Abstract
Stem and derivative cells induced from somatic tissues are a critical tool for disease modeling but significant technical hurdles hamper their use. The purpose of this review is to provide an overview of pitfalls and mitigation strategies for the nonstem cell biologist using induced pluripotent stem cells and investigating neurodevelopmental disorders. What sample sizes are reasonable? What derivation and purification protocols should be used to make human neurons? In what way should gene editing technologies be used to support discoveries? What kinds of preclinical studies are the most feasible? It is hoped that this roadmap will provide the necessary details for experimental planning and execution for those less familiar in the area of stem cell disease modeling. High‐quality human preclinical models will allow for the discovery of molecular and cellular phenotypes specific to different neurodevelopmental disorders, and may provide the assays to advance translational medicine for unmet medical needs.
Keywords: genetic engineering, neurodevelopmental disorders, neuronal induction, somatic cell reprogramming, stem cells, therapeutics
Significance statement.
Modeling human neurodevelopmental disease using stem cell biology techniques requires significant expertise to allow for discovery of cell phenotypes. This article provides a roadmap for experimental planning for those less familiar with the use of induced pluripotent stem cells to model human neurodevelopmental disease.
1. INTRODUCTION
Since the discovery of human somatic cell reprogramming,1 disease modeling in patient‐derived cells has become a critical component to elucidate mechanistic insight into pathology. Referred to as iPSCs (induced pluripotent stem cells) the potential and promise were plain to see, but the reality of disease modeling has proven more challenging than initially hoped.2 Timelines for most projects have extended, and significant resources related to simply understanding basics of cell quality have been required.3 This is true of all diseases being modeled in iPSCs but is even more so for brain diseases because of the sheer number of cell types and our lack of understanding (compared with other organs such as kidney or heart) about tissue organization. This review is focused on iPSCs, as opposed to stem cells derived from an embryo (ES cells), because iPSCs can be made from subjects after a disease has been diagnosed (ES cells by definition are made from an embryo).
Neurodevelopmental disorders (NDDs) include a large spectrum of diseases that affect the way the brain grows, including the wide spectrum of autism spectrum disorders and intellectual disabilities. For many NDDs, mutations have been identified that can be causally linked to disease, and several of these genes have been investigated in mouse, fly, worm, and frog homologs, providing significant insight into gene function. Still, most disease phenotypes are a result of a pathogenic mutation on a specific genetic background which contributes to the variable spectrum of phenotypes observed, even with fully penetrant mutations. For this reason, disease modeling in cells from human subjects with a disease captures the genetic spectrum of disease, at least for in vitro modeling of cell‐autonomous effects. NDDs provide a unique modeling opportunity using patient‐derived cells because “development” from a stem cell state is triggered by the experimenter by the addition of specific transcription factors or small molecules that recapitulate a development stage in some specific sequential order, meaning defined development stages can be directly assayed for specific hypotheses relevant to disease. Difficulties arise, however, in the accurate ability to maintain stem cells in an undifferentiated state, in differentiating CNS cell types, and in achieving consistency in postmitotic cell population types, all problems compounded by the fact that cells are derived from different individuals, meaning that while genetic background contributes to disease by interactions with pathogenic mutations, it also leads to significant increases in technical variability (ie, experimental noise). What can be done to maximize this remarkable technology while minimizing variation unrelated to a disease state?
Is it better to have an expert in stem cell induction, derivation, and differentiation perform studies on a specific disease, or an expert in those diseases or related molecular pathways? One might argue that a close collaboration between the two is the ideal; however, this can be difficult to accomplish, particularly for those outside of major centers that do not have stem cell core facilities. Even for those with these facilities, the expertise required for differentiation from a stem cell state to a more differentiated state is unlikely to be performed at these centers, which usually focus on making stem cells themselves. To this end, I hope to provide a “roadmap” for the nonstem cell expert that can be applied across different neurodevelopmental diseases as a baseline for discussion and planning for experimental design, troubleshooting, and phenotypic discovery.
2. GENERAL ISSUES TO CONSIDER BEFORE BEGINNING
2.1. Disease choice
Minimization of variation in an experimental system, desirable in all scientific studies, is paramount in a iPSC‐based NDD stem cell study since conclusions are necessarily drawn from few, often unrelated subjects. For this reason, studies should be anchored in a mutation known to cause disease, and preferably a mutation that has a direct read‐out, such as mRNA and/or protein levels of the gene of interest or a metabolite known to be increased or decreased in human subjects with the disease. This provides clinical validity to the disease model. Amenability of a disease‐causing mutation to genetic engineering techniques (discussed later) should also be considered before a project is begun. Clinically defined or genetically heterogeneous neurodevelopmental syndromes with no known biological marker should be avoided, at least in the near future.
