, Steffey, Stanley, & Kass, 2017); however, there are no published reports of the use of this drug in clinical cases. Therefore, the objectives of this study were to determine the pharmacokinetics of trazodone and its active metabolite in this species following a single oral dose of 10 and 7.5 mg/kg as well as to determine whether administration results in sedation, ataxia or other adverse effects. Finally, the use of daily trazodone in clinical patients presenting to a veterinary teaching hospital is reported.
2. MATERIALS AND METHODS
2.1. Experimental cases
2.1.1. Animals
Six healthy adult geldings aged 6–12 years and weighing between 481 and 651 kg were used in the study. Breeds included four Quarter Horses and two appendix Quarter Horses. Horses were housed in stables beginning the day prior to drug administration and for the duration of the study. Water and grass hay were available ad libitum throughout the study, with the exception that hay was withheld for 1 hr before and 2 hr after drug administration. This study was approved by the North Carolina State University Institutional Animal Care and Use Committee (Protocol #15‐079‐O), and all ethical and legal requirements were followed.
2.1.2. Pharmacodynamic data
Physiologic data (heart rate, respiratory rate, body temperature, mucous membrane colour and capillary refill time) were recorded prior to drug administration, 30 min and 1, 2, 4, 6, 8, 12 and 24 hr postadministration. Gastrointestinal sounds were evaluated by auscultation of the dorsal and ventral quadrants on both sides and scored as present or absent in each quadrant to assign a GI motility score that ranged from 0 to 4 at each time point. Auscultation was performed over a period of up to 30 s per quadrant. Faecal output and time to first faecal production were recorded. Horses were also monitored for adverse effects including signs of colic (rolling, flank watching, excessive pawing and stretching out) or other abnormal behaviours.
Sedation and ataxia scores were determined using scoring systems adapted from the literature (Solano, Valverde, Desrochers, Nykamp, & Boure, 2009; Wojtasiak‐Wypart et al., 2012; Wong et al., 2015). Scoring was performed at time points corresponding with physical examinations. In general, physical examinations were performed prior to blood collection and sedation and ataxia scores were performed after blood collection when those time points coincided. Sedation scores were assigned as described in Table 1. Ataxia scoring was graded as follows: 0 = none; 1 = stable and swaying slightly; 2 = swaying and leaning; and 3 = swaying, leaning, crossing limbs and buckling. For all horses, the baseline score was determined to be zero for both scoring systems.
Table 1.
Criteria used for assigning sedation scores in horses following trazodone administration
| Sedation scoring table | |
|---|---|
| Score | Description |
| 0 | No sedation |
| 1 | Mild sedation (slightly decreased frequency and velocity of movement, lower ear and neck carriage, slight base‐wide stance) |
| 2 | Moderate sedation (moderately decreased frequency and velocity of movement, obvious ear tip separation, increased base‐wide stance, crossed legs, buckled knees/fetlocks) |
| 3 | Deep sedation (markedly decreased frequency and velocity of movement, pronounced ear tip separation, markedly low neck carriage, markedly increased base‐wide stance, increased occurrence and severity of crossed legs, buckled knees and/or fetlocks) |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
2.1.3. Drug administration
By use of a randomized, two‐way crossover design, trazodone hydrochloride in the form of commercially available 100 mg tablets (Teva Pharmaceuticals, Sellersville, PA, USA) was administered orally. Three horses (horses A–C) were randomly assigned to receive the 10 mg/kg dose first, followed by the 7.5 mg/kg dose. The other three horses (horses D–F) received 7.5 mg/kg first, followed by 10 mg/kg. Doses were rounded to the nearest complete tablet, and actual doses ranged between 9.98–10.03 and 7.43–7.55 mg/kg for the high and low dose, respectively. A minimum 2‐week washout period was allowed between administrations. To administer the drug, the dose was divided into two 60‐ml catheter tip syringes and the tablets were dissolved in 40 cc of warm water for 5 min. Light corn syrup (15 ml) was then added to increase viscosity and palatability. The resulting suspension was then administered orally through the interdental space and the horse's head elevated for 1 min to ensure administration of the entire dose. Oral administration was achieved within 15 min after tablet contents were mixed with corn syrup.
2.1.4. Collection of blood samples
Blood samples were collected via an indwelling catheter inserted in the jugular vein. For placement of the jugular catheters, a small area over the jugular vein was clipped and aseptically prepared. The skin and subcutaneous tissue was anesthetized with 2% lidocaine hydrochloride. The catheter (14 gauge, 5 ¼ inch; Mila International, Inc, Florence, KY, USA) was then placed and sutured in position, along with an extension set. Samples were collected at time 0 (before treatment), 10, 20, 30 and 45 min and 1, 1.5, 2, 4, 6, 8, 12, 24, 36 and 48 hr after oral administration. Additional samples were collected by venipuncture from the cephalic vein at 1 and 4 hr (n = 3 at each time point) to determine the effect of sample site on plasma concentrations. Waste blood (10 ml) was aspirated from the intravenous jugular catheter into a syringe and then discarded. The blood sample (6 ml) was then collected and immediately placed in lithium heparin‐containing plastic blood tubes. After each sample collection, the catheter was flushed with 10 ml of heparinized saline. Plasma samples were centrifuged at 3,500 rpm (1,400 × g) for 10 min, and the plasma was then separated into 2 ml cryogenic storage tubes. All samples were stored at −80°C until analysis. Plasma samples were stored between 4 and 11 months prior to analysis. The long‐term stability of trazodone and m‐CPP has been described in prior publications (Kale, Agrawal, Gupta, Patel, & Patel, 2014; Li‐Bo et al., 2014).
