Summary
Introduction
The COVID-19 outbreak in France is disturbing our health system. Urologists in training who are already known to have burnout, are in the front line to face this disease. The aim of our study was to assess the psychological impact of COVID-19 pandemic on young French urologists in training.
Material and methods
A self-administered anonymous questionnaire evaluating the pandemic added stress, and its negative impact on work and training quality, was e-mailed to the members of the French Association of Urologists in Training (AFUF). The association includes all French junior and senior residents. The survey lasted 3 days. Multivariable analyses using logistic regression was performed to identify the predictive factors.
Results
Two hundred and seventy-five (55.5%) of the 495 AFUF members responded to the questionnaire. More than 90% of responders felt more stressed by the pandemic. Fellows and senior residents were more likely to feel that the crisis had an important impact on their work quality (OR = 1.76, IC95 = [1.01–3.13]), even more when COVID 19 patients were present in their department (OR = 2.31, IC95 = [1.20–4.65]). Past medical history of respiratory disease (OR = 2.57, IC95 = [1.31–5.98]) and taking in charge COVID19 patients (OR = 1.85, IC95 = [0.98–3.59]) were additional risk factors.
Conclusion
COVID19 pandemic has a negative impact on young French urologists in training and on their work and training quality. Managing their psychosocial well-being during this time is as important as managing their physical health.
Level of evidence
3.
Keywords: Anxiety, Virus SARS-Cov2, COVID19, Urology, Residents, Survey
Résumé
Introduction
La pandémie actuelle de COVID19 en France met sous tension notre système de santé. Les internes d’urologie, représentant une population à risque reconnu de burnout, sont en première ligne pour faire face à cette nouvelle pathologie. L’objectif de cette étude était d’évaluer l’impact psychologique du COVID19 sur les urologues en formation.
Matériels et méthodes
Un questionnaire anonyme évaluant le stress surajouté par l’épidémie, la détérioration de la qualité de travail ainsi que le retentissement sur la formation médicale a été adressé par mail à tous les membres de l’Association française des urologues en formation (AFUF). L’AFUF regroupe tous les internes et CCA/assistant de France. Ce questionnaire est resté ouvert au total trois jours. Les facteurs associés aux critères de jugement étaient calculés par régression logistique multivariée.
Résultats
Au total 55,5 % des membres de l’AFUF ont répondu au questionnaire. Plus de 90 % des participants se sentaient plus stressés à cause de l’épidémie. L’épidémie était plus susceptible d’avoir un impact négatif sur la qualité de travail des urologues les plus expérimentés (OR = 1,76, IC95 = [1,01–3,13) et lorsqu’ils prenaient en charge des patients COVID19 dans leur service (OR = 2,31, IC95 = [1,20–4,65]). Le fait d’avoir un antécédent médical respiratoire (OR = 2,57, IC95 = [1,31–5,98]) et de s’occuper de patients COVID19 (OR = 1,85, IC95 = [0,98–3,59]) étaient des facteurs de risque de stress chez les participants.
Conclusion
La pandémie de COVID19 entraîne une répercussion psychologique ainsi qu’une détérioration de la qualité de travail sur les jeunes urologues en formation français. La vigilance concernant des signaux d’épuisement doit être accrue en cette période de crise sanitaire.
Niveau de preuve
3.
Mots clés: Anxiété, Virus SARS-Cov2, COVID19, Internes, Urologie, Enquête
Introduction
The COVID-19 pandemic is completely disrupting our health care system, affecting the management of our patients and changing our medical and surgical practice. In France, according to reports from the health authorities as for the COVID-19 pandemic, the number of confirmed cases, including serious cases in the intensive care units is rising in a very fast way, just as the number of deaths, including patients who have died in hospitals and people in social-medical centers such as nursing homes [1].