2.2. Selection of the initial study sample
There are not usually cohorts of somatic cells ready from multiple subjects with the same disease, although this is changing for certain diseases through projects like Simons Searchlight4 and sustained efforts at cell repositories such as Coriell. Assuming that there is no cohort of subject cells available, one option is to identify and establish a representative initial cell line that reflects disease and which has a well‐matched control. This “discovery” case/control pair could be a patient cell line sex‐matched to a healthy family member cell line, or genetically engineered lines with an isogenic control. The focus on a single case/control pair allows for in‐depth characterization and the creation of multiple replicates (eg, many stem cell clones). It also allows for simply establishing working protocols in a lab that may be unfamiliar with the necessary reagents and techniques. This discovery sample allows for rapid probing of many experimental hypotheses and extensive attention to quality control parameters. The trade‐off is that any finding is not necessarily representative of the true disease population and could be driven by genetic background of the line used. For this reason, validation sets are essential and these can be made or recruited after or during experiments on the discovery sample set. Validation samples can also be well‐controlled pairs of disease subjects with family members or genetically engineered cells with the idea that each pair can complement the discovery samples and other validation samples. All case/control pairs can be analyzed independently and consistency of signal across pairs becomes the critical outcome measure. This means not all samples need to be prepared at the same time to create case/control comparisons, taking into account the reality of sample collection for many NDDs. In short, start with one very well characterized cell line, probe and explore it, then validate in other cellular models of the disease. The analog of this is mouse transgenic studies—most mouse transgenic studies involve investigation in a single highly, inbred strain but in multiple siblings in that strain. This is equivalent to assessing a mutation in one human individual using multiple iPSC clones. Additionally, unrelated human patients recruited are in a sense equivalent to assessing a mutation on different mouse strains.
2.3. Subject selection and sample size
“How many subjects do I need?” While the answer to this question can vary and is dependent on experimental design conditions, things to consider include how representative a selected patient is that is being modelled; for example, do they possess a mutation known to be present in other cases? Are subjects with this mutation similarly affected (eg, age‐of‐onset, severity, tissue locus)? If the mutation is a large deletion or duplication, how many extra genes might be affected by the variant? Is disease predicted to be caused by a missense mutation? How certain is it that this missense mutation causes disease? Missense mutations, even those absent from large databases and which occur in a gene known to cause disease are not usually the best choice. The only unambiguous proof of a genotype/phenotype relationship is supported by statistics—patients with a similar phenotype have the identical mutation that is absent from large control cohorts. Variants or mutations that show increased frequency in disease cases but which are still present in controls should be avoided, though these are admittedly important sources of disease causing variation. In our work,5, 6 we avoid missense mutations (rare variants in genes suspected to cause disease because they are private to the individual being studied) unless there is a measureable effect of the mutation (frameshift to affect RNA or protein for example). Our preference is for modeling small variants that cause stop or frameshift mutations, because these are easier to edit and cause a measurable output in the cell. Finally, the degree of quality control parameters (how many and how good to the cells look), the number of independent clones used, whether or not output measures are confirmed by gene edited cell lines, and the effect size of the output measure are further factors that influence people's opinions on sample number. Currently, in studies using standard tools and low clone numbers and with no genetic engineering, the expectation is for at least three unrelated subjects.
2.4. Genetic engineering strategy
Genetic engineering provides the necessary tools to adequately control cell‐based experiments in NDD studies. Key issues include achieving the right editing event in a genome that reflects the founder genome. For general review and background of general issues, see Reference 7.
Genetic engineering imposes significant cell stress due to technical procedures needed to get nucleases, gRNAs, and template DNA into a cell. iPSCs are the most commonly used cells to edit, but have a higher rate of anomalies due to genomic instability,8 which can be exasperated by replication stress due to single cell plating9 often used for genetic engineering to achieve clonality. General good practice is to minimize expansion and purification of iPSCs to avoid the possibility of acquiring often well‐known karyotypic anomalies, particularly aneuploidy in late passage iPSCs.10 We have suggested performing simultaneous reprogramming and gene editing, which allows for electroporation to be done in somatic cells.11 The rationale for this is that it takes advantage of the low probability of reprogramming (~2%‐4% of somatic cells) to achieve clonality on low‐density plates. Colonies derived from single cells can be isolated and expanded, then sequenced for editing events. Successful desired events from selected colonies can then be grown and assessed for QC measures.
Off‐target effects of genome editing are infrequent12 (though this can depend on nucleases chosen, eg Reference 13), but can drastically affect data interpretation if not adequately addressed. Current thinking is that some off‐target effects are tolerable14; however, the use of specific tools such as DISCOVER‐Seq15 remain important to characterize potential events.
For genetic engineering in NDD studies, either induction of a mutation in control cells or repairing of a mutation in disease cells can be used. Diseases that are caused by hetero‐ or hemi‐zygous loss‐of‐function are the easiest to model in control cells, since they involve nonhomologous end‐joining (NHEJ) after nuclease‐induced strand breaks on one allele, as opposed to homology directed repair (HDR) that requires template DNA, as well as nucleases and gRNAs. For disease caused by reduced dosage of either one or both alleles, the goal is not necessarily to recreate a specific patient mutation but rather to take advantage of CRISPR technology, which is accurate but not specific, to select for clones that have the outcome of interest, that is, reduced mRNA levels. Since disease mechanism is often not known, interpretation of data should be tempered with these disease models made from healthy cells. While the assumption is that making cells with reduced dosage approximates disease, it may be that the specific mutations observed in patients that also cause reduce dosage are in fact important, even if nothing can be explicitly gleaned from categorizing all known patient mutations and their clinical phenotype. It may be that CRISPR‐induced mutations are hypomorphic, or show a more severe phenotype that what would be observed in the true disease population. Still, engineering frameshifts to create nonsense products are relatively straightforward for diseases predicted to be caused by reduced dosage. Desired changes often can be identified in 5 to 10 clones.
