Abstract
Since December 2019, the epidemic of coronavirus disease 2019 (COVID-19) has spread very rapidly in China and worldwide. In this article, we report on a 75-year-old man infected with 2019 novel coronavirus who has end-stage kidney disease (ESKD). COVID-19 patients with ESKD need isolation dialysis, but most of them cannot be handled in time due to limited continuous renal replacement therapy (CRRT) machines. CRRT provided benefits for this patient by removing potentially damaging toxins and stabilizing his metabolic and hemodynamic status. With the control of uremia and fluid status, this patient ended up with an uneventful post-CRRT course, absence of clinical symptoms, and negative PCR tests. Greater efforts are needed to decrease the mortality of COVID-19-infected ESKD patients.
Keywords: Coronavirus disease 2019, End-stage kidney disease, Dialysis, Continuous renal replacement therapy
Introduction
Since December 2019, the epidemic of coronavirus disease 2019 (COVID-19) has spread very rapidly in China and worldwide [1]. Up to March 3, COVID-19 has led to 2,873 deaths in China with a 2% mortality rate, which surpassed the total of SARS (774 deaths) and MERS (858 deaths) [2]. Clinical characteristics of patients with COVID-19 infection have been reported in previous studies [3]. However, there are limited data about the clinical features of infections in patients with end-stage kidney disease (ESKD). Most ESKD patients return to their homes for isolation when infected, which leads to a high risk of mortality.
Case Presentation
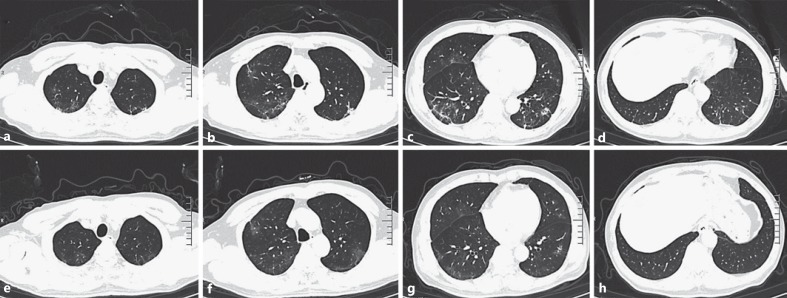
On February 11, 2020, a 75-year-old man with ESKD living in Wuhan was referred to Huoshenshan Hospital with a 2-week history of cough and chest tightness. Due to his symptoms and travel history, a chest CT was ordered (Fig. 1) and an oropharyngeal swab specimen was collected and tested with 2019 novel coronavirus RT-PCR assays several days before his hospitalization. The patient received 75 mg of oseltamivir orally twice daily. Immediately after the positive RT-PCR result was revealed, the patient was referred to Huoshenshan for hospitalization. A review of the patient's history showed that he had hypertension, chronic heart failure, COPD, and ESKD and was on routine hemodialysis. The patient had an atrophied right kidney, and in 2004, he underwent an open stone surgery for his nephrolithiasis in the left kidney. After the surgery, his renal function declined gradually and eventually entered hemodialysis in 2016. Due to the exhaustion of medical resources and travel restriction inside Wuhan city, the patient presented without dialysis for 5 days. His temperature was 36.8°C, respiratory rate was 23/min, heart rate was 100/min, and blood pressure was 139/89 mm Hg. His physical examination revealed pitting edema bilaterally in his lower limbs but was otherwise unremarkable.
Fig. 1.
a-d Previous chest CT scan of the patient showing ground-glass opacity in both lungs on January 30, 2020, after symptom onset. There were multiple pieces of slightly higher density shadows scattered in the lungs, which were mostly ground glass-like changes, mainly distributed in the middle and outer zones. Inflammation affected 5.6% of the bilateral lungs. e-h Chest CT on February 22, 2020, showing absorption of bilateral ground-glass opacity after treatment. Less than 1% of the bilateral lungs was affected by inflammation.
The patient was admitted to an airborne infection isolation unit with healthcare workers following CDC recommendations for contact, droplet, and airborne precautions with eye protection. His oxygen saturation was 90% in room air and he was given oxygen therapy at 4-5 L/min flow rate. His oxygen saturation increased to 96%. Laboratory tests showed Cr 1,432.3 μmol/L, BUN 40 μmol/L, K+ 4.63 mmol/L, and uric acid 760 μmol/L. On February 12, 14, 16, 19, and 23, the patient was given continuous venovenous hemodiafiltration 5 times and decreased water retention for 2,400, 1,904, 1,500, 1,200, and 1,500 mL, respectively. The total duration of continuous renal replacement therapy (CRRT) (continuous venovenous hemodiafiltration: blood flow, 120 mL/min; effluent flow rate, 1,000 mL/h; ultrafiltration rate, 150-200 mL/h; anticoagulation agent, heparin; vascular access site, right jugular vein) was 53 h (14, 12, 8, 10, and 9 h, respectively). Respiratory distress was relieved immediately after the first CRRT session and almost disappeared after three sessions. He was also administrated Arbidol 200 mg tid for 8 days from February 12. The laboratory tests were repeated on these days (Table 1). CRRT improved his BUN, serum Cr, uric acid, potassium, and C-reactive protein levels. The chest CT was repeated on February 22 (Fig. 1). An oropharyngeal swab specimen was collected twice and both tested negative in 2019 novel coronavirus RT-PCR assays on February 21 and 24, respectively. On February 26, his temperature was 36.6°C, respiratory rate was 17/min, heart rate was 79/min, blood pressure was 132/96 mm Hg, and oxygen saturation was 99% in room air. He met the criteria for hospital discharge in China (absence of clinical symptoms and radiological abnormalities, and 2 negative PCR results). Then, the patient was discharged home on February 26.