In front of this fact, and as in any other country, French physicians in training are involved regardless of their specialty, in this unprecedented global health threat. Far from surgical procedures, young surgeons have changed their daily practice to respond to the emerging needs of the patients. As for any new activity there is always a learning-curve and one could understand that this is done in a stressful environment. These individuals are at high-risk to become infected, to eventually contaminate others and to spread the virus. In addition, in order to protect their family members, some have chosen to isolate themselves. All these factors, may lead to unusual stress, moral injury or mental health problems even in the setting of trained caregivers accustomed to high workload [2]. Within this population with high burn-out trends, emotional burden has not been properly evaluated [3], [4], [5].
The aim of our study was to assess the psychological impact of COVID-19 pandemic among French urologists in training.
Material and methods
Database and study population
During the stage 3 of the pandemic in France and two weeks after the beginning of COVID 19 lockdown, a self-administered anonymous questionnaire was sent from the board of the French Association of Urologists in Training (AFUF) to all its registered members. The association includes all French junior and senior residents. All urologists in training, members of the association, were eligible to participate in the study. The survey sought to evaluate the psychological impact of the COVID19 situation and was reachable via Google Form©. After the approval of the AFUF board, on the 27th of March 2020, the survey's link was e-mailed to the 495 members of the association. A reminder email was sent every day as it was decided that the survey would be closed 3 days later.
Our 17-item survey included demographic questions: gender, age, level of training (PGY 1–5, junior urologist or researcher), and geographic region. Additional survey items were: past medical history, history of smoking or psychiatric medications and the responder's judgment if the institution is providing him the necessary protection equipment. The majority of the questions in this section were close-ended.
The survey also included in a separate way, the level of confidence to treat COVID 19 patients, the impact on work and training, the degree of stress felt during duties and the need for psychiatric medications to overcome this stress.
The survey was validated by all of the authors’ group; to develop our questionnaire, we were inspired by the known risk factors of COVID-19 [1], the recommended protection tools, classic questionnaires used in the literature to assess the level of stress [6], [7], and from our daily experience facing COVID-19 patients. A copy of the questionnaire is available from the authors on request.
Statistical analysis
Quantitative variables were described as means and standard deviations and qualitative variables as numbers and percentages. Univariable and Multivariable analyses using logistic regression were performed to identify the predictive factors of stress that altered work or training quality. Statistical significance was set at p < 0.05. All tests were 2-sided. Analyses were performed using R version 3.6.2. (2009–2019 RStudio, Inc.).
Results
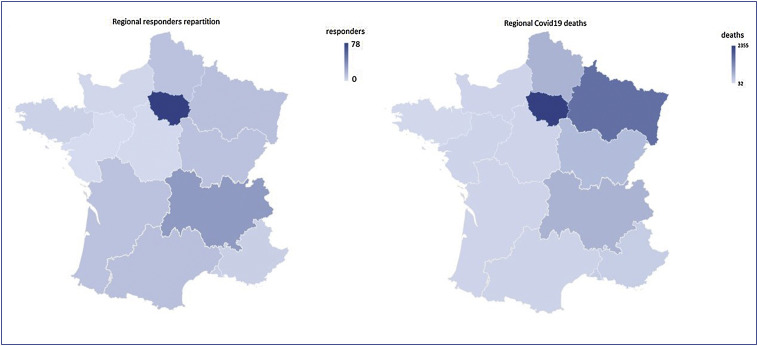
In 72 hours, we obtained 275 (55.5%) responses to the questionnaire. Overall, mean age of the responders was 29.5 years (SD = 0.47), thirty percent were female urologists and almost half of them (n = 133) worked in high epidemic regions (Fig. 1 ). Status of training among responders was homogenous, 90 (32.7%) were seniors while the others were resident or in a research year (Fig. 2 ). Among them, 211 (76.7%) had to manage COVID19 patients in their own department, despite the fact that 132 (62.5%) declared themselves unable to treat this new pathology (Table 1 ).
Figure 1.
High respondance rate in endemic regions.
