Abstract
Objectives:
Cold polypectomy (CP) is widely used because of its safety profile. This systematic review and meta-analysis aimed to clarify the indications for CP based on polyp size.
Methods:
We searched PubMed and the Cochrane Library for randomized controlled trials that compared cold snare polypectomy (CSP) and other procedures for polyps ≤10 mm. Large-scale prospective observational studies were also searched to assess delayed bleeding rates. The studies were integrated to assess the risk ratio for incomplete resection rates according to polyp size. The Cochrane risk of bias tool was used to evaluate the study bias. The certainty of cumulative evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation system.
Results:
We found 280 articles and reviewed their eligibility. We selected and extracted 12 randomized controlled trials and 3 prospective observational studies. The risk ratio of incomplete resection of polyps ≤10 mm using CSP compared with hot snare polypectomy (HSP) was 1.36 (95% confidence interval [CI], 0.92-2.01). The risk ratio for incomplete removal using CSP compared with cold forceps polypectomy (CFP) was 0.50 (95% CI, 0.31-0.82). For polyps ≤3 mm, the risk ratio of CSP compared with CFP was 1.40 (95% CI, 0.39-4.95). Certainty of cumulative evidence was considered low. No delayed bleeding after CP was reported after the treatment of 3446 polyps.
Conclusions:
CSP and HSP may result in the same complete resection rates for polyps ≤10 mm. For polyps ≤3 mm, CFP and CSP may have the same resection rates (PROSPERO registration number: CRD42019122132).
Keywords: cold snare polypectomy, cold forceps polypectomy, colorectal cancer, colon polyp, colonoscopy, endoscopy
Introduction
Endoscopic removal of colorectal polyps is widely used to prevent future colorectal cancer. Based on the results of the National Polyp Study, removal of colorectal polyps can reduce deaths caused by colorectal cancer[1]. In addition, large-scale case-control studies and cohort studies have reported that colonoscopic interventions reduce the incidence and mortality rates of colorectal cancer[2,3].
Cold polypectomy (CP) is a polypectomy technique used to remove small polyps by mechanical transection with a polypectomy snare or forceps without high-frequency current[4]. CP has been used in daily clinical practice since the 1990s[5,6], and its safety and usefulness have been gaining attention since approximately 2010[4]. In recent years, CP has been widely used because of its safety profile. CP comprises cold snare polypectomy (CSP), which uses a polypectomy snare, and cold forceps polypectomy (CFP), which uses forceps.
Recently, trials comparing the effects and risks of CSP and hot snare polypectomy (HSP) or endoscopic mucosal resection (EMR) for colorectal polyps ≤10 mm have been reported, and systematic reviews with meta-analyses that integrated those trials have been published[7-9]. However, the polyp size was not evaluated in these studies, and no meta-analysis analyzed the influence of the polyp size. Several trials and meta-analyses comparing CSP and CFP have also been reported[11,12]; however, these did not evaluate the polyp size.
In clinical practice, we frequently encounter the question of which procedure to select based on the size of the polyp. It would be clinically useful if the indications for the procedures are clarified according to the polyp size. Therefore, we planned a systematic review and meta-analysis to evaluate incomplete resection rates and to clarify the indications for CP based on the polyp size that was not evaluated in the previous meta-analyses.
Methods
Registration
We created a research plan and registered it with PROSPERO[12], a systematic review registration system, prior to starting this research (registration number: CRD42019122132).
Eligibility criteria
We included full randomized controlled trials comparing CSP and other endoscopic procedures for polyps ≤10 mm to assess their beneficial effects and to examine their incomplete resection rates. Furthermore, we included large-scale (≥1,000 polyps) prospective cohort studies to assess delayed bleeding rates. We excluded abstracts and proceedings of medical meetings as it is challenging to obtain sufficient information.