Repairing patient mutations is a holy grail for most NDD studies, but is significantly more difficult than inducing the disease in healthy controls cells. The power of HDR is that it allows for “repair” of a patient mutation, providing the critical isogenic experiment to ensure accurate interpretation of data. As mentioned, HDR requires gRNA‐guided nuclease strand breaks and template DNA that must occur at the sample place and time for the event to occur. This low efficiency is the reason for the difficulty of this approach, though there are many groups attempting to increase the probability of gRNA, nucleases, and template DNA occurring together at a given genomic locus.16 In our experience, we screen >5X as many clones when using HDR compared with NHEJ to identify a desired genotype which can be anywhere from 50 to 100 clones.
2.5. Somatic cell source
Difficulties and troubleshooting for stem cell derivation have been reviewed and more information can be found here.17 While routine, it requires significant infrastructure and expertise to do properly to avoid common, preventable problems. For NDDs, the first challenge after patient identification is acquiring somatic cells and this may require international recruitment and collaboration with affected families that have often established charitable foundations related to disease. In almost all of our studies, we have acquired cells that have required local partners in distant places and careful shipping procedures.
Standard cell types include blood, urine, and skin, all of which have limitations18: urine is least invasive at collection but is probably the most sensitive to failure due to the low number of transformable cells (~1 per 2 mL). This process requires >30 mL of urine, a centrifuge at collection, freezing media, and dry ice. Once renal epithelial lines are established, the cells grow quickly and reprogram well. Blood requires staff to safely perform a blood draw. We require 5 to 10 mL of blood in ethylenediaminetetraacetic acid tubes, with shipment on ice. Skin cells require minor surgery so need a medical doctor on‐site. Hair and saliva have been used but are highly unreliable, so should be avoided. We have successfully expanded peripheral blood mononuclearcytes (PBMCs; blood) and renal epithelial cells (RECs; urine) from overseas patients and family members, and made iPSCs from these cells. This requires substantial QC in‐house to optimize all procedures and reagents prior to recruitment.
There are often questions about comparability across somatic cell tissues as potential sources of variation; specifically, might deriving stem cells from different tissues affect cell phenotype detection, and might even small effects bias a study with small sample sizes? While there are no extensive studies comparing iPSCs from human blood, skin, and urine, there has been extensive work done comparing embryo‐derived stem cells to iPSCs,19 and iPSCs from different mouse derived tissues.20 The general consensus is that iPSCs do retain an epigenetic memory of cell‐of‐origin but that this disappears after early passages (4‐5).19 We make every effort to remain consistent in cell type of origin to minimize potential variation, but suspect that there may be little difference if this were not done.
2.6. Sex and age of recruited subjects
Sex of recruited subjects is a potential confound, and in studies with low sample number this could be problematic. The first protection against sex‐effects is a sample set design where subjects are not necessarily pooled groups of cases and controls, but rather studied as groups of pairs (eg, female patient compared with her own sister, gene edited line compared with healthy isogenic line, drug exposed compared with no drug exposed), then looking for consistency across independent samples. Second, provided diseases are not sex‐linked, it is possible and even likely for some diseases that mutational effects are so strong that secondary issues related to sex chromosomes may not matter. This is dependent on effect size of a given cell phenotype, but given that most neurological disease do not have skewed sex ratios (ie, affect equally males and females) it is reasonable to think that sex does not affect cell phenotypes related to mutations. For example, detection of Huntington's disease cell phenotypes in iPSC‐derived cells across different laboratories and multiple subjects showed similar effects independent of sex.21 The critical concept seems to be an a priori understanding of what to look for, usually based on the function of a mutant gene, or known pathology in humans.
There is no reason to think that using samples from people of different ages will increase variation in the experiment. Reprogramming cells with Yamanaka factors, OCT4, SOX2, KLF4, and CMYC returns cells to a stem cell state that is indistinguishable from ES cells after 4 to 5 passages. “Cellular age” is thought be maintained using transdifferentiation or direct induction techniques (see next section); however, epigenetic reprogramming is a main function of Yamanaka factors. Age of participant is thus unlikely to drive increased variation provided cells are reprogrammed to a stem cell‐like state. Using a control mother and her affected daughter for example, is thus a reasonable strategy.
2.7. Potential for the use of small molecules to induce or reverse disease
In vitro iPSC‐based cell modeling requires multiple lines of proof to protect against the potential for artifactual signals. While completely dependent on the gene of study, agonists or antagonists that directly affect the mutant or absent protein of interest or which have a known effect on some part of the pathway in which the protein is found can provide important information to triangulate evidence. Choosing a disease to study which could be amenable to pharmacological manipulation is helpful, if possible. That said, almost all molecules usually come with off‐target effects; for example, we use the drug UNC0642 in healthy neural progenitor cells (NPCs) to recapitulate EHMT1 deficiency (to model Kleefstra Syndrome) since the drug is a well‐known EHMT1 protein inhibitor. We thus knew before beginning the project that we could take advantage of this drug to recapitulate any disease phenotypes in healthy cells treated with this drug. Problems with this drug are common to this type of approach—(a) it is known to inhibit EHMT2, and (b) choosing the correct dose to actually mimic disease is rarely trivial. Still, once a cell phenotype is associated with a given mutation, one can either recapitulate disease in a control cells with (usually) an antagonist of the said protein, or attempt to rescue heterozygous mutations by using an agonist drug if wildtype protein is present. Critical here is that a cell phenotype has been identified already and that the same cell phenotype can be identified in the drugged cells, with expected effects on direction of cell phenotype. This implies that pharmacological approaches were done as secondary experiments to complement a discovery made in patient disease cells.