Figure 2.
Demographic data of the respondents.
Table 1.
Univariable logistic regression according to the different questions of the survey.
| OR (95% CI) | p-value | |
|---|---|---|
| Ability/competency to treat COVID 19 patients if requisitioned | ||
| Sex (female) | 0.67 (0.39–1.13) | 0.15 |
| Medical History | 0.43 (0.18–1.03) | 0.08 |
| Smoker | 0.76 (0.4–1.4) | 0.44 |
| History of psychiatric medication | 3.2 (0.29–36) | 0.56 |
| Experience (Senior) | 1.3 (0.75–2.10) | 0.43 |
| COVID 19 patients in the same building | 1.38 (0.54–3.5) | 0.65 |
| COVID 19 patients in the department | 1.22 (0.7–2.2) | 0.56 |
| High epidemic location | 1.26 (0.77–2.05) | 0.39 |
| Degree of stress during duties | ||
| Sex (female) | 1.25 (0.8–1.6) | 0.44 |
| Medical History | 2.96 (1.23–7.12) | 0.01 |
| Smoker | 0.66 (0.36–1.20) | 0.22 |
| History of psychiatric medication | NA | NA |
| Experience (Senior) | 1.76 (1.05–2.97) | 0.04 |
| COVID 19 patients in the same building | 0.89 (0.37–2.15) | 0.83 |
| COVID 19 patients in the department | 2.39 (1.30–4.39) | 0.006 |
| High epidemic location | 1.71 (1.06–2.78) | 0.029 |
| Negative impact on work quality | ||
| Sex (female) | 0.69 (0.42–1.16) | 0.19 |
| Medical History | 1.70 (0.75–.84) | 0.24 |
| Smoker | 1.15 (0.62–2.12) | 0.76 |
| History of psychiatric medication | 1.31 (0.12–4.7) | 1 |
| Experience (senior) | 2 (1.17–3.44) | 0.013 |
| COVID 19 patients in the same building | 1.93 (0.8–4.64) | 0.17 |
| COVID 19 patients in the department | 2.62 (1.39–4.97) | 0.003 |
| High epidemic location | 1.71 (1.05–2.79) | 0.036 |
| Negative impact on training | ||
| Sex (female) | 1.68 (0.81–3.48) | 0.17 |
| Medical history | 1.99 (0.58–6.88) | 0.32 |
| Smoker | 1 (0.45–2.23) | 1 |
| History of psychiatric medication | NA | NA |
| Experience (senior) | 0.57 (0.30–1.09) | 0.12 |
| COVID 19 patients in the same building | 2 (0.74–5.41) | 0.23 |
| COVID 19 patients in the department | 1.11 (0.52–2.39) | 0.85 |
| High epidemic location | 1.75 (0.91–3.36) | 0.11 |
In bold: significant values.
Despite the high number of cases in France and the contagiousness of the virus, more than 50% of the responders did not have sufficient personal protective equipment (PPE) such as FFP2 masks, protective glasses or medical overcoats. The level of stress was much higher than before the crisis; 91.6% (n = 252) of the participants reported to be stressed, with a medium to high level of stress in 56.5% of the cases (Table 1).
As a consequence, for 235 of them (85.5%) this health crisis had an impact on the quality of their work (n = 235, 85.5%) (Table 1).
Very few participants had a past or present history of psychiatric disease and only 2 started anxiolytic medications.
On multivariable logistic regression (Table 2 ), experience level (OR = 1.76, IC95 = [1.01–3.13], p = 0.048) and COVID-19 patients management in the department of urology (OR = 2.31, IC95 = [1.20–4.65], p = 0.015) were significantly associated with an impaired quality of work. Finally, past medical history (OR = 2.57, IC95 = [1.31–5.98], p = 0.013) and COVID-19 patients management (0R = 1.85, IC95 = [0.98–3.59], p = 0.06) were identified as risks factors of added stress.
Table 2.