2.1.5. Chromatographic assay
The concentrations of trazodone and its metabolite m‐CPP were determined by ultra‐high pressure liquid chromatography with tandem mass spectrometry using a method validated in our laboratory for equine plasma. Calibration curves were prepared daily by fortifying blank equine plasma with stock solutions of trazodone and m‐CPP (Sigma‐Aldrich Corp., St. Louis, MO, USA) dissolved in methanol at a concentration of 1 mg/ml each, then further diluted in a solution of 50% acetonitrile (ACN) and 50% double distilled water (ddH2O). Plasma samples and standards were prepared identically by placing 200 μl of plasma into a glass tube and adding 200 μl of 2% ammonium hydroxide in water and vortexing for 10 s. The sample or standard was then transferred to a 1 ml supported liquid extraction cartridge (Isolute SLE+; Biotage, LLC, Charlotte, NC, USA) attached to a vacuum manifold. A short period of vacuum was applied to initiate absorption, and then, the cartridges were allowed to sit for 5 min. Next, 2.5 ml of methyl tert‐butyl ether was applied to the cartridge and allowed to sit for 5 min without vacuum followed by light vacuum for 2 min. This process was repeated and the vacuum was applied until complete elution of the sample. The eluate was then evaporated under a stream of compressed nitrogen for 15 min at 45°C. The samples and standards were then reconstituted using 200 μl of 50/50 ACN:ddH2O (v/v). From this point, the samples and standards were further diluted accordingly to produce concentrations within a high and low concentration standard curve. The high concentration standard curve was prepared by adding 5 μl sample to 400 μl 50/50 ACN:ddH2O (v/v) and was used for concentrations of trazodone between 0.01 and 10 μg/ml. The low concentration standard curve was prepared by adding 100 μl sample to 250 μl 50/50 ACN:ddH2O (v/v) and was used for concentrations of trazodone and m‐CPP between 0.001 and 0.5 μg/ml. The two standard curves were used to accommodate the wide range of concentrations in the samples, the low concentrations of the metabolite and to increase the sensitivity of the assay.
Volumes of 2 μl for samples and standards were injected on an I Class Acquity UPLC with a Xevo/TQD mass spectrometer (Waters Corporation, Milford, ME, USA). The initial mobile phase consisted of formic acid (0.1%) in water (Solution A) and formic acid (0.1%) in acetonitrile (Solution B). Initial conditions were set at 90% Solution A and 10% Solution B from 0 to 3 min followed by 10% Solution A and 90% Solution B from 3 to 4 min and then returned to initial conditions from 4 to 5 min. Mobile phase was run at a rate of 0.4 ml/min. Separation was achieved using an Acquity UPLC BEH phenyl column (1.7 μm, 2.1 × 100 mm) and corresponding VanGuard Pre‐column (130 Å, 1.7 μm, 2.1 × 5 mm) (Waters Corporation, Milford, ME, USA). The column and samples were maintained at 40°C and 10°C, respectively. The collision and desolvation gases used were argon and nitrogen, respectively. Trazodone and m‐CPP were quantified using a single mass transition in the positive ion mode of 372.25 → 179.01 for trazodone and 197.17 → 118.01 for m‐CPP.
Assay validation and quality assurance were performed according to published guidelines (Shah, Midha, & Dighe, 1992). Calibration curves were prepared and analysed daily using six calibration samples and a blank (unfortified) sample. For the calibration curve to be deemed acceptable, the coefficient of determination (R 2) value was >.99 and calibration standards back‐calculated to within 15% of the true value. Blank samples from each animal were analysed to ensure selectivity of the assay. Accuracy is reported as the % deviation from the true value, and precision was measured as the % deviation about the mean. Accuracy and precision were deemed acceptable if values were less than 15% for each concentration used. The lower limit of detection (LLOD) and lower limit of quantitation (LLOQ) are reported as the lowest concentration detected or quantifiable on the calibration curve, respectively. The overall LLOQ for trazodone was 0.001 μg/ml and the LLOD was 0.0005 μg/ml. The intraday accuracy and precision of the assay were determined in quality control (QC) samples using spiked equine plasma at 5 concentrations representing a high, medium and low concentration over the range of the high and low calibration curve. For trazodone, the accuracy was within 4.52 ± 3.85% of the true value, and precision was within 6.65 ± 5.74% of the mean for concentrations of 2.5, 1, 0.1, 0.01 and 0.005 μg/ml. For the metabolite, m‐CPP, the LLOQ was 0.005 μg/ml and the LLOD was 0.001 μg/ml. The intraday accuracy and precision of the assay were determined at three concentrations over the range of the low standard curve. For m‐CPP, the accuracy was within 5.75 ± 5.32% of the true value, and precision was within 6.73 ± 4.82% of the mean for concentrations of 0.1, 0.01 and 0.005 μg/ml.
2.1.6. Data analysis
Drug concentrations were analysed using commercially available software (Phoenix® WinNonlin® version 6.3; Certara USA, Inc., Princeton, NJ, USA) to determine pharmacokinetic parameters for each horse. Noncompartmental analysis was used to determine the maximum plasma concentration (C max), time to C max (T max), terminal rate constant (λz), half‐life of the terminal phase (t½λ) and total area under the curve (AUC) of trazodone and m‐CPP following oral administration.
2.1.7. Statistical analysis
Statistical analysis was performed using commercially available software (SigmaPlot 12.0; Systat Software, Inc., San Jose, CA, USA). For all data, normality was assessed using the Shapiro–Wilk and equal variance tests. Changes in normally distributed data, including heart rate, respiratory rate and temperature (for 10 mg/kg dose), as well as differences in sedation and ataxia scores between dose levels, were analysed using one‐way repeated measures analysis of variance (RM‐ANOVA). Changes in non‐normally distributed data, including gastrointestinal sounds and temperature (for 7.5 mg/kg dose), as well as differences in sedation and ataxia scores compared to baseline, were analysed using Friedman's RM_ANOVA on ranks. Linear regression analysis was used to determine the relation between the combined (trazodone and m‐CPP) plasma concentrations and effect based on sedation and ataxia scores. Paired t tests were used to determine differences in normally distributed data, including pharmacokinetic parameters (C max, AUC, t½λ) for trazodone and its metabolite between the 10 and 7.5 mg/kg dose groups, as well as differences between jugular and cephalic drug concentrations, time to first defecation and total number of faecal piles in the first 24 hr. For non‐normally distributed data (T max), the Mann–Whitney rank sum test was used to analyse the difference between dose groups. Statistical significance was set at a p value ≤.05.
2.2. Clinical cases
Medical records from horses presenting to the Veterinary Teaching Hospital and prescribed trazodone were searched to determine clinical safety and efficacy. Data collected included signalment, presenting complaint, number of days on trazodone, doses used, usage of concurrent reserpine and any adverse effects attributed to trazodone administration. Response to trazodone was classified as satisfactory or unsatisfactory based on the assessment of the treating clinician.
