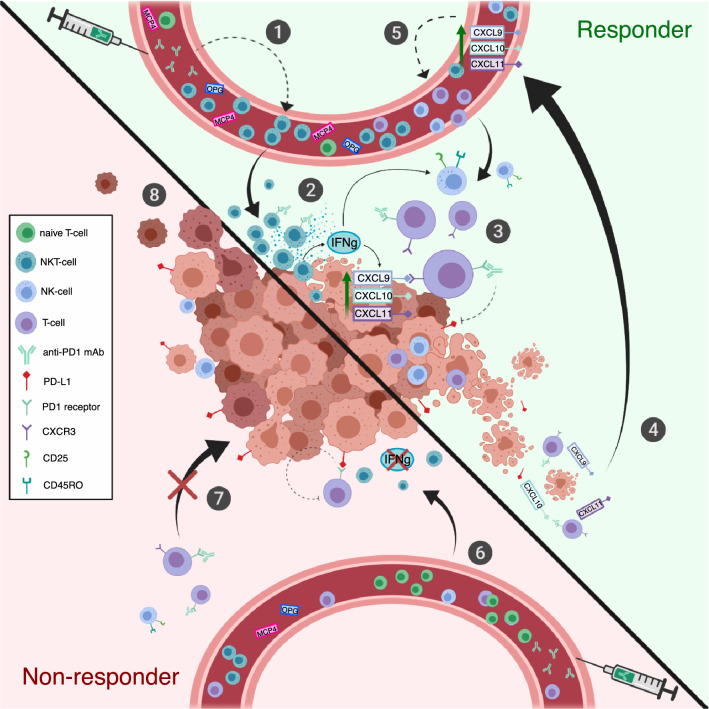
Fig. 6.
Putative role of observed immunological changes in responders and non-responders. (1) The frequency of PB NKT cells is higher and naïve T cells lower in the responders after initiation of anti-PD1 treatment. (2) NKT cells are able to produce large quantities of IFNγ, a known activator of other lymphocytes, such as cytotoxic NK- and T cells. IFNγ has also been previously shown to induce the production of CXCL9, -10, and -11 chemokines in tumor microenvironment. (3) CXCL9, -10, and -11 are known to induce T-cell migration and infiltration into tumor via CXCR3 interaction. Anti-PD1 treatment blocks the inactivating binding of PD-L1 to its receptor on the surface of cytotoxic T-cell enabling the antitumor immune response. (4) CXCR3 ligands (CXCL9, -10, and -11) could be released into circulation as a result of tumor cell lysis, which may further enhance the loop by (5) attracting lymphocytes to the tumor site. Further, the responders have increased levels of serum OPG and MCP4, which are cytokines associated with age; however, their role in positive response to anti-PD1 requires further studies. (6) Non-responders have less circulating NKT cells, thus the production of IFNγ may be insufficient in activating other lymphocytes and inducing the production of CXCR3 ligands in the tumor microenvironment. (7) Without chemokine attraction, the cytotoxic T cells may not be able to migrate to the tumor site, leading to (8) insufficient antitumor immune response, tumor growth and disease progression