Multivariable logistic regression according to the different questions of the survey.
| OR (95% CI) | p-value | |
|---|---|---|
| Degree of stress during duties | ||
| Sex (female) | 1.41 (0.82–2.45) | 0.22 |
| Medical history | 2.57 (1.31–5.98) | 0.013 |
| Smoker | 0.72 (0.38–1.33) | 0.29 |
| Experience (Senior) | 1.66 (0.96–2.9) | 0.07 |
| COVID 19 patients in the same building | 0.69 (0.26–1.75) | 0.44 |
| COVID 19 patients in the department | 1.85 (0.98–3.59) | 0.06 |
| High epidemic location | 1.56 (0.92–2.64) | 0.097 |
| Negative impact on work quality | ||
| Sex (female) | 0.73 (0.43–1.25) | 0.23 |
| Medical History | 1.17 (0.66–2.19) | 0.6 |
| Smoker | 1.26 (0.67–2.40) | 0.48 |
| Experience (senior) | 1.76 (1.01–3.13) | 0.048 |
| COVID 19 patients in the same building | 1.81 (0.73–4.62) | 0.2 |
| COVID 19 patients in the department | 2.31 (1.20–4.65) | 0.015 |
| High epidemic location | 1.3 (0.77–2.19) | 0.33 |
In bold: significant values.
Discussion
Despite the health crisis, and the number of emergencies, this study has the strength to report a high response rate (55.5%) in 3 days only, which reveals the important interest given to this subject by young urologists [8]. It confirms that the COVID-19 crisis has a negative psychological impact on urologists in training probably due to disease outcomes uncertainties and lack of psychological preparation. This is of utmost importance when considering that this population was already having increased burnout in routine practice over the last 7 years despite the introduction of mandatory safety breaks and a limit of working time to 48 hours per week [3], [4], [5].
In China, about 3000 HCW have been infected and at least 22 have died [9]. This may explain why HCW are at increased risk of mental health problems facing pandemics such as COVID-19 [10], [11].
Recently, Lai et al. showed that HCW, including physicians, reported experiencing psychological burden of COVID 19 patients’ care, with more severe symptoms reported by those in Wuhan city, epicenter of the original outbreak [12]. Our findings are in line with these results, since we demonstrated a higher level of stress for responders working in high epidemic region. Residents working in these areas most probably need more protection, support and training than the others, and this was mentioned in the updated WHO recommendations for local risk assessment in high-risk areas [13].
In previous epidemics, mental health and psychosocial support (MHPSS) has been reported as a key priority [14] and during the acute SARS outbreak, 89% of HCW, reported psychological symptoms [15]. To our knowledge, our study is the first to assess the impact of COVID 19 crisis on a sub-population of young surgeon residents and fellows.
Herein, the degree of stress reported by these young caregivers was significantly correlated to the presence of COVID 19 patients in their department and to their personal past medical history of respiratory disease. This could reflect their fear of the viral infection that have been reported to lead to a more severe form in case of such medical history [16]. More than 50% felt to be not enough protected in their institutions, accounting that PPE shortage has been reported worldwide [17].
Even though to date no certain direct impact of COVID-19 on urogenital tissues has been reported [18], urologists can be involved in the initial evaluation of patients presenting with fever without other symptoms of COVID-19, often interpreted as urosepsis. An immediate diagnosis through laboratory tests could reduce this risk and reassure urologists. That being said, while this test is still unavailable, all efforts should be done to provide sufficient PPE to the urology residents, by expanding the potential use of eye protection and fluid resistant surgical masks [19].
The training has been judged to be affected by more than 80% of the responders. This finding needs to be carefully interpreted in our population, where a feeling of being well trained was found to be the only protective factor against burnout [4].
On the other hand, it is urgently needed to provide courses on COVID 19 and on upper respiratory tract infections (URTI) management among trainees. This should be performed and promoted by our scientific associations through e-learning and webinar [20], [21], [22] and could create a supportive educational environment [23].