3. RESULTS
3.1. Pharmacokinetics
The plasma concentrations over time of trazodone and m‐CPP are depicted in Figure 1a,b. Trazodone was detected in the plasma of all horses 10 min after oral administration of either 7.5 or 10 mg/kg and reached maximum concentrations between 10 and 45 min. The metabolite, m‐CPP, was detectable in 3/6 horses at 10 min, and all horses by 20 min following administration of either 7.5 or 10 mg/kg and reached maximum concentrations between 20 and 60 min. The metabolite was prepared by all horses, although it was present in low amounts, representing only 2.55 ± 1.41% of the total AUC of trazodone plus metabolite. No significant difference between plasma concentration was noted between the blood collection sites (p = .82). The half‐life of the terminal phase (t½λ) of trazodone was moderate at approximately 7 hr and was not affected by dose. The t½λ of m‐CPP was more variable, with an average of approximately 4 hr for the 7.5 mg/kg and 6.8 hr for 10 mg/kg. Other relevant pharmacokinetic parameters are summarized in Tables 2 and 3. For trazodone, no significant difference between t½λ and T max was detected between dose groups. A trend towards a higher C max was noted in the 10 mg/kg dose group compared to the 7.5 mg/kg group (p = .0621). A significant difference was detected between the AUC for the 10 mg/kg dose group and the 7.5 mg/kg dose group (p = .0482). No significant differences were detected for any pharmacokinetic parameters for m‐CPP.
Figure 1.
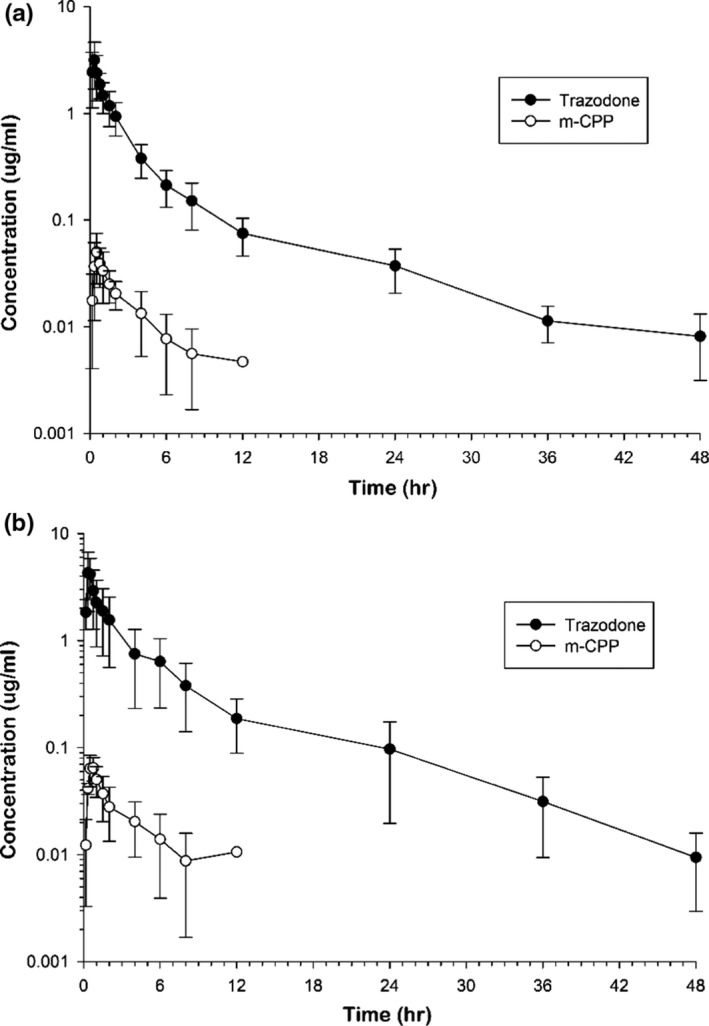
Plasma trazodone and m‐CPP concentrations in horses (n = 6) after a single oral dose of trazodone hydrochloride at either 7.5 mg/kg (a) or 10 mg/kg (b)
Table 2.
Noncompartmental pharmacokinetic parameters for trazodone following administration of 7.5 or 10 mg/kg orally to six horses
| Pharmacokinetic Variable | 7.5 mg/kg Mean ± SD | 10 mg/kg Mean ± SD |
|---|---|---|
| T max (hr) | 0.37 ± 0.20 | 0.42 ± 0.09 |
| C max (μg/ml) | 2.45 ± 0.79 | 4.07 ± 2.23 |
| AUC0–∞ (μg*hr/ml)a | 5.77 ± 1.929 | 11.42 ± 7.30 |
| AUC0–∞ (% extrap) | 1.20 ± 0.73 | 1.21 ± 1.63 |
| AUMC (hr*hr*μg/ml) | 35.09 ± 27.96 | 86.39 ± 70.23 |
| λ (hr−1) | 0.093 ± 0.025b | 0.10 ± 0.02 |
| t 1/2λ (hr) | 7.86 ± 1.76b | 7.19 ± 1.84 |
T max, time to maximum concentration; C max, maximum concentration; AUC, area under the concentration–time curve; AUMC, area under the first moment–time curve; λ, slope of the terminal phase; t 1/2λ, half‐life of terminal phase.
Statistical difference detected between value for 7.5 and 10 mg/kg dose (p = .0482).
Indicates data from five horses only.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Table 3.