3. IDENTIFICATION AND SELECTION OF NEURAL POPULATIONS
Stem cell derivation22, 23 and quality control24 options including the best ways to assess genomic integrity25 have been reviewed many times, so I focus here on neural differentiation and issues for neurodevelopmental disease research. Once iPSCs have been made and carefully validated, one can begin to think about the optimal way to make neuron‐like cells.
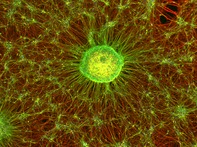
Once a stem cell state has been achieved, cells can be maintained or differentiated into different neural cell types. This is a big field and decisions are intricately linked to the disease being studied with respect to cell type and purity of cell cultures. Induction method, length of exposure time to different molecules, and differentiation parameters are all important and an in‐depth discussion can be found here.26 The main issue for the study of NDDs is ensuring the induction technique is consistent across samples since in some cases the mutation itself could affect neuronal differentiation. These can only be detected with careful monitoring of outcomes and highly reproducible standard operating procedures.
3.1. Transdifferentiation, direct induction, or developmental reprogramming?
Transdifferentiation refers to the induction of a somatic cell directly to a cell of interest while developmental reprograming refers to recapitulating developmental timing and factors in stem cells to make a cell‐type of interest. Direct induction is between these two, where stem cells are directly induced to a particular cells state, usually bypassing progenitor‐like states. Transdifferentiation usually involves using one or more transcription factors known to be present at a critical developmental time; for example, ectopic expression of ASCL1 in skin cells can transdifferentiate fibroblasts to neuron‐like cells,27 where ASCL1 is a master regulator gene normally present in neural progenitor cells. Direct induction of neurons from stem cells can be done via NGN2,28 where neurons can be made in 2 weeks. Developmental reprogramming is a longer process but involves attempting to recapitulate sequential steps and factors in neurodevelopment. Developmental reprogramming takes the most time but should probably be considered the default option for most NDD studies. Only this procedure leads to neural progenitor cells (multipotent cells that can give rise to many CNS cell types such astrocytes and neuronal subtypes) and washes away via Yamanaka factors the original epigenetic patterning in the somatic cell. The other two procedures are terminal, whereby cells are directly transformed into what will become postmitotic cells. While no in vitro procedure can ever be perfect, one would assume that to model most neurodevelopmental disorders one should attempt to best recapitulate neurodevelopment. By using the closest technique available to recapitulate neurodevelopment allows for identification of earliest cell phenotypes. The critical early phenotypes can be missed if jumping directly to a postmitotic cell state using transdifferentiation or direct induction, even if other phenotypes are identified in mature cells. That said, developmental reprogramming is the longest and most expensive of the techniques, and likely leads to more heterogeneous cell populations since cells are exposed to more factors and the procedure takes longer—both of which are variables that will allow for nondesired differentiation. NGN2‐based techniques are popular because they are done on a short time frame and lead to a relatively pure population of cells. Careful thought needs to be given to the trade‐offs between different approaches.
3.2. Purity of neural progenitor cells after developmental reprogramming
Neuronal induction from iPSCs is a 2‐ to 3‐ week process where cells need to be selected and purified in some form (for specific details of induction see: http://bio-protocol.org/e3188). Stem cells induced to neural progenitor cells are rarely uniform29, 30 so selection methods are critical. Fluorescence activated cell sorting (FACS) methods are common selecting for the presence of some markers and the absence of others (eg, CD184+/CD44−/ CD271−/CD24+ cells), but these require antibodies, a FACS machine, and the ability to regrow clean cultures after sorting. We favor a selective adhesion technique that purifies NPCs via preferential adhesion of NPCs and attachment of non‐NPC cells.11 Proper reagents can avoid spontaneous differentiation to nonectodermal lineages, mostly because the use of dual SMAD inhibition is a strong neuroectodermal driver31; however, after this stage other molecules are required to further pattern cells, and many difficulties can arise around selecting for or against neural crest, forebrain, midbrain, or hindbrain cells. For example, a slight increase in a GSK3b inhibitor drives cells to a hindbrain cell fate, rather than a midbrain cell fate,32 where the molecule is required for both cell types but at different doses, and where all other reagents are identical. This reflects fundamental biology of neurodevelopment,33 and is probably the main reason so many difficulties arise (ie, specific morphogenic dose at the right time and place is needed for cell fate specification). Another related problem is the difficulty in separating neural crest (NC) progenitors from CNS progenitors, where NC cells (observed as flat, larger cells) are usually immediately adjacent to neural rosettes so can often contaminate a forebrain culture34, 35 since they seem to proliferate more quickly than neural progenitors.