Moreover, the use of social media [25], especially in this young population could be a great tool to provide fast and accessible courses in order to propose to every practitioner the best support for COVID-19 management as for their own urological training [24], [25].
We found that fellows and senior residents were more stressed and were more likely to feel that the crisis had an important impact on their work quality. This finding is probably explained by the feeling of inability to provide competent medical care in a brand new subject never been learned in medical school that they finished many years ago [26], [27]. Hence, in France, a collaborative and helping crisis cell has been set up for every resident in need. Under the leadership of a national residents’ union, this cell connects physicians in training with psychiatry residents 24 hours a day, in all regions of the country, in order to address their anxiety and to give them all the needed support.
Limitations
The findings of this study should be considered in view of its limitations: Survey research has inherent limitations in particular related to whether responders answered the survey questions honestly; this is a valid concern for all survey research and one reason why the survey was anonymous. We used a non-validated questionnaire to assess stress and psychological impact of the crisis; other questionnaires like the 12-item version of the General Health Questionnaire (GHQ-12) which is a frequently used and well-standardized measure of recent emotional distress [6], could have been used. Also, a pilot-test of the survey instrument among HCW was recommended to assess its validity. However, owing to time constraints, this was not done. Further assessments of this questionnaire in other populations could improve its reliability. The survey duration was voluntarily reduced knowing the current workload of physicians. Our study was timed after the announcement of an extension of the duration of the ongoing semester of this academic year, which could be a confusion bias of stress. Indeed, in France, residency is divided into semesters within different departments (in May and November). Usually residents can experience an added level of stress approaching this department change, but a prolongation also can be confusing.
Conclusion
Our data have expressed the necessity to bear in mind that surgical residents and fellows in high epidemic regions require a particular attention. Preservation of work quality in this stressful period and promotion of e-learning for trainees are mandatory.
Once the crisis will be over, all the medical staff and the supervisors should monitor the young colleagues in training to reflect on and learn from all personal experiences in order to create a meaningful narrative rather than a traumatic one.
Author's contributions
M. Abdessater: Protocol/project development, Data analysis, Manuscript writing/editing.
M. Rouprêt: Protocol/project development, Manuscript writing/editing.
V. Misrai: Protocol/project development, Manuscript writing/editing.
U. Pinar: Protocol/project development, Data analysis, Manuscript writing/editing.
X. Matillon: Data collection.
B. Gondran Tellier: Data collection.
L. Freton: Data collection.
M. Vallée: Data collection.
I. Dominique: Data collection.
M. Felber: Data collection.
Z.E. Khene: Data collection.
E. Fortier: Data collection.
J. Boustany: Protocol/Data collection.
F. Lannes: Data collection.
C. Michiels: Data collection.
T. Grevez: Data collection.
N. Szabla: Data collection.
F. Bardet: Data collection.
K. Kaulanjan: Data collection.
E. Seizilles de Mazancourt: Data collection.
G. Ploussard: Protocol/project development; Manuscript writing/editing.
B. Pradere: Protocol/project development; Data management & collection; Data analysis, Manuscript writing/editing.
Ethics
Research involving Human Participants and/or Animals: not applicable.
Informed consent: not applicable.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.World Health Organization (WHO). Coronavirus disease (COVID-2019) situation reports. Available from URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed March 2020).