Noncompartmental pharmacokinetic parameters for m‐CPP following administration of 7.5 or 10 mg/kg trazodone orally to six horses
| Pharmacokinetic Variable | 7.5 mg/kg Mean ± SD | 10 mg/kg Mean ± SD |
|---|---|---|
| T max (hr) | 0.57 ± 0.26 | 0.53 ± 0.19 |
| C max (μg/ml) | 0.04 ± 0.03 | 0.07 ± 0.02 |
| AUC0–∞ (μg*hr/ml) | 0.13 ± 0.07 | 0.31 ± 0.20 |
| AUC0–∞ (% extrap) | 18.35 ± 7.19 | 18.52 ± 6.03 |
| AUMC (hr*hr*μg/ml) | 0.77 ± 0.57 | 5.52 ± 6.50 |
| λ (hr−1) | 0.21 ± 0.10 | 0.13 ± 0.08 |
| t 1/2λ (hr) | 3.95 ± 1.93 | 6.85 ± 3.64 |
T max, time to maximum concentration; C max, maximum concentration; AUC, area under the concentration–time curve; AUMC, area under the first moment–time curve; λ, slope of the terminal phase; t 1/2λ, half‐life of terminal phase.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.2. Pharmacodynamics
All horses receiving either dose displayed some degree of sedation and ataxia, beginning as early as 20 min after administration. A significant difference was not detected in sedation scores or ataxia scores at the different doses. Despite the lack of statistical significance, the onset of sedation and ataxia in the 7.5 mg/kg dose group was delayed compared to the 10 mg/kg group. At the 10 mg/kg dose, sedation scores were significantly increased at 30 min compared to 0, 12, 24, 36 and 48 hr. Ataxia scores were also significantly increased in the 10 mg/kg dose group at 30 min compared to 0, 24, 36 and 48 hr (Figure 2a and b). A linear relationship existed between plasma concentrations and sedation scores (R 2 = .826) and ataxia scores (R 2 = .854). Sedation and ataxia scores had returned to baseline in all horses between concentrations of 0.14–0.31 and 0.07–0.14 μg/ml, respectively. At the 7.5 mg/kg dose, no significant difference was detected in either sedation or ataxia scores compared to baseline. A linear relationship between plasma concentration and effect was not seen with the 7.5 mg/kg dose.
Figure 2.
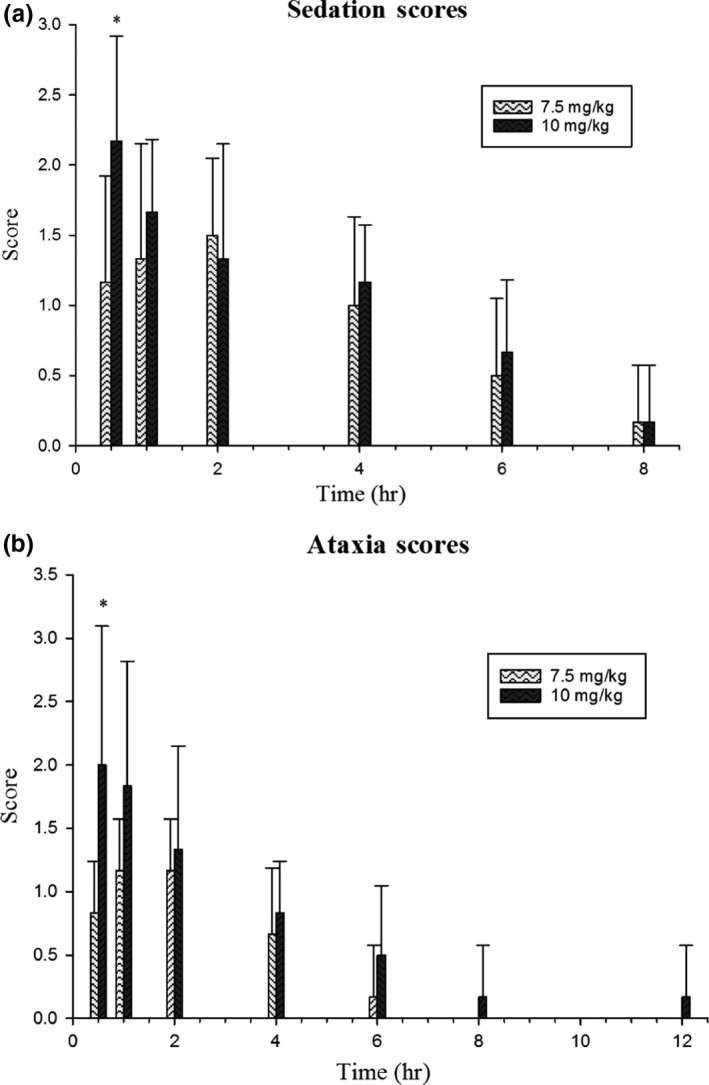
Sedation (a) and ataxia (b) scores over time in horses (n = 6) administered a single oral dose of trazodone hydrochloride at 7.5 or 10 mg/kg. The baseline score (time 0) was zero for all horses for both scoring systems. *Denotes a statistical difference from baseline
No significant differences were detected at any time point after drug administration for respiratory rate or gut sounds at either dose level. Heart rate was significantly increased (p = .031) at the 2‐hr time point compared to the 1‐hr time point for the 7.5 mg/kg dose, although it was not elevated above a normal reference range (mean HR 41 bpm). A significant difference in heart rate was not detected in the 10 mg/kg dose group. Temperature was significantly decreased (p < .05) at the 2‐ and 4‐hr time points compared to the 8‐hr time point for the 7.5 mg/kg dose. Temperature was also significantly decreased at multiple time points for the 10 mg/kg dose (Figure 3). Time to first faecal output ranged from 20 to 60 min for the 7.5 mg/kg dose and 20 to 90 min for the 10 mg/kg dose, with no significant difference detected between doses.
Figure 3.
