Figure 2.
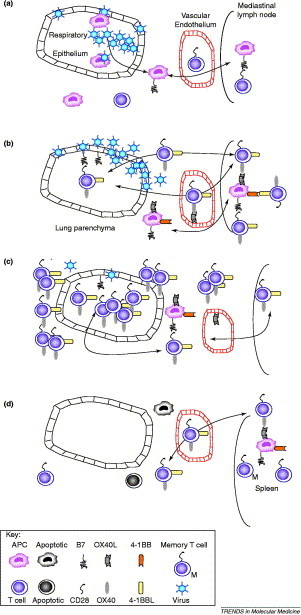
The coordinated activation of T lymphocytes during acute pulmonary viral infection. (a) Infection of the respiratory epithelium, alveolar macrophages and dendritic cells (e.g. with influenza virus or respiratory syncytial virus) causes the release of inflammatory cytokines and chemokines that recruit immune cells to the lung. Some epithelial cells that are killed during replication of the virus are ingested by antigen presenting cells (APCs). These, together with directly infected APCs, migrate to the expanding lung-associated lymph nodes (such as the mediastinal lymph node). Naïve T cells enter the lymph node from the blood and are activated by the viral antigens that are presented on APCs. The activation of T cells depends on the co-stimulatory interaction between CD28 and B7, and results in the expression of alternative chemokine receptors and adhesion molecules that facilitate the entry of activated T cells into the inflamed lung. (b) From 2–4 days after lung infection, T cells are further expanded and upregulate late co-stimulatory molecules (OX40 and possibly 4-1BB). These cells migrate to the site of viral replication via the blood. Note that inflamed endothelial cells can also express OX40L, which might facilitate the movement of OX40-expressing T cells into the lung. Once in the lung, further activation occurs through the interaction with activated APCs or epithelial cells (which can upregulate co-stimulatory molecules). (c) By days 4–8, the level of T-cell recruitment and activation is maximal. OX40 (and probably 4-1BB)-expressing T cells accumulate in and around the airways and blood vessels, disrupting their function. This, together with excessive inflammatory cytokine production, causes the clinical symptoms of infection (sweating, weight loss, cachexia and appetite suppression). (d) If the virus is eliminated and the patient survives, by day 8–18, the inflammatory infiltrate subsides (by activation-induced cell death) and the mediastinal lymph node reduces in size. Some antigen-specific cells survive this contraction process and migrate to the spleen as memory T cells. For clarity, we have omitted inducible co-stimulatory molecule (ICOS), which is induced much faster than OX40. The precise timing of co-stimulatory molecule expression is affected by the precise pathogen and dose.