Search strategy
We searched PubMed and the Cochrane Library. We used the following keywords in PubMed: (“polypectomy”[All Fields] or “emr”[All Fields] or ((“endoscopy”[All Fields] or “endoscopic”[All Fields]) and resection[All Fields])) and “cold”[All Fields]. In the Cochrane Library, we used the following keywords: (“cold” and “polypectomy”) or (“cold” and “resection”). We requested additional information from the corresponding authors of each article via e-mail, as necessary. The language used in the studies was restricted to English. The date of the last search was January 31, 2019.
Study selection
First, two reviewers (T.K. and Y.T.) who are endoscopists certified by the Japan Gastroenterological Endoscopy Society shared the literature list and independently evaluated the titles and abstracts. Second, the full texts of the selected literature were independently reviewed for eligibility by the same two reviewers. In the case of disagreement, the two reviewers discussed the issue and decided the eligibility.
Data extraction
We extracted the following data from each literature: study design, countries, study setting, target polyp size, interventions, endpoints, evaluation method of incomplete resection, and type of snare and forceps.
Outcomes and prioritization
The primary endpoint of this study was the incomplete resection rate according to polyp size. Incomplete resection was defined as positive pathological results at the resection site after polypectomy[13] or polyps for which R0 resection could not be performed[14]. Secondary endpoints were the polyp retrieval rate and delayed bleeding rate. The polyp retrieval rate was defined as the ratio of the specimen obtained for pathological evaluation[15]. Delayed bleeding was defined as bleeding requiring medical treatment or emergency endoscopy after examinations[4,16,17].
Risk of bias in individual studies
We estimated the risk of bias of the included studies based on the Cochrane risk of bias criteria, which comprised of selection bias, performance bias, detection bias, attrition bias, reporting bias, and others. The domain of each bias was evaluated as low risk, unclear risk, or high risk. We also used the Cochrane risk bias tool[18].
Data synthesis
If studies were sufficiently homogenous in terms of design and comparator, we conducted a meta-analysis. The risk ratios (RR), risk differences (RD), and 95% confidence intervals (CI) of outcomes (incomplete resection, tissue retrieval, and occurrence of delayed bleeding) were calculated using the Mantel-Haenszel method. Statistical heterogeneity was evaluated using the I2 statistic. Review Manager version 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark) was used to combine each outcome and assess the bias risk. The statistical review of this study was performed by a biomedical statistician (I.Y.).
Publication biases
We checked the registration websites, such as ClinicalTrials.gov (https://clinicaltrials.gov/) and the University Hospital Medical Information Network (https://www.umin.ac.jp/) to evaluate whether selective reporting of outcomes occurred.
Certainty in cumulative evidence
To judge the quality of evidence, we referenced the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology[19], using GRADEpro Guideline Development Tool (McMaster University, 2015, developed by Evidence Prime, Inc. Available from https://gradepro.org/). The quality of evidence was assessed by the domains of the risk of bias, inconsistency, indirectness, imprecision, and other considerations. The limitation of each quality domain was rated as not serious, serious, or very serious. Overall certainty of evidence was evaluated as high (further research is very unlikely to change our confidence in the estimate of the effect), moderate (further research is likely to have an important impact on our confidence in the estimate of the effect and may change the estimate), low (further research is very likely to have an important impact on our confidence in the estimate of the effect and is likely to change the estimate), or very low (any estimate of the effect is very uncertain).
Results
Study selection
Our database search yielded 280 documents for extraction. As a result of the first screening of titles and abstracts, 260 documents were excluded (Figure 1). As a result of checking the full text during the second screening, 5 articles were excluded. The reasons for exclusion were as follows: retrospective analysis[20,21] (n = 2); comparison with hot forceps biopsy[22] (n = 1); comparison with a suction pseudopolyp technique[23] (n = 1); and nonrandomized controlled trial[24] (n = 1). Finally, 12 randomized controlled trials[13-15,25-33] and 3 prospective observational studies[4,16,17] were extracted. We did not conduct funnel plot analyses for publication bias because there were fewer than 10 trials[34].