The critical issue is not the quest for ultimate cell purity, but the characterization of what has been made provided some baseline level of purity is attained. Cultures are unlikely ever to be perfectly pure at least using today's techniques, but the uniformity of cell content should be consistent across cases and controls. For example, the creation of dopaminergic cells for clinical use in monkeys to alleviate Parkinson‐like symptoms are cells that are 60% to 80%36—positive for Tyrosine Hydroxylase, an important marker of dopaminergic cells, across cell cultures derived from different subjects. The expectation is that cell lines across an experiment show a level of purity that is consistent and reproducible.
3.3. Purity of postmitotic cells derived from NPCs
Purification of a committed progenitor (NPC) is usually the main determinant of quality of more mature cells. That said, more patterning agents are required to differentiate neurons and so postmitotic cells also need to be assessed for uniformity. Variability is often high across mature neuronal cell cultures, and identical to the assessment of progenitors, the important step is to characterize levels of variation across statistically comparable pairs. For example, forebrain cultures made from NPCs that were developmentally reprogrammed are almost always a mixture of GABAergic, glutamatergic, and glial cells with ratios of about 3:6:1, respectively. What level of variation is tolerable in this ratio is really the key experimental design question rather than ensuring purity of a given cell type. We expect that as techniques improve in neural differentiation, culture purity and experimental control will only improve. The most comprehensive examples of postmitotic neuron purity can be found in the literature from midbrain dopaminergic neurons of the A9 type, resembling those dopamine‐producing cells from the substantia nigra, since significant resources have been deployed to attempt to make transplantable cells to treat Parkinson's disease.37 What is reassuring from this literature is not that cell purity has reached 100% for dopamine‐producing cells, but that the technology development that has been fostered by active investigations suggest a clear trajectory toward improved cell purity.
3.4. Length of differentiation time for neuron‐like cells derived from NPCs
How long should neurons be differentiated for from an NPC state? We favor an operational definition (https://bio-protocol.org/e3188) whereby neuron cultures are postmitotic (ie, very limited cell division present), clear networks have formed, and selected cells fire spontaneous action potentials consistent with neuronal type. Cells made from stem cells mostly resemble fetal cells38 so even long‐term differentiation is of questionable value, although neuronal features do increase with longer differentiation time (eg, increased amplitude of action potentials), which may be important particularly if electrophysiological measures are used as a read‐out. Different labs using different but related reagents have very different maturational times, so defining output measures is critical for each study.
Organoids (long differentiated NPCs that proliferate and differentiate as self‐adhering, free‐floating cells and begin to form tissue‐like structures) provide one promising avenue for neuronal maturation, and complete review can be found here.39 While the technique is promising in some specific applications,40 our own experience as well as work from others41 suggests variation across organoids is extensive. We consider organoids to be best used as a secondary validation of an identified cell phenotype, though this will likely change as techniques continue to improve.
4. PHENOTYPIC ANALYSIS
Studying NDDs can be difficult because mutations in some genes that cause neurodevelopmental disorders can be important in multiple biological systems, and may even be important in cell reprogramming, stem cell maintenance, or cell differentiation. Many NDDs are multi‐tissue, likely reflecting global importance of a particular gene. For example, there are several NDDs of the epigenetic machinery (eg, Kabuki or Kleefstra syndrome), where genes such as KMT2D, mutations in which cause Kabuki syndrome, are known for their role in cell fate transitions but not stem or progenitor maintenance.42 Their role in brain is unknown, but children with KMT2D mutations have intellectual disability, suggesting a specific role in neurons providing a rationale to model the disease in iPSC‐derived brain‐like cells. Other genes such as EHMT1, mutations in which cause Kleefstra syndrome, may be important in stem cell induction,43 thus might actually result in difficulties in differentiation to neurons due to EHMT1's role in turning off pluripotency factors,44 which could impact experimental outcomes in cell models. An understanding about what is known about genes from different fields (eg, cancer) can significantly affect interpretation of data and initial study design. Becoming aware of the molecular machinery important for stem cell reprogramming, maintenance, and induction is essential.
It is possible that in vitro procedures expose new phenotypes that do not exist during natural human development when stem cells with mutations in these genes are investigated, leading to potentially “true” effects but with no relevance to human disease biology. One option to address this is to select a disease where the mutation of interest is in a gene not known to be expressed in stem cells. For example, NDDs caused by mutations in genes coding for synapse‐related proteins (eg, GRIN2B, SHANK1) are unlikely to cause cellular deficits in reprogramming or even neural induction since these genes are typically expressed only in more mature neurons. In short, one needs to be extremely careful in interpreting “phenotype” since mutations of interest could cause a host of unintended effects, including reproducible effects with drastic changes to fundamental properties of cells that could persist throughout development.
Once neuronal cell lines are established and quality assessed, the most interesting part of a project can begin—finding cell phenotypes associated with a given mutation. As with most projects in the life sciences, these experiments tend to follow high or low throughput approaches, where high throughput approaches include transcriptomic, proteomic, or metabolomic profiling; and low throughput approaches tend to target specific molecules that might plausibly be associated with the protein made from the mutated gene. Whatever the approach, it will be the parallel cell lines independently matched to different control cells that will allow for confirmation of a cell or molecular phenotype of interest.