- 2.Xiang Y.-T., Yang Y., Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roumiguié M., Gamé X., Bernhard J.-C. Does the urologist in formation have a burnout syndrome? Evaluation by Maslach Burnout Inventory (MBI) Prog Urol. 2011;21:636–641. doi: 10.1016/j.purol.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Gas J., Bart S., Michel P. Prevalence of and predictive factors for burnout among French urologists in training. Eur Urol. 2019;75:702–703. doi: 10.1016/j.eururo.2018.12.037. [DOI] [PubMed] [Google Scholar]
- 5.Marchalik D., Goldman C.C., Carvalho F.F.L. Resident burnout in USA and European urology residents: an international concern. BJU Int. 2019;124:349–356. doi: 10.1111/bju.14774. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg D., Williams P. NFER Nelson Publishing; Windsor (UK): 1991. A user's guide to the General Health Questionnaire. [Google Scholar]
- 7.Piccinelli M., Bisoffi G., Bon M., Cunico L., Tansella M. Validity and test–retest reliability of the Italian version of the 12 item General Health Questionnaire in general practice: a comparison between three scoring methods. Compr Psychiatry. 1993;34(3):198–205. doi: 10.1016/0010-440x(93)90048-9. [DOI] [PubMed] [Google Scholar]
- 8.Dykema J., Jones N.R., Piche T., Stevenson J. Surveying clinicians by web: current issues in design and administration. Eval Health Prof. 2013;36(3):352–381. doi: 10.1177/0163278713496630. [DOI] [PubMed] [Google Scholar]
- 9.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;12 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 10.Abdessater M., Roupret M., Misrai V. COVID-19 outbreak situation and its psychological impact among surgeons in training in France. World J Urol. 2020 doi: 10.1007/s00345-020-03207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 12.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO: Infection Prevention and Control Guidance for COVID-19 available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control.
- 14.Dickson K., Bangpan M. What are the barriers to, and facilitators of, implementing and receiving MHPSS programmes delivered to populations affected by humanitarian emergencies? A qualitative evidence synthesis. Glob Ment Health (Camb) 2018;5:e21. doi: 10.1017/gmh.2018.12. [Published 2018 Jun 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chua S.E., Cheung V., Cheung C. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49(6):391–393. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 16.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [published online January 29, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang L., Lin G., Tang L. Special attention to nurses’ protection during the COVID-19 epidemic. Crit Care. 2020;24:120. doi: 10.1186/s13054-020-2841-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu Z., McGoogan J.M. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. PMID 32091533. [DOI] [PubMed] [Google Scholar]
- 19.Sayburn A. Covid-19: PHE upgrades PPE advice for all patient contacts with risk of infection. BMJ. 2020;369:m1391. doi: 10.1136/bmj.m1391. [DOI] [PubMed] [Google Scholar]
- 20.Carrion D.M., Rodriguez-Socarrás M.E., Mantica G. Current status of urology surgical training in Europe: an ESRU–ESU–ESUT collaborative study. World J Urol. 2020;38:239–246. doi: 10.1007/s00345-019-02763-1. [DOI] [PubMed] [Google Scholar]
- 21.Griffin C., Aydın A., Brunckhorst O. Non-technical skills: a review of training and evaluation in urology. World J Urol. 2019 doi: 10.1007/s00345-019-02920-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veneziano D., Morgia G., Castelli T. Evaluation of the “Teaching Guide for Basic Laparoscopic Skills” as a stand-alone educational tool for hands-on training sessions: a pilot study. World J Urol. 2020 doi: 10.1007/s00345-020-03161-8. [DOI] [PubMed] [Google Scholar]
- 23.Meher S.K., Kurwal N.S., Suri A. E-learning through telemedicine in neurosurgical teaching and patient care. Int J Telemed Clin Pract. 2017;2(1):2–11. doi: 10.1504/IJTMCP.2017.082099. [DOI] [Google Scholar]
- 24.Arslan B., Gönültaş S., Gökmen E. Does YouTube include high-quality resources for training on laparoscopic and robotic radical prostatectomy? World J Urol. 2019 doi: 10.1007/s00345-019-02904-6. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization . WHO; Geneva: 2018. Occupational safety and health in public health emergencies: a manual for protecting healthworkers and responders. [Google Scholar]
- 26.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. Published online April 07. [DOI] [PubMed] [Google Scholar]
- 27.Bao Y., Sun Y., Meng S. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]