Figure 1.
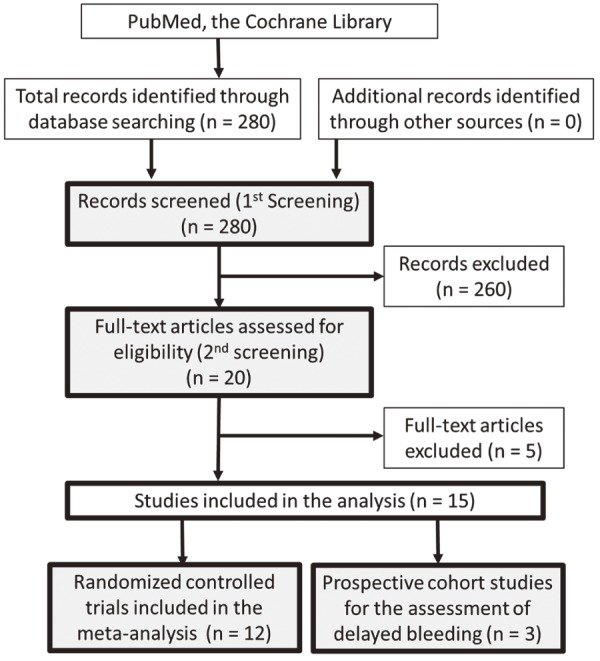
Study flow.
Characteristics of the studies
The countries in which clinical research was performed were Japan (n = 5), Korea (n = 4), Greece (n = 2), China (n = 1), Germany (n = 1), Italy (n = 1), and the United States (n = 1) (Table 1). The study comparing CSP and HSP targeted polyps ≤10 mm, whereas the study comparing CSP and CFP mainly focused on smaller polyps. In all the studies, except for that by Schett et al.[17], polyp size was estimated comparing the snare, forceps, or endoscopic measurement device. In 8 randomized controlled trials with complete or incomplete resection rates as the primary endpoint[13,25,26,29-33], the completeness of resection was evaluated by biopsy (n = 6), EMR (n = 1), or cold snaring (n = 1) at the resection site. If a biopsy, EMR, or cold snaring from the post-polypectomy ulcer showed residual tumor cells, it was defined as incomplete resection. Of the 6 studies that assessed the complete resection by biopsy, 2 studies evaluated biopsies only from the lateral margin of the post-polypectomy ulcer, and 4 studies evaluated biopsies from both the base and lateral margin of the ulcer. Of the 4 randomized controlled trials in which the primary endpoint was neither the complete or incomplete resection rate[14,15,27,28], 3 reported complete resection and evaluation of the margin of the resected specimen; however, an evaluation of the complete resection was not performed in 1 randomized controlled trial[27]. Of the 12 randomized controlled trials, only 1 used a submucosal injection when CSP was performed[25]. Of the 7 studies evaluating HSP, 3 studies did not use submucosal injections[14,15,28], 2 studies used submucosal injections (expressed as EMR)[25,26], and in the other 2 studies, whether to perform submucosal injection depended on the endoscopist's decision[13,27]. Only 1 of the 12 studies used a dedicated snare for CSP[25], and jumbo forceps were used in only 1 study[29] evaluating CFP (Table 2).
Table 1.
Study Characteristics.