5. DRUG SCREENING IN IPSC‐DERIVED CELLS FOR TRANSLATIONAL MEDICINE
An identified cell phenotype that is associated with disease model cells is required before drug screening is attempted. There are several reviews on assay development prior to embarking on drug screening projects, as reviewed here.3, 45 High throughput screens using iPSC‐derived cells are a well‐explored avenue and an interesting option provided an excellent cell read‐out is available. For some diseases, a cell phenotype may be amenable to application of a specific set of already approved drugs that might immediately be available for testing. For example, in the case of Fragile X syndrome (FXS), a severe neurodevelopmental disorder, mutations in mouse Fmr1 are thought to increase mRNA translation46 via decreased repression through Eif4e and other factors. In other words, aberrant translation is a potential molecular output of the disease as modeled in mouse. Metformin, a drug for diabetes, is known to increase translational repression and seems to ameliorate FXS in mouse.47 An experiment to perform then, prior to testing metformin in children, is to determine metformin effects on protein translation in iPSC‐derived neurons from children with FXS.
5.1. Preclinical testing of ASOs for gain‐of function mutation syndromes
Antisense oligonucleotides (ASOs) are short stretches of DNA, 15 to 50 nucleotides long that bind to complementary mRNAs, creating a complex that can be recognized by endogenous RNase H and degraded, or that can block translation or splicing by steric hindrance.48, 49 ASOs can efficiently decrease mRNA levels and subsequent protein levels from a targeted mRNA. They have been used as drug treatments for several dominant, gain‐of‐function diseases. Over 50 ASOs are in or have been in clinical trials for various diseases in humans,50, 51, 52, 53 including spinal muscular atrophy (SMA; targeting SMN2), which was approved for clinical use in children in 2016.54
ASOs have a remarkable ability to enter the CNS after intrathecal delivery, distributing widely through the brain55, 56 and are taken up by neurons.48, 57 Intrathecal delivery, infusion into the spinal cord, is the most commonly used delivery method to treat neurological disorders by ASO, and is the FDA‐approved method for the ASO used to treat SMA. Delivery of a therapeutic payload has long been a critical problem for any form of gene therapy, yet oligonucleotides enter the cortex after intrathecal infusion and have not shown an immune reaction at therapeutically relevant doses. That said, ASOs require chemical modifications to maximize their stability and this needs to be assessed for any new ASO being developed. Furthermore, each ASO that targets a particular gene is different so each one needs to be carefully assessed in vitro and in vivo to understand its half‐life and knockdown efficiency, and tissue distribution after intrathecal infusion. Importantly, several pioneering trials, most notably in Huntington's disease, where ASO targeting mRNA from HTT have been optimized (dose, concentration, time, delivery) in primates55 and humans,58 and can form a template for other disorders, including that for only a single patient, one example of which recently had minor but significant improvements59 in a child with an NDD.
6. CONCLUSIONS
Neurodevelopmental diseases are a specialized category of stem cell modeling and therefore require specialized experimental design. Explicit plans in the pre‐experiment phase, careful selection of cell lines, attention to differentiation protocols and reasonable choices related to cell purity of end stage cells are critical to detection of cell phenotypes that might then be used in preclinical drug discovery assays.
CONFLICT OF INTEREST
The author declared no potential conflicts of interest.
Ernst C. A roadmap for neurodevelopmental disease modeling for non‐stem cell biologists. STEM CELLS Transl Med. 2020;9:567–574. 10.1002/sctm.19-0344
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Takahashi K, Tanabe K, Ohnuki M, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861‐872. [DOI] [PubMed] [Google Scholar]
- 2. Hirschi KK, Li S, Roy K. Induced pluripotent stem cells for regenerative medicine. Annu Rev Biomed Eng. 2014;16:277‐294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Engle SJ, Blaha L, Kleiman RJ. Best practices for translational disease modeling using human iPSC‐derived neurons. Neuron. 2018;100:783‐797. [DOI] [PubMed] [Google Scholar]
- 4. Simons VC. Simons Variation in Individuals Project (Simons VIP): a genetics‐first approach to studying autism spectrum and related neurodevelopmental disorders. Neuron. 2012;73:1063‐1067. [DOI] [PubMed] [Google Scholar]
- 5. Bell S, Maussion G, Jefri M, et al. Disruption of GRIN2B impairs differentiation in human neurons. Stem Cell Reports. 2018;11:183‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bell S, Rousseau J, Peng H, et al. Mutations in ACTL6B cause neurodevelopmental deficits and epilepsy and lead to loss of dendrites in human neurons. Am J Hum Genet. 2019;104:815‐834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bassett AR. Editing the genome of hiPSC with CRISPR/Cas9: disease models. Mamm Genome. 2017;28:348‐364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Henry MP, Hawkins JR, Boyle J, et al. The genomic health of human pluripotent stem cells: genomic instability and the consequences on nuclear organization. Front Genet. 2018;9:623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lamm N, Ben‐David U, Golan‐Lev T, Storchová Z, Benvenisty N, Kerem B. Genomic instability in human pluripotent stem cells arises from replicative stress and chromosome condensation defects. Cell Stem Cell. 2016;18:253‐261. [DOI] [PubMed] [Google Scholar]
