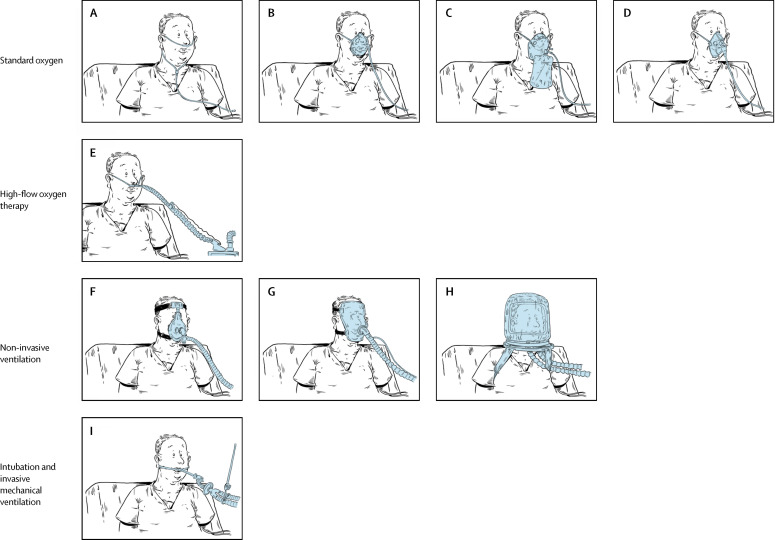
Figure 6.
Nine oxygenation and ventilation methods
Standard oxygen can be administered through a wide array of devices. Low-flow oxygen systems comprise a nasal cannula (or nasal catheters; A) providing supplemental oxygen at flows below the total minute ventilation, leading to oxygen dilution with ambient air and lowering the inspired oxygen concentration. A standard nasal cannula delivers an inspiratory FiO2 of 0·24–0·44 at supply flows 1–8 L/min, depending on respiratory rate and tidal volume. A humidification device is recommended for flows >4 L/min. Reservoir masks (B) can deliver FiO2 values of 0·40–0·60 at 5–10 L/min. The reservoir system (∼100–300 cm3) stores oxygen. A flow rate >5 L/min must be set to ensure the washout of exhaled gas and avoid CO2 retention. The non-rebreathing facemask (C) may deliver up to 0·90 FiO2 at flow settings >10 L/min. It should be used only for short periods, as humidification is difficult and there is also a risk of CO2 retention if the mask's reservoir bag is allowed to collapse on inspiration. Lastly, the Venturi system (D) mixes oxygen with room air (humidification is not necessary) and provides an accurate and constant FiO2 despite variations in respiratory rate and tidal volume. It is employed when concern arises about CO2 retention or when the respiratory drive is inconsistent. High-flow oxygen therapy through nasal prongs or cannulas (high-flow nasal oxygen therapy; E) supplies an exact FiO2 (up to 1) at a flow equal to or greater than the patient's inspiratory flow demand. Nasal oxygen is administered at a flow rate of up to 60 L/min. It is warmed to body temperature and saturated to full humidity by molecular humidification. Non-invasive positive-pressure ventilation provides ventilator support without an endotracheal tube, using an oronasal (F) or total face (G) mask or a helmet (H). The main non-invasive ventilation mode used in hypoxaemic acute respiratory failure is pressure support; continuous positive airway pressure and bi-level positive airway pressure are used less often. Finally, invasive mechanical ventilation (I) uses a tracheal tube inserted into the trachea under general anaesthesia and a neuromuscular-blocking drug. The tube is then secured to the face or neck and connected to a ventilator. In patients with hypoxaemic acute respiratory failure, intubation and invasive mechanical ventilation are used after failure of standard oxygen and, in some cases, of the aforementioned non-invasive options. FiO2= fraction of inspired oxygen.