| First Author | Year | Study Design | Country | Study Setting | Polyp Size | Procedure | Primary Endpoint | Confirmation of Complete Resection |
|---|---|---|---|---|---|---|---|---|
| CSP vs HSP (EMR) | ||||||||
| Suzuki [14] | 2018 | RCT, single center | Japan | General hospital | ≤10 mm | CSP vs HSP | Resection width achieved by polypectomy | Negative margin of resected specimen |
| Kawamura [13] | 2018 | RCT, multicenter | Japan | Multicenter | 4-9 mm | CSP vs HSP (EMR) | Complete resection rate | 2 biopsies |
| Papastergiou [25] | 2018 | RCT, dual center | Greece | Two tertiary referral centers | 6-10 mm | CS-EMR vs HS-EMR | Complete resection rate | 5 biopsies |
| Zhang [26] | 2018 | RCT, single center | China | A tertiary care referral center | 6-9 mm | CSP vs EMR | Incomplete resection rate | 5 biopsies |
| Horiuchi [15] | 2014 | RCT, single center | Japan | General hospital | ≤10 mm | CSP vs HSP | Delayed bleeding | Negative margin of the resected specimen |
| Paspatis [27] | 2011 | RCT, single center | Greece | General hospital | 3-8 mm | CSP vs HSP (EMR) | Delayed bleeding | / |
| Ichise [28] | 2011 | RCT, single center | Japan | General hospital | ≤8 mm | CSP vs HSP | Abdominal symptoms after polypectomy | Negative margin of the resected specimen |
| CSP vs CFP (JFP) | ||||||||
| Huh [29] | 2019 | RCT, dual center | Korea | Two tertiary referral centers | ≤5 mm | CSP vs JFP | Complete resection rate | 2 biopsies |
| Park [30] | 2016 | RCT, single center | Korea | Tertiary care referral hospital | ≤5 mm | CSP vs CFP | Complete resection rate | 2 biopsies |
| Kim [31] | 2015 | RCT, single center | Korea | University hospital | ≤7 mm | CSP vs CFP | Complete resection rate | EMR |
| Lee [32] | 2013 | RCT, single center | Korea | Academic hospital | ≤5 mm | CSP vs CFP | Complete resection rate | 2 biopsies |
| CSP vs HSP vs CFP | ||||||||
| Gomez [33] | 2015 | RCT, single center | United States | An academic hospital | <6 mm | CSP vs HSP vs CFP | Complete resection rate | Cold snaring or 4 biopsies |
| Prospective cohort study of cold polypectomy | ||||||||
| Shimodate [16] | 2017 | Prospective cohort, single center | Japan | General hospital | <10 mm | CSP and CFP | Complication | / |
| Schett [17] | 2017 | Prospective cohort, single center | Germany | General hospital | 4 to ≤15 mm | CSP only | Complication | / |
| Repici [4] | 2012 | Prospective cohort, multicenter | Italy | Five endoscopic centers | <10 mm | CSP and CFP | Complication | / |
CSP, cold snare polypectomy; HSP, hot snare polypectomy; EMR, endoscopic mucosal resection; CFP, cold forceps polypectomy; JFP, jumbo forceps polypectomy; RCT, randomized controlled trial; CS-EMR, cold snare endoscopic mucosal resection; HS-EMR, hot snare endoscopic mucosal resection
Table 2.
Snare and Forceps Used in Randomized Controlled Trials.
| First Author | Snare for CSP | Snare for HSP (EMR) | Forceps for CFP |
|---|---|---|---|
| Suzuki [14] | Captivator II 10-mm (Boston Scientific) | Captivator II 10-mm (Boston Scientific) | - |
| Kawamura [13] | Captivator II 10-mm (Boston Scientific) | Captivator II 10-mm (Boston Scientific) | - |
| Papastergiou [25] | Exacto 9-mm* (US Endoscopy) | Snare Master (Olympus), Acusnare (Cook Medical), Captivator II (Boston Scientific) | - |
| Zhang [26] | Snare Master 10-mm (Olympus) | Snare Master 10-mm (Olympus) | - |
| Horiuchi [15] | Dual-loop wire snare 33/16 mm (Medico’s Hirata) | Dual-loop wire snare 33/16 mm (Medico’s Hirata) | - |
| Paspatis [27] | Snare 13-mm (Boston Sensation Polypectomy Scientific) | Sensation Polypectomy Snare 13-mm (Boston Scientific) | - |
| Ichise [28] | SD-7P-1, BP-1 (Olympus) | Unknown | - |
| Huh [29] | SGO-1622S 10-mm (Endo-Therapeutics) | - | Radial Jaw 4 jumbo forceps* (Boston Scientific) |
| Park [30] | A micro-oval snare 10-mm (SD-210U-10; Olympus) | - | Oval spoon-shaped mouth forceps (MTW) |
| Kim [31] | A micro-oval snare 10-mm (SD-210U-10; Olympus) | - | Standard capacity forceps (FB-24U-1; Olympus) |
| Lee [32] | A micro-oval snare 10-mm (SD-210U-10; Olympus) | - | Standard capacity forceps (FB-24U-1; Olympus) |
| Gomez [33] | Captiflex Extra Small Oval 11-mm (Boston Scientific) | Captiflex Extra Small Oval 11-mm (Boston Scientific) | Radial Jaw 4 Large Capacity with a 2.8-mm needle (Boston Scientific) |
* Dedicated snare and jumbo forceps are described in bold.