- 10. Taapken SM, Nisler BS, Newton MA, et al. Karotypic abnormalities in human induced pluripotent stem cells and embryonic stem cells. Nat Biotechnol. 2011;29:313‐314. [DOI] [PubMed] [Google Scholar]
- 11. Bell S, Peng H, Crapper L, et al. A rapid pipeline to model rare neurodevelopmental disorders with simultaneous CRISPR/Cas9 gene editing. Stem Cells Transl Med. 2017;6:886‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Veres A, Gosis BS, Ding Q, et al. Low incidence of off‐target mutations in individual CRISPR‐Cas9 and TALEN targeted human stem cell clones detected by whole‐genome sequencing. Cell Stem Cell. 2014;15:27‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grunewald J, Zhou R, Garcia SP, et al. Transcriptome‐wide off‐target RNA editing induced by CRISPR‐guided DNA base editors. Nature. 2019;569:433‐437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carroll D. Collateral damage: benchmarking off‐target effects in genome editing. Genome Biol. 2019;20:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wienert B, Wyman SK, Richardson CD, et al. Unbiased detection of CRISPR off‐targets in vivo using DISCOVER‐Seq. Science. 2019;364:286‐289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aird EJ, Lovendahl KN, St Martin A, et al. Increasing Cas9‐mediated homology‐directed repair efficiency through covalent tethering of DNA repair template. Commun Biol. 2018;1:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shi Y, Inoue H, Wu JC, Yamanaka S. Induced pluripotent stem cell technology: a decade of progress. Nat Rev Drug Discov. 2017;16:115‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Raab S, Klingenstein M, Liebau S, et al. A comparative view on human somatic cell sources for iPSC generation. Stem Cells Int. 2014;2014:768391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bilic J, Izpisua Belmonte JC. Concise review: Induced pluripotent stem cells versus embryonic stem cells: close enough or yet too far apart? Stem Cells. 2012;30:33‐41. [DOI] [PubMed] [Google Scholar]
- 20. Polo JM, Liu S, Figueroa ME, et al. Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat Biotechnol. 2010;28:848‐855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Consortium HDi . Induced pluripotent stem cells from patients with Huntington's disease show CAG‐repeat‐expansion‐associated phenotypes. Cell Stem Cell. 2012;11:264‐278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rossant J, Tam PPL. New insights into early human development: lessons for stem cell derivation and differentiation. Cell Stem Cell. 2017;20:18‐28. [DOI] [PubMed] [Google Scholar]
- 23. Schlaeger TM, Daheron L, Brickler TR, et al. A comparison of non‐integrating reprogramming methods. Nat Biotechnol. 2015;33:58‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. D'Antonio M, Woodruff G, Nathanson JL, et al. High‐throughput and cost‐effective characterization of induced pluripotent stem cells. Stem Cell Reports. 2017;8:1101‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Assou S, Bouckenheimer J, De Vos J. Concise review: assessing the genome integrity of human induced pluripotent stem cells: what quality control metrics? Stem Cells. 2018;36:814‐821. [DOI] [PubMed] [Google Scholar]
- 26. Tao Y, Zhang SC. Neural subtype specification from human pluripotent stem cells. Cell Stem Cell. 2016;19:573‐586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chanda S, Ang CE, Davila J, et al. Generation of induced neuronal cells by the single reprogramming factor ASCL1. Stem Cell Reports. 2014;3:282‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhang Y, Pak C, Han Y, et al. Rapid single‐step induction of functional neurons from human pluripotent stem cells. Neuron. 2013;78:785‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Elkabetz Y, Panagiotakos G, Al Shamy G, et al. Human ES cell‐derived neural rosettes reveal a functionally distinct early neural stem cell stage. Genes Dev. 2008;22:152‐165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Golebiewska A, Atkinson SP, Lako M, Armstrong L. Epigenetic landscaping during hESC differentiation to neural cells. Stem Cells. 2009;27:1298‐1308. [DOI] [PubMed] [Google Scholar]
- 31. Chambers SM, Fasano CA, Papapetrou EP, Tomishima M, Sadelain M, Studer L. Highly efficient neural conversion of human ES and iPS cells by dual inhibition of SMAD signaling. Nat Biotechnol. 2009;27:275‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xi J, Liu Y, Liu H, Chen H, Emborg ME, Zhang SC. Specification of midbrain dopamine neurons from primate pluripotent stem cells. Stem Cells. 2012;30:1655‐1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wolpert L. Positional information and the spatial pattern of cellular differentiation. J Theor Biol. 1969;25:1‐47. [DOI] [PubMed] [Google Scholar]