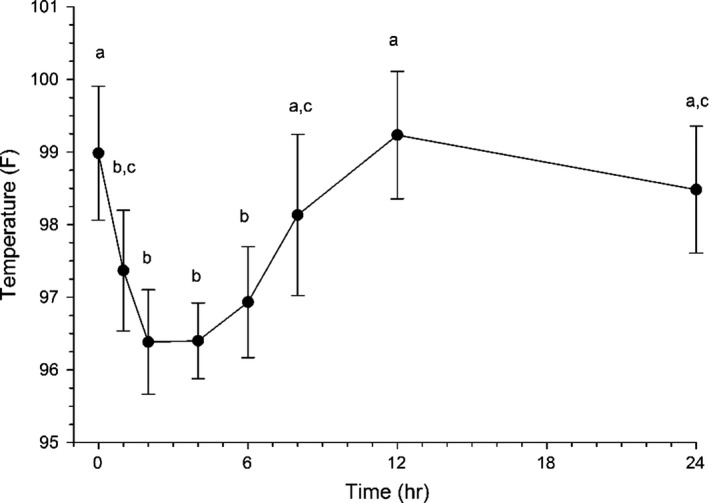
Effects of trazodone hydrochloride on body temperature in horses (n = 6) administered a single oral dose of trazodone hydrochloride at 10 mg/kg. Values with different superscript letters differ significantly between time points (p ≤ .05)
3.3. Adverse drug events
Overall, the drug was well tolerated in experimental horses. Oversedation, defined as either a sedation or ataxia score of 3/3 accompanied by a refusal to eat, was the most common adverse effect noted and was seen in three horses (horses A, B and D) at the 10 mg/kg dose, but none in the 7.5 mg/kg dose. Transient arrhythmias were detected in two horses (horses E and F) in the 10 mg/kg dose, one at 1‐hr postdosing and one at 36‐hr postdosing. Electrocardiogram readings were not performed; however, based on auscultation, sinus arrhythmias or ventricular premature contractions were considered. The abnormal rhythm detected had resolved within 10 min of initial diagnosis. One of these horses also showed muscle fasciculations concurrent with the arrhythmia. No horses had arrhythmias detected in the 7.5 mg/kg dose. One horse (horse B) developed signs of colic, fever and soft manure 32 hr after administration of the 10 mg/kg dose. Samples from this horse were available for 36 hr after drug administration; therefore, all data were included in the study. Complete blood count, palpation per rectum and abdominal ultrasound were within normal limits. Faecal float for sand, McMaster's egg count and PCR for equine coronavirus, Clostridium difficile toxins A and B, Lawsonia intracellularis, Neorickettsia risticii and Salmonella spp. were negative. Medical management with intravenous and enteral fluids and flunixin meglumine (1.1 mg/kg i.v q12 h for three doses) resulted in resolution of clinical signs within 24 hr. During the 7.5 mg/kg dose study, horse B also developed soft manure that persisted for the first 24 hr of sampling. This same horse had one other documented episode of colic during the washout period between crossover dosing.
Only one horse (horse D) had a significant adverse event at the 7.5 mg/kg dose. This horse developed a pruritic dermatitis during sampling. A small area of alopecia and crusting was noted on the head prior to drug administration. At 12 hr after drug administration, diffuse lesions characterized by pruritus, excoriations, oozing and crusting were noted on the head, neck, chest and forelimbs, which necessitated removing the horse from the study. The horse pulled its catheter and no samples were available after 8 hr, because the skin at the catheter site and over other accessible veins was too inflamed for safe venipuncture. For this reason, data from this horse for the 7.5 mg/kg dose group were not used in the mean calculations for λz or t½λ. Biopsy of the affected skin revealed eosinophilic perivascular dermatitis, with oedema and epidermal spongiosis consistent with acute allergic reaction. Treatment with dexamethasone (15 mg) intramuscularly in the semimembranosus muscle and medicated baths were initiated and the horse responded favourably within 24 hr. A tapering dose of dexamethasone was administered over 7 days, and complete resolution of signs was achieved. Signs did not recur with re‐introduction of the drug during the second phase of the crossover experiment.
3.4. Clinical cases
Medical records for 18 horses that received trazodone as a sedative were identified, including 11 geldings, six mares and one stallion aged 2–26 years. Nine were Warmbloods, three Thoroughbreds, two Quarter Horses and one each of Paint, Pony, Tennessee Walking horse and Saddlebred breeds. All horses were being stall rested for treatment of various diseases, including 12 orthopaedic cases, two post‐op colic cases, two ophthalmic cases, one behavioural issue and one tooth root abscess. Horses were placed on trazodone for a variety of adverse behaviours including owner identified anxiety, stall walking, circling, pacing, weaving, kicking stall walls, rearing and violent behaviour. Doses ranged from 2.5 mg/kg orally once a day to 10 mg/kg orally twice daily, depending on the horse's response and the desired degree of sedation. Horses were treated for a range of 1–70 days. Six horses that received trazodone were already being treated with reserpine with an inadequate response. One of these horses was switched to trazodone, and five were maintained on both reserpine and trazodone with no apparent adverse effects of combination therapy. Seventeen of the 18 (94.4%) horses treated showed significant calming effects following administration, including a decreased occurrence of the previously mentioned adverse behaviours. Adverse events noted while on the drug included clinician identified oversedation (4/18) requiring a lowering of the dose, muscle fasciculations (2/18) and the development of apparent tolerance (2/18).
4. DISCUSSION
The results of this study indicate that trazodone is an effective oral drug that can be used in horses to facilitate stall rest and recovery. Trazodone was rapidly absorbed in all the horses in this study. The actual extent of absorption could not be determined due to the lack of an intravenous dose. Intravenous dosing was not performed due to the unacceptable level of adverse effects noted in dogs and horses, including tachycardia, aggression/excitation and whole body tremors (Jay et al., 2013; Knych et al., 2017). This, in addition to the lack of a commercially available injectable formulation, makes intravenous dosing unlikely to be clinically relevant. The pharmacokinetics of the oral formulation demonstrated a moderate t½λ of approximately 7–8 hr following administration of either 7.5 or 10 mg/kg. At a dose of 4 mg/kg, Knych et al. (2017) report a t½λ of 7.11 hr. The lack of significant difference in t½λ between these doses likely indicates linear pharmacokinetics within this small dose range.
The significantly increased AUC noted for the 10 mg/kg dose compared to the 7.5 mg/kg demonstrate increased drug exposure at higher doses, which also supports linear kinetics. A previous study reports an AUC of 8.09 μg*hr/ml at 4 mg/kg orally (Knych et al., 2017). This AUC is in between the AUCs reported here for 7.5 and 10 mg/kg (means of 5.77 and 11.42 μg*hr/ml, respectively). This discrepancy may represent differences in absorption of the drug based on the formulation and method of administration. The present study used commercially available trazodone tablets administered via syringe, whereas the previous study used a trazodone powder administered in feed. Differences in absorption profiles of these to formulations are supported by the differences noted in T max reported. Use of the tablets resulted in a mean T max of 0.37–0.42 hr, whereas administration of the powdered form in feed resulted in a T max of approximately 1.7 hr. Bioavailability reported by Knych et al. (2017) was 63%, but caution should be used in extrapolating this data to the commercially available tablet form.
