A 69-year old man, from Lombardy, Italy, was admitted to our unit because of acute respiratory distress syndrome that required mechanical ventilation; he was in Nice, France, on holiday. He had previously been fit and well; he had a history of hypertension controlled with bisoprolol 2·5 mg/day. He initially reported vomiting and diarrhoea, and 7 days afterwards, he came to our emergency department with a cough, fever of 39°C, and dyspnoea. He was immediately transferred to our intensive care unit (ICU) because of the respiratory distress syndrome and severe hypoxia. Investigations found a haemoglobin concentration of 15·4 g/dL, a platelet count of 187 × 109 per L, and a leucocyte count of 14·9 × 109 per L (neutrophils 89%, lymphocytes 7%, monocytes 4%, and no eosinophils or basophils 0%). His blood pH was 7·27, partial pressure of carbon dioxide was 45·3 mm Hg, partial pressure of oxygen was 146 mm Hg, and peripheral oxygen saturation was 98·2%.
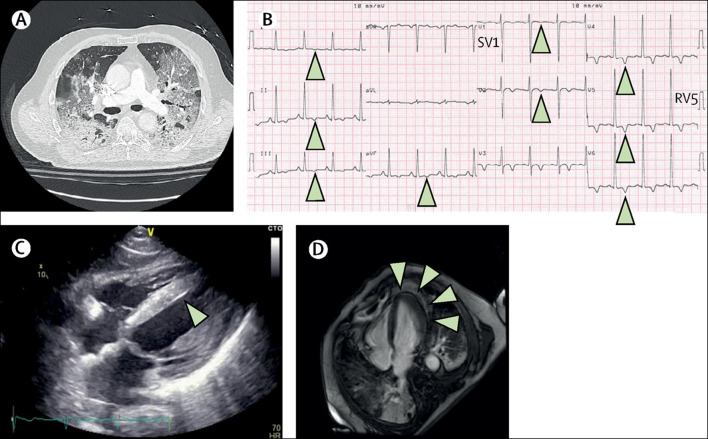
A CT of his chest showed bilateral ground-glass opacities and condensations (figure ; video). PCR of swabs taken from his upper respiratory tract showed severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) confirming a diagnosis of coronavirus disease 19 (COVID-19). Multiplex PCR was negative for other viruses using BioFire FilmArray Respiratory Panel 2 plus (bioMérieux, Marcy l'Etoile, France) and no bacterial infections were found. An electrocardiogram (ECG), done on admission to the ICU, showed signs of left ventricular hypertrophy (LVH) and diffuse inverted T waves (figure)—a previous ECG showed inverted T waves in anterior leads only. High-sensitivity cardiac troponin I concentration was raised at 9002 ng/L (normal <40). Transthoracic echocardiography showed mild LVH; the left ventricular ejection fraction and wall motion were within normal limits (figure; video). The patient was known to have LVH which was probably caused by his chronic hypertension.
Figure.
Myocarditis and coronavirus disease 19
(A) Chest CT shows bilateral crazy paving pattern, ground-glass opacities and condensations. (B) Electrocardiogram shows diffuse T-wave inversion (arrowheads) and left ventricular hypertrophy. (C) Echocardiogram shows left ventricular hypertrophy (arrowhead). (D) Cardiovascular magnetic resonance—4 chamber view—shows subepicardial late gadolinium enhancement of the apex and inferior wall (arrowheads).
Antiplatelet therapy—aspirin—and anticoagulation therapy—fondaparinux—were started because we suspected a non-ST elevation myocardial infarction: his Global Registry of Acute Coronary Events (GRACE) score was greater than 140. However, coronary angiography showed no disease, but cardiovascular magnetic resonance scanning showed subepicardial late gadolinium enhancement of the apex and inferolateral wall—suggestive of myocarditis (figure; video). We decided not to do an endomyocardial biopsy because the patient showed no signs of heart failure or arrhythmias. Additional tests for common causes of myocarditis—including parvovirus B19, human herpes virus, Epstein-Barr virus, enterovirus, cytomegalovirus, adenovirus, HIV, and hepatitis C virus—were negative. We therefore concluded that SARS-CoV-2 infection was the most likely cause of our patient's myocarditis. We gave the patient hydrocortisone at day 11 for 9 days with the aim of reducing inflammation—particularly of the myocardium. The patient was weaned off mechanical ventilation and discharged from the ICU after 3 weeks.
We believe this comprehensive description of myocarditis associated with COVID-19 confirms the importance of recent data reporting acute cardiac injury in almost a fifth of patients, with a 50% survival rate. It is recommended that troponin is not routinely measured in patients with COVID-19. However, physicians need to pay heed to the possibility of myocarditis in cases of COVID-19: in cases with high GRACE scores and dynamic ECG changes, usual guidelines to exclude the possibility of an acute myocardial infarction, including measuring troponin and doing an angiogram within 24 h, need to be followed (video).
Contributors
We were all involved in the care and management of the patient, and the writing, editing, and preparing the manuscript. Written consent for publication was obtained from the patient.
Supplementary Material
Myocarditis, COVID-19, ECG, troponin, and risk factors
Myocarditis in a patient with COVID-19
Youtube url: https://youtu.be/g8-55pUwdY4
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Myocarditis, COVID-19, ECG, troponin, and risk factors
Myocarditis in a patient with COVID-19
Youtube url: https://youtu.be/g8-55pUwdY4