Figure 5.
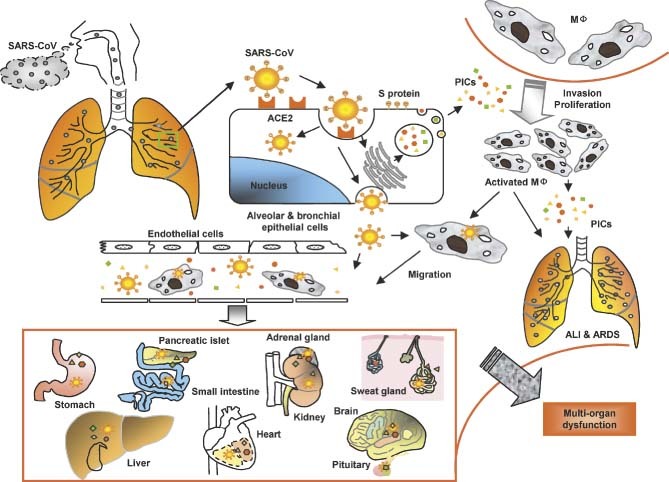
A model for the immunopathogenesis of SARS. SARS‐CoV in droplets enters into the lung, where the virus binds via its S protein to ACE2 on the alveolar or bronchial epithelial cells. The virus replicates in these cells, from which new virions are released into the blood. The infected cells under the stimulation of SARS‐CoV and some uninfected cells induced by viral antigens or PIC‐regulatory factors produce high levels of PICs to mediate inflammatory responses for combating the virus. However, these PICs also damage the host cells. Some of the PICs, eg monocyte chemoattractant protein‐1 (MCP‐1), attract monocytes in blood to migrate to the alveolar cavities, where the monocytes are stimulated by other PICs to become proliferative and/or activated macrophages (MΦ). The activated macrophages can produce more PICs and may transmit SARS‐CoV to other sites. Some of the PICs, including TGF‐β1 and TNF‐α, may induce apoptotic death of the epithelial cells, pneumocytes, and lymphocytes, or mediate pulmonary fibronosis, resulting in ALI and ARDS. The cell‐free and MΦ‐associated SARS‐CoV in the blood can be transmitted from the lung to other organs to infect the ACE2‐expressing cells in the local sites. More PICs are produced and the level of PICs in the blood is rapidly elevated, leading to multi‐organ dysfunction. MΦ = macrophages; ALI = acute lung injury; PICs = pro‐inflammatory cytokines