- 34. Muratore CR, Srikanth P, Callahan DG, Young‐Pearse TL. Comparison and optimization of hiPSC forebrain cortical differentiation protocols. PLoS One. 2014;9:e105807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wilson PG, Stice SS. Development and differentiation of neural rosettes derived from human embryonic stem cells. Stem Cell Rev. 2006;2:67‐77. [DOI] [PubMed] [Google Scholar]
- 36. Kikuchi T, Morizane A, Doi D, et al. Human iPS cell‐derived dopaminergic neurons function in a primate Parkinson's disease model. Nature. 2017;548:592‐596. [DOI] [PubMed] [Google Scholar]
- 37. Barker RA, Studer L, Cattaneo E, et al. G‐Force PD: a global initiative in coordinating stem cell‐based dopamine treatments for Parkinson's disease. NPJ Parkinsons Dis. 2015;1:15017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hrvatin S, O'Donnell CW, Deng F, et al. Differentiated human stem cells resemble fetal, not adult, beta cells. Proc Natl Acad Sci U S A. 2014;111:3038‐3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Di Lullo E, Kriegstein AR. The use of brain organoids to investigate neural development and disease. Nat Rev Neurosci. 2017;18:573‐584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Watanabe M, Buth JE, Vishlaghi N, et al. Self‐organized cerebral organoids with human‐specific features predict effective drugs to combat Zika virus infection. Cell Rep. 2017;21:517‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Camp JG, Badsha F, Florio M, et al. Human cerebral organoids recapitulate gene expression programs of fetal neocortex development. Proc Natl Acad Sci U S A. 2015;112:15672‐15677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang C, Lee JE, Lai B, et al. Enhancer priming by H3K4 methyltransferase MLL4 controls cell fate transition. Proc Natl Acad Sci U S A. 2016;113:11871‐11876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chen J, Liu H, Liu J, et al. H3K9 methylation is a barrier during somatic cell reprogramming into iPSCs. Nat Genet. 2013;45:34‐42. [DOI] [PubMed] [Google Scholar]
- 44. Liu N, Zhang Z, Wu H, et al. Recognition of H3K9 methylation by GLP is required for efficient establishment of H3K9 methylation, rapid target gene repression, and mouse viability. Genes Dev. 2015;29:379‐393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Corti S, Faravelli I, Cardano M, Conti L. Human pluripotent stem cells as tools for neurodegenerative and neurodevelopmental disease modeling and drug discovery. Expert Opin Drug Discov. 2015;10:615‐629. [DOI] [PubMed] [Google Scholar]
- 46. Gkogkas CG, Khoutorsky A, Cao R, et al. Pharmacogenetic inhibition of eIF4E‐dependent Mmp9 mRNA translation reverses fragile X syndrome‐like phenotypes. Cell Rep. 2014;9:1742‐1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gantois I, Khoutorsky A, Popic J, et al. Metformin ameliorates core deficits in a mouse model of fragile X syndrome. Nat Med. 2017;23:674‐677. [DOI] [PubMed] [Google Scholar]
- 48. Wild EJ, Tabrizi SJ. Therapies targeting DNA and RNA in Huntington's disease. Lancet Neurol. 2017;16:837‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Roovers J, De Jonghe P, Weckhuysen S. The therapeutic potential of RNA regulation in neurological disorders. Expert Opin Ther Targets. 2018;22:1017‐1028. [DOI] [PubMed] [Google Scholar]
- 50. Miller TM, Pestronk A, David W, et al. An antisense oligonucleotide against SOD1 delivered intrathecally for patients with SOD1 familial amyotrophic lateral sclerosis: a phase 1, randomised, first‐in‐man study. Lancet Neurol. 2013;12:435‐442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Skotte NH, Southwell AL, Østergaard ME, et al. Allele‐specific suppression of mutant huntingtin using antisense oligonucleotides: providing a therapeutic option for all Huntington disease patients. PLoS One. 2014;9:e107434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Finkel RS, Chiriboga CA, Vajsar J, et al. Treatment of infantile‐onset spinal muscular atrophy with nusinersen: a phase 2, open‐label, dose‐escalation study. Lancet. 2016;388:3017‐3026. [DOI] [PubMed] [Google Scholar]
- 53. Tabrizi SJ, Leavitt BR, Landwehrmeyer GB, et al. Targeting Huntingtin Expression in Patients with Huntington's Disease. N Engl J Med. 2019;380(24):2307‐2316. 10.1056/NEJMoa1900907. [DOI] [PubMed] [Google Scholar]
- 54. Hoy SM. Nusinersen: first global approval. Drugs. 2017;77:473‐479. [DOI] [PubMed] [Google Scholar]
- 55. Kordasiewicz HB, Stanek LM, Wancewicz EV, et al. Sustained therapeutic reversal of Huntington's disease by transient repression of huntingtin synthesis. Neuron. 2012;74:1031‐1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Smith RA, Miller TM, Yamanaka K, et al. Antisense oligonucleotide therapy for neurodegenerative disease. J Clin Invest. 2006;116:2290‐2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gherardini L, Bardi G, Gennaro M, Pizzorusso T. Novel siRNA delivery strategy: a new "strand" in CNS translational medicine? Cell Mol Life Sci. 2014;71:1‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. van Roon‐Mom WMC, Roos RAC, de Bot ST. Dose‐dependent lowering of mutant Huntingtin using antisense oligonucleotides in Huntington disease patients. Nucleic Acid Ther. 2018;28:59‐62. [DOI] [PubMed] [Google Scholar]
- 59. Kim J, Hu C, Moufawad El Achkar C, et al. Patient‐customized oligonucleotide therapy for a rare genetic disease. N Engl J Med. 2019;381:1644‐1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