Table 1.
Laboratory characteristics of the patient with ESKD infected with COVID-19
| Feb 11 | Feb 13 | Feb 15 | Feb 16 | Feb 17 | Feb 20 | Feb 21 | Feb 25 | Feb 26 | |
|---|---|---|---|---|---|---|---|---|---|
| White blood cells, ×109 per L | 7.2 | 6.8 | 6 | 6.3 | 6.7 | 7.4 | 7.4 | 5.9 | 6 |
| Neutrophil count, ×109 per L | 6.41 | 6.03 | 5.2 | 5.47 | 5.52 | 6.05 | 5.95 | 4.86 | 4.72 |
| Lymphocyte count, ×109 per L | 0.28 | 0.27 | 0.35 | 0.42 | 0.46 | 0.61 | 0.87 | 0.46 | 0.69 |
| C-reactive protein, mg/L | 200.18 | 192.44 | 119.16 | 92.34 | 70.48 | 40.56 | 24.06 | 14.23 | 13.04 |
| Fibrinogen, g/L | 5.22 | 4.22 | 4.85 | 3.74 | 3.53 | 3.44 | 3.69 | 3.58 | 3.38 |
| D-dimer, mg/L | 3.51 | 4.75 | 3.6 | 3.42 | 2.93 | 3.99 | 3.07 | 2.45 | |
| BUN, mmol/L | 40 | 36.34 | 29.49 | 29.45 | 31.38 | 39.47 | 38.51 | 36.7 | 33.82 |
| Cr, μmol/L | 1,432.3 | 1,084.7 | 873.1 | 820.2 | 886 | 1,091.1 | 902 | 1,037 | 924.6 |
| Uric acid, μmol/L | 760 | 489 | 359 | 320 | 351 | 440 | 421 | 382 | 349 |
| Cystatin C, mg/L | 8 | 4.62 | 4.53 | 2.79 | 5.46 | 6.13 | 5.99 | 4.34 | 4.64 |
| Brain natriuretic peptide, pg/mL | 13,254 | 8,759 | 2,203 | 1,034 | 1,200 | 231 | 243 | 270 | 253 |
ESKD, end-stage kidney disease; COVID-19, coronavirus disease 2019.
Discussion
Previous studies suggest that COVID-19 in people with chronic comorbidities can more easily become a critical illness or cause death [4]. ESKD patients may be at great risk of COVID-19 infection due to suppression of the immune system and may have poorer outcomes from COVID-19. In this article, we reported on an ESKD patient with COVID-19 who was treated with CRRT to save his life. This case ended up with an uneventful post-CRRT course and negative PCR tests.
Several reasons may contribute to this uneventful course. First, the ESKD pathogenesis in our case was atrophy and natural aging without other medical history and chronic comorbidities. Second, since our hospital is a newly built designated hospital for COVID-19, there are enough CRRT machines and protective equipment for critical COVID-19 patients. Our case only presented without dialysis for 5 days before admission. Besides, all doctors and nurses received systemic training for emergency rescue, protection measures, and strict isolation.
Although CRRT is a normal treatment for saving critically ill ESKD patients, most COVID-19-infected ESKD patients would not receive CRRT or normal hemodialysis due to limited CRRT resources and strict isolation requirements. Besides, there is no family dialysis in China. As far as we know, more than 6 infected ESKD patients died of multiple organ dysfunction syndromes. Therefore, more medical resources such as CRRT machines, protection suits, and N95 respirators are needed to be prepared in this COVID-19 crisis, and more intensive care is urgently needed to decrease the mortality of COVID-19-infected ESKD patients.
Statement of Ethics
A written informed consent of the patient for publication has been obtained.
Disclosure Statement
The authors declare that they have no relevant financial interests and no conflict of interest.
Funding Sources
This work was supported by the National Natural Science Foundation (grant 81700579), Shanghai science and technology talent program (19YF1450300), the National Social Science Fund of China (No. 17AGL024), and general scientific research project of Huoshenshan hospital (No. 140).
Author Contributions
C.X. and B.Y. drafted and revised the manuscript; all authors attended the interview.
References
- 1.World Health Organization Official Website [Internet] Available from: https://www.who.int.
- 2.Livingston E, Bucher K, Rekito A. Coronavirus disease 2019 and influenza. JAMA. 2020 Feb; doi: 10.1001/jama.2020.2633. [DOI] [PubMed] [Google Scholar]
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, China. JAMA. 2020;323((11)):1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb;395((10223)):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]