Although there was a trend towards a higher C max, the difference was not significant. The lack of significance for the C max is likely due to the small number of animals used as well as the method of administration used in this study. Oral administration instead of intragastric administration was used to more closely mimic treatment in clinical patients. Despite best practices being used to deliver oral medication, a small amount of drug was lost during delivery. This may have contributed to the variability noted in C max. An additional factor that may contribute to variability is the lack of fasting prior to drug administration. This was again done to more closely mimic treatment in clinical patients, as horses on stall rest are frequently fed free choice hay in order to keep them occupied throughout the day. For this study, horses were fed two flakes of hay at 10 p.m. on the night prior to dosing and allowed to eat up to 1 hr prior to dosing. Some horses finished all feed, while others still had hay left at the time feed was pulled. Therefore, the amount of feed in the stomach may have affected the rate or extent that the drug reached the small intestine and was available for absorption (Baggot, 1992). In humans, absorption of trazodone was irregular in fasting subjects and improved after food intake, but the C max concentrations were lower and the T max was increased with feeding (Nilsen & Dale, 1992). However, due to the differences in diet between humans and horses, the actual effects of feeding may differ. The effects of feeding on drug absorption remain to be investigated.
With some drugs, oral administration and subsequent collection of blood samples from the jugular vein may lead to falsely elevated plasma concentrations due to direct absorption from the sublingual vessels that drain into the jugular vein (Kaukinen, Aspegrén, Hyyppä, Tamm, & Salonen, 2011; Messenger, Davis, LaFevers, Barlow, & Posner, 2011). A comparison of plasma concentrations of trazodone collected from the cephalic and jugular veins indicated there is minimal absorption from the sublingual space, and sampling from the jugular likely does not affect overall drug concentrations.
The active metabolite, m‐CPP, was present in all horses following administration of either dose of trazodone. Even though it was present in all horses, it was present in low concentrations, representing only 2.55 ± 1.41% of the total AUC. This is similar to a previous report in horses, where m‐CPP concentrations were less than 10% of trazodone concentrations following either oral or intravenous administration of trazodone. Given the low amount detected in plasma, it is unlikely that the metabolite contributes significantly to drug effect.
Oral administration of trazodone produced some degree of sedation and ataxia in all experimental horses. The duration of sedation ranged between 4–8 and 2–8 hr for the 10 and 7.5 mg/kg dose, respectively. The duration of ataxia ranged between 2–6 and 4–12 hr for the 10 and 7.5 mg/kg dose, respectively. The longer duration of ataxia reported compared to sedation for the 10 mg/kg dose is due to one horse having an ataxia score of 1 at the 8‐ and 12‐hr time point. All other horses had returned to an ataxia score of 0 by 6 hr after administration. The degree to which sedation and ataxia was produced was highly variable among horses. This may be due to the factors affecting absorption previously discussed, including method of administration and effects of feed. After administration of 4 mg/kg, sedation without significant ataxia was documented in five of six horses, further suggesting a dose‐dependent response (Knych et al., 2017). This information highlights the need for dosing to be tailored based on the individual animal's response.
A linear relationship existed between plasma concentrations and sedation and ataxia scores at the 10 mg/kg dose where oversedation was noted in three of six horses. Behavioural calming effects in dogs are seen at concentrations between 0.13 and 2 μg/ml (Jay et al., 2013). A threshold concentration of 0.7 μg/ml has been described for humans being treated for major depressive order (Mihara et al., 2002). In this study, all horses were within the expected therapeutic range for dogs for at least 4 hr following administration of either dose. All horses also reached the threshold concentration for humans following administration of either dose. Sedation scores had returned to baseline between concentrations of 0.14 and 0.31 μg/ml and ataxia scores had returned to normal between concentrations of 0.07–0.14 μg/ml in the horses in this study. The lower concentrations noted for ataxia scores relate to one outlier horse that was graded a 1 on ataxia scores for 6 hr longer than the other horses. Exclusion of this horse from the data analysis results in a concentration resulting in ataxia of 0.31–0.54 μg/ml. Overall, results of this study suggest the behavioural calming concentration of trazodone and m‐CPP is approximately 0.14 μg/ml in normal animals. The behavioural calming concentration in clinical horses for which trazodone is prescribed would be expected to be more variable and dependent on the individual animal's temperament and degree of anxiety.
There were minimal physiologic effects associated with trazodone administration in experimental horses. Clinically significant changes were not noted in relation to heart rate, respiratory rate and gut sounds. Significant changes were noted in relation to body temperature, particularly in the 10 mg/kg dose group. The body temperature was significantly decreased at multiple time points following administration of trazodone. This phenomenon has been previously reported in horses (Knych et al., 2017). The cause is unknown; however, it may be due to the sedative effects of the drug resulting in decreased anal tone and potential pneumorectum. Trazodone has been shown to affect the core body temperature in humans, resulting in a tendency to advance the appearance time of the minimal temperature based on daily temperature rhythms compared to placebo and this effect is related to the development of slow wave sleep (Suzuki , Yamadera, Nakamura, & Endo, 2002; Yamadera, Suzuki, Nakamura, & Endo, 1999). Conversely, trazodone has also been associated with hyperthermia in humans that develop neuroleptic malignant syndrome or serotonin syndrome, although this typically only occurs with administration of multiple medications, including other serotonergic drugs, monoamine oxidase inhibitors, antipsychotics or dopamine antagonists (Sokoro, Zivot, & Ariano, 2011). Full body sweating was reported in four of six horses dosed with 4 mg/kg p.o. in a previous study (Knych et al., 2017); however, this was not evident in the horses in the current study.
Adverse drug events (ADE) were noted during this trial. Oversedation was the most frequent ADE, as previously discussed. Two horses also developed arrhythmias and muscle fasciculations. These were transient and of a short duration. Lower doses of trazodone (4 mg/kg PO) were not noted to cause arrhythmias, and no change in the percentage of atrioventricular block was noted when administered to healthy horses undergoing fitness training (Knych et al., 2017). Trazodone has been associated with arrhythmias in humans, including prolonged QT intervals, ventricular premature contractions and torsades de pointes (Tarantino, Appleton, & Lansdell, 2005). These effects are most commonly noted in people with pre‐existing causes of ventricular irritability; therefore, the use of this drug in horses with pre‐existing cardiac disease or other drugs that may prolong the QT interval should be performed with caution. The cause of the muscle fasciculations noted in the horses with arrhythmias is unknown, but may be related to general sedation and ataxia. The arrhythmias auscultated were of such short duration they were deemed unlikely to be associated with hypoxia‐related muscle weakness. The effect of trazodone on skeletal muscle ion channels is not reported.
