Editor—Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome (SARS-CoV-2) infection, has particularly involved intensivists and the intensive care community worldwide.1 Arterial hypertension has been reported as one of the most common cardiovascular comorbidities in COVID-19 patients.2 Investigators have identified an association between pre-existing hypertension and ICU admission in COVID-19 patients.3 , 4 We performed a brief systematic review and meta-analysis to evaluate the risk of ICU admission in hypertensive patients with COVID-19. Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines, we searched MEDLINE, Scopus, and Web of Science for all investigations in English published any time up to March 27, 2020, and reporting data on COVID-19 patients with hypertension admitted to ICU. The identification of studies to be included in our analysis was independently conducted by two authors (LR and GR) in a blinded fashion. Any discrepancy in study selection was resolved in consultation with a third author (MZ). The following MeSH terms were used for the search: ‘COVID-19’ AND ‘ICU’ OR ‘hypertension’. We searched the bibliographies of target studies for additional references. Case reports review articles, abstracts, editorials/letters, and case series with less than 10 participants were excluded. Studies that compared the prevalence of arterial hypertension between hospitalised patients who required ICU care and those who did not were included in the meta-analysis. The quality of included studies was graded using the Newcastle–Ottawa quality assessment scale (NOS).3 Data were pooled using the Mantel–Haenszel random-effects models with odds ratio (OR) as the effect measure with the related 95% confidence interval (CI). Statistical heterogeneity between groups was measured using the Higgins I 2 statistic. To evaluate publication bias, if any, Egger's test was performed to assess asymmetry of the funnel plot. Analyses were carried out using Review Manager 5.2 (Cochrane Collaboration, Oxford, UK).
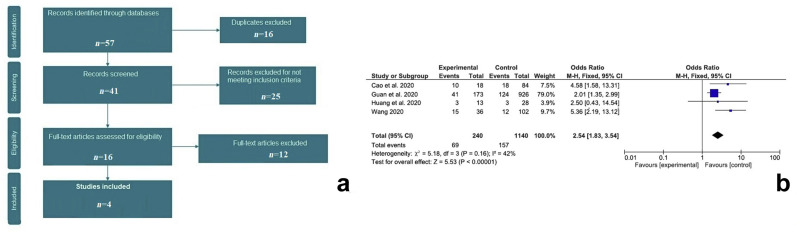
A total of 41 articles were retrieved after excluding duplicates. After initial screening, 25 were excluded for not meeting the inclusion criteria, leaving 16 articles to assess for eligibility. After evaluation of the full-text articles, 12 articles including editorial/letter, reviews, case reports, and investigations not in English were excluded. Finally, four studies (Supplementary File 1) met the inclusion criteria (Fig. 1 a).3, 4, 5, 6 Three investigation were of high quality while one was of moderate quality according to the NOS. Among the 1382 patients (mean age 51.5 yr, 798 males) included, arterial hypertension was the most frequent comorbidity. On meta-analysis, COVID-19 patients with hypertension had a significantly increased risk of ICU admission (OR=2.54; 95% CI, 1.83–3.54; P<0.0001; I 2=42%) as shown in Fig. 1b. Egger's regression test confirmed that there was no evidence of publication bias (t=1.39, P=0.299).
Fig 1.
(a) Flow diagram of selected studies for the meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). (b) Forest plot of studies investigating ICU admission in relation to arterial hypertension. CI, confidence interval.
Our brief meta-analysis suggests that hypertensive patients with COVID-19 have a greater risk of ICU admission. This has potentially important implications in clinical practice. A recent report from Italy suggests that the prevalence of arterial hypertension is significantly higher amongst COVID-19 patients admitted to ICU who do not survive.7
Our study has several limitations related to the observational nature of the studies reviewed with all inherent biases. Few investigations have examined the link between arterial hypertension and ICU admission in COVID-19 patients, limiting the number of the studies included in the meta-analysis. No formal definition of arterial hypertension was given in the included studies. The need for ICU admission may have depended on local resources that are often different between units. No adjustments for confounders were made for other risk factors such as age or other baseline cardiovascular or chronic comorbidities. All included studies were performed in China, so we cannot exclude significant differences between other populations. Because we considered only published studies in English, we cannot exclude missing some investigations with interesting findings published only in Chinese in particular. In our analysis, the degree of increased risk of ICU admission in hypertensive patients was strongly influenced by a single study, that of Guan and colleagues.2 The identification of those predictors indicating a need for intensive care admission could be helpful in managing the early phase of the pandemic both for clinical and ICU management. However, our results should be considered preliminary, and further research is necessary to confirm our findings.8
Declarations of interest
The authors declare that they have no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2020.04.056.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Arabi Y.M., Murthy S., Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. March 3, 2020 doi: 10.1007/s00134-020-05955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Liang W.H., Zhao Y. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. March 26, 2020 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao J., Hu X., Cheng W., Yu L., Tu W.J., Liu Q. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. March 2, 2020 doi: 10.1007/s00134-020-05987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. February 7, 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan W.J., Ni Z.Y., Hu Y. China medical treatment expert group for covid-19. Characteristics of coronavirus disease 2019 in China. N Engl J Med. February 28, 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grasselli G., Zangrillo A., Zanella A. COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.