FIGURE 1.
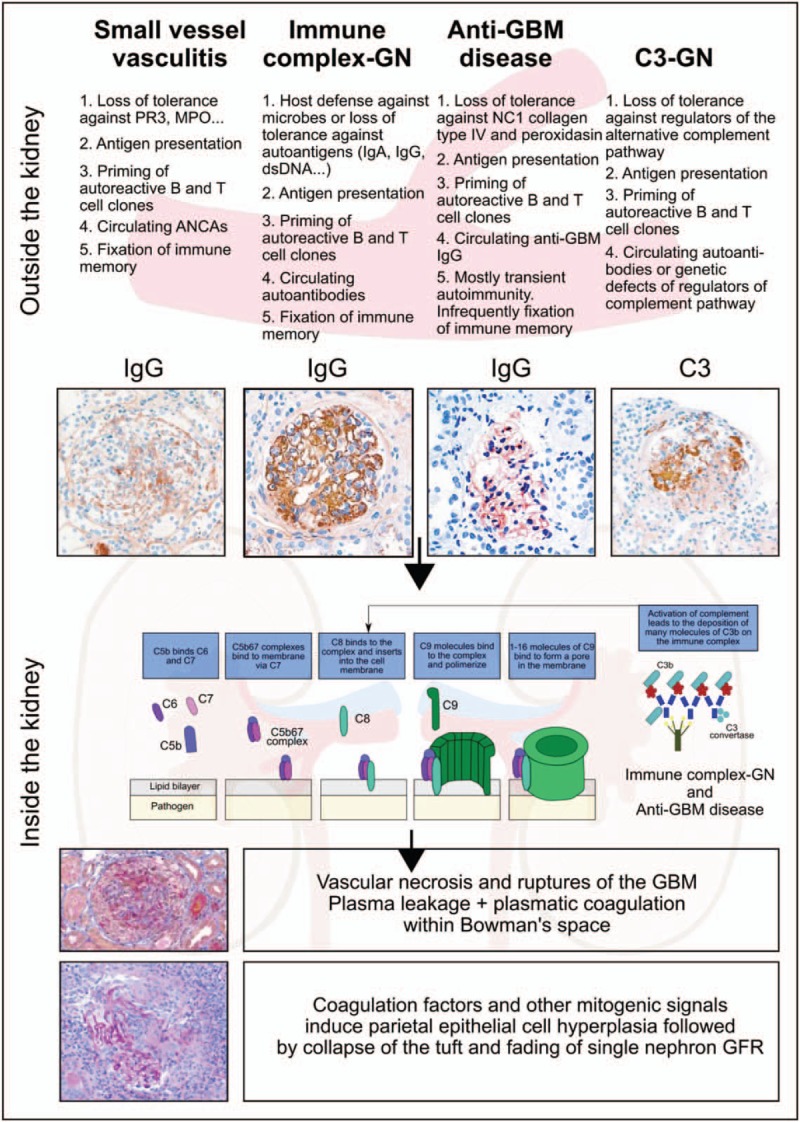
Evolution of crescent formation. The crescent is an unspecific histopathological lesion that can be triggered by a variety of different underlying disorders. This figure illustrates four of those and highlights first the extrarenal pathomechanisms leading to glomerular injury. The different patterns of immunoglobulin and complement deposits help to dissect these entities. Indeed, all of the aforementioned extrarenal drivers of injury to the glomerular microvasculature involve local complement activation as a shared molecular target for therapeutic interventions. Whenever, microvascular injury leads to rupture of the glomerular basement membrane (GBM), the leakage of plasma proteins drives parietal epithelial cell hyperplasia as the key cellular component of the crescent. Single nephron GFR decreases because of tuft collapse, rupture of the Bowman capsule, and influx of immune cells and fibroblasts are all secondary events that may or may not occur in individual glomeruli. Periglomerular immune cell infiltrates or fibrotic encasting of the activated parietal cells (fibrocellular crescents) are subsequent events that may affect the dynamics and prognosis of the disease. ANCA, antineutrophil cytoplasmic antibody; GFR = glomerular filtration rate; Ig, immunoglobulin; MPO, myeloperoxidase; PR3, proteinase 3.