The use of trazodone in clinical patients was deemed successful in that it subjectively caused some degree of sedation and modified adverse behaviours associated with stall rest in 94.4% of cases. Horses still required additional sedation for prolonged or painful procedures. Due to the retrospective nature of this aspect of the study, the duration of action was not specifically available. One horse, the stallion, did not respond at all. Dosing this horse was difficult due to extreme agitation, and it is estimated that only 50%–60% of the dose was successfully delivered orally. Repeat or higher doses were not attempted due to the reported association between trazodone administration and priapism in human (Warner, Peabody, Whiteford, & Hollister, 1987). Although this patient showed no signs of priapism, given the fact that he was a stallion used for breeding, the risk of further treatment based on the potential for effect was considered too high by the attending clinicians and owner. Four horses were determined to be over‐sedated by initial doses of trazodone administered. The most common reason for clinicians to determine that a decrease in dose was necessary was not eating for 1–2 hr after drug administration. Three of these horses received a decrease in dose of 25% while one horse was maintained on the initial dose. Two horses developed an apparent tolerance to the drug. One horse was initially administered trazodone 10 mg/kg p.o. once daily and the drug lost effect after 14 days so the horse was switched to alpha‐casozepine with good effect. Another horse received an initial dose of 10 mg/kg p.o. once daily, which produced oversedation. The dose was then decreased to 7.5 mg/kg and was effective for a period of approximately 3 weeks. After that time, the dose was increased to approximately 9 mg/kg and was effective, but only for a short duration (approximately 6 hr). Development of tolerance to trazodone has been reported in other species, notably dogs. In a clinical trial of trazodone for postsurgical confinement in dogs, 29.7% of owners requested an increased dosage during treatment, starting 2 weeks following surgery (Gruen, Roe, Griffith, Hamilton, & Sherman, 2014).
Two horses demonstrated severe muscle fasciculations following a single dose, and the drug was discontinued. Both horses had received the drug within 8 hr following a general anaesthetic event, potentially indicating pharmacodynamic interactions between trazodone and the anaesthetic drugs used. Trazodone has been used successfully in postsurgical canine patients with no adverse effects worthy of drug discontinuation noted; however, dosing did not begin until the day after surgery and was initiated at a low dose (Gruen et al., 2014). Other ADEs noted in experimental horses (colic, dermatitis and arrhythmias) were not noted in clinical cases.
Six of the 18 clinical horses were originally treated with reserpine either prior to or at the time of admission to facilitate stall rest, with little to no clinical effect. The use of trazodone alone or in combination with reserpine was considered superior to reserpine treatment alone in all cases. No adverse effects were noted other than those already described. Both reserpine (Dowling, 2004) and trazodone (Stahl, 2013) may cause hypotension, and effects of co‐administration of these two drugs may be additive. Therefore, caution should be used with concurrent or consecutive administration of trazodone and reserpine. Two of the four clinical cases deemed to be over‐sedated in this study were treated concurrently with reserpine.
In conclusion, trazodone can be used as an alternative oral sedative for horses that demonstrate behavioural issues while being rested for various medical conditions. Dosage regimens will likely need to be tailored based on an individual horse's response. Although ADEs were noted in the horses described in this report, they were of a short duration and did not necessarily require discontinuation of the drug. Further studies investigating the pharmacokinetics of trazodone following multiple doses and with concurrent administration of other sedative and anaesthetic medications are warranted, as well as the safety of using this drug in horses that may be ridden during administration.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
AUTHOR CONTRIBUTIONS
JLD was involved in study design and execution, sample collection and analysis, manuscript preparation and submission. JS and EM were involved in study execution, sample collection and analysis. All authors have read and approved the final manuscript.
ACKNOWLEDGMENTS
Sample collection and processing were performed at the North Carolina State University College of Veterinary Medicine's Large Animal Analysis Laboratory.
Davis JL, Schirmer J, Medlin E. Pharmacokinetics, pharmacodynamics and clinical use of trazodone and its active metabolite m‐chlorophenylpiperazine in the horse. J vet Pharmacol Therap. 2018;41:393–401. 10.1111/jvp.12477
REFERENCES
- Baggot, J. D. (1992). Bioavailability and bioequivalence of veterinary drug dosage forms, with particular reference to horses: An overview. Journal of Veterinary Pharmacology and Therapeutics, 15, 160–173. 10.1111/j.1365-2885.1992.tb01003.x [DOI] [PubMed] [Google Scholar]
- Dowling, P. M. (2004). Drugs acting on the neurological system and behavior modification In Bertone J. J. & Horspool L. J. I. (Eds.), Equine clinical pharmacology (pp. 145–154). Edinburgh, UK: Saunders; 10.1016/B978-0-7020-2484-9.50013-4 [DOI] [Google Scholar]
- Gruen, M. E. , Roe, S. C. , Griffith, E. , Hamilton, A. , & Sherman, B. L. (2014). Use of trazodone to facilitate postsurgical confinement in dogs. Journal of the American Veterinary Medical Association, 245, 296–301. 10.2460/javma.245.3.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruen, M. E. , & Sherman, B. L. (2008). Use of trazodone as an adjunctive agent in the treatment of canine anxiety disorders: 56 cases (1995–2007). Journal of the American Veterinary Medical Association, 233, 1902–1907. 10.2460/javma.233.12.1902 [DOI] [PubMed] [Google Scholar]
- Jay, A. R. , Krotscheck, U. , Parsley, E. , Benson, L. , Kravitz, A. , Mulligan, A. , … Schwark, W. S. (2013). Pharmacokinetics, bioavailability, and hemodynamic effects of trazodone after intravenous and oral administration of a single dose to dogs. American Journal of Veterinary Research, 74, 1450–1456. 10.2460/ajvr.74.11.1450 [DOI] [PubMed] [Google Scholar]
- Kale, P. , Agrawal, Y. K. , Gupta, S. , Patel, C. , & Patel, I. (2014). Determination of trazodone in human plasma by reversed‐phase liquid chromatography‐mass spectrometry with electrospray ionization. International Journal of Pharmacy and Pharmaceutical Sciences, 6, 300–304. [Google Scholar]
- Kaukinen, H. , Aspegrén, J. , Hyyppä, S. , Tamm, L. , & Salonen, J. S. (2011). Bioavailability of detomidine administered sublingually to horses as an oromucosal gel. Journal of Veterinary Pharmacology and Therapeutics, 34, 76–81. 10.1111/j.1365-2885.2010.01193.x [DOI] [PubMed] [Google Scholar]
- Knych, H. K. , Mama, K. R. , Steffey, E. P. , Stanley, S. D. , & Kass, P. H. (2017). Pharmacokinetics and selected pharmacodynamics of trazodone following intravenous and oral administration to horses undergoing fitness training. American Journal of Veterinary Research, 78, 1182–1192. 10.2460/ajvr.78.10.1182 [DOI] [PubMed] [Google Scholar]
- Li‐Bo, D. , Rong‐Hua, Z. , Huan‐De, L. , Feng, W. , Ping‐Fei, F. , & Jiang, L. (2014). Quantitative analysis of trazodone in human plasma by using HPLC‐fluorescence detector coupled with strong cation exchange chromatographic column: Application to a pharmacokinetic study in Chinese healthy volunteers. Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences, 944, 43–48. 10.1016/j.jchromb.2013.11.013 [DOI] [PubMed] [Google Scholar]
- Messenger, K. M. , Davis, J. L. , LaFevers, D. H. , Barlow, B. M. , & Posner, L. P. (2011). Intravenous and sublingual buprenorphine in horses: Pharmacokinetics and influence of sampling site. Veterinary Anaesthesia and Analgesia, 38, 374–384. 10.1111/j.1467-2995.2011.00613.x [DOI] [PubMed] [Google Scholar]
- Mihara, K. , Yasui‐Furukori, N. , Kondo, T. , Ishida, M. , Ono, S. , Ohkubo, T. , … Kaneko, S. (2002). Relationship between plasma concentrations of trazodone and its active metabolite, m‐chlorophenylpiperazine, and its clinical effect in depressed patients. Therapeutic Drug Monitoring, 24, 563–566. 10.1097/00007691-200208000-00016 [DOI] [PubMed] [Google Scholar]
- Nilsen, O. G. , & Dale, O. (1992). Single dose pharmacokinetics of trazodone in healthy subjects. Pharmacology and Toxicology, 71, 150–153. 10.1111/j.1600-0773.1992.tb00535.x [DOI] [PubMed] [Google Scholar]
- Odagaki, Y. , Toyoshima, R. , & Yamauchi, T. (2005). Trazodone and its active metabolite m‐chlorophenylpiperazine as partial agonists at 5‐HT1A receptors assessed by [S‐35]GTP gamma S binding. Journal of Psychopharmacology, 19, 235–241. 10.1177/0269881105051526 [DOI] [PubMed] [Google Scholar]
- Orlando, J. , Case, B. , Thomson, A. , Griffith, E. , & Sherman, B. (2016). Use of oral trazodone for sedation in cats: A pilot study. Journal of Feline Medicine and Surgery, 18, 476–482. 10.1177/1098612X15587956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, V. P. , Midha, K. K. , & Dighe, S. (1992). Conference report: Analytical methods validation: Bioavailability, bioequivalence, and pharmacokinetic studies. International Journal of Pharmaceutics, 82, 1–7. 10.1016/0378-5173(92)90065-A [DOI] [PubMed] [Google Scholar]
- Sokoro, A. A. , Zivot, J. , & Ariano, R. E. (2011). Neuroleptic malignant syndrome versus serotonin syndrome: The search for a diagnostic tool. Annals of Pharmacotherapy, 45, e50. [DOI] [PubMed] [Google Scholar]
- Solano, A. M. , Valverde, A. , Desrochers, A. , Nykamp, S. , & Boure, L. P. (2009). Behavioural and cardiorespiratory effects of a constant rate infusion of medetomidine and morphine for sedation during standing laparoscopy in horses. Equine Veterinary Journal, 41, 153–159. 10.2746/042516408X342984 [DOI] [PubMed] [Google Scholar]
- Stahl, S. M. (2013). Stahl's essential psychopharmacology: Neuroscientific basis and practical applications, 4th ed. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Stevens, B. J. , Frantz, E. , Orlando, J. M. , Griffith, E. , Harden, L. , Gruen, M. L. , & Sherman, B. L. (2016). Efficacy of a single dose of trazodone hydrochloride for reducing signs of transport‐associated anxiety in cats and facilitating handling during veterinary examinations. Journal of the American Veterinary Medical Association, 249, 202–207. 10.2460/javma.249.2.202 [DOI] [PubMed] [Google Scholar]
- Suzuki, H. , Yamadera, H. , Nakamura, S. , & Endo, S. (2002). Effects of trazodone and imipramine on the biological rhythm: An analysis of sleep EEG and body core temperature. Journal of Nippon Medical School, 69, 333–341. [DOI] [PubMed] [Google Scholar]
- Tarantino, P. , Appleton, N. , & Lansdell, K. (2005). Effect of trazodone on hERG channel current and QT‐interval. European Journal of Pharmacology, 510, 75–85. 10.1016/j.ejphar.2005.01.009 [DOI] [PubMed] [Google Scholar]
- Warner, M. D. , Peabody, C. A. , Whiteford, H. A. , & Hollister, L. E. (1987). Trazodone and priapism. Journal of Clinical Psychiatry, 48, 244–245. [PubMed] [Google Scholar]
- Wojtasiak‐Wypart, M. , Soma, L. R. , Rudy, J. A. , Uboh, C. E. , Boston, R. C. , & Driessen, B. (2012). Pharmacokinetic profile and pharmacodynamics effects of romifidine hydrochloride in the horse. Journal of Veterinary Pharmacology and Therapeutics, 35, 478–488. 10.1111/j.1365-2885.2011.01347.x [DOI] [PubMed] [Google Scholar]
- Wong, D. M. , Davis, J. L. , Alcott, C. J. , Hepworth‐Warren, K. L. , Galow‐Kersh, N. L. , Rice, S. , & Coetzee, J. F. (2015). Pharmacokinetics and physiologic effects of alprazolam after a single oral dose in healthy mares. Journal of Veterinary Pharmacology and Therapeutics, 38, 301–304. 10.1111/jvp.12192 [DOI] [PubMed] [Google Scholar]
- Yamadera, H. , Suzuki, H. , Nakamura, S. , & Endo, S. (1999). Effects of trazodone on polysomnography, blood concentration and core body temperature in healthy volunteers. Psychiatry and Clinical Neurosciences, 53, 189–191. [DOI] [PubMed] [Google Scholar]