CSP, cold snare polypectomy; HSP, hot snare polypectomy; EMR, endoscopic mucosal resection; CFP, cold forceps polypectomy
Incomplete resection rate
CSP vs. HSP for polyps ≤10 mm
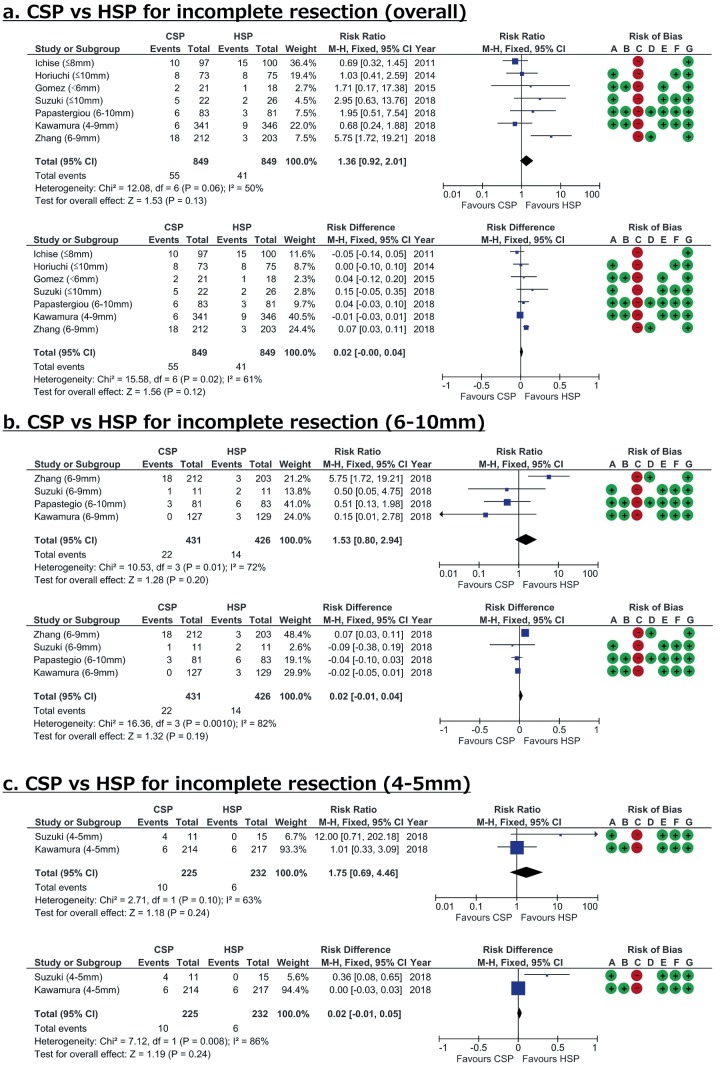
Among the 8 randomized controlled trials comparing CSP and HSP, the complete and incomplete resection rates were evaluated in 7 randomized controlled trials[13-15,25,26,28,33]. A “complete retrieval rate” was reported in the studies by Ichise et al.[28] and Horiuchi et al.[15], which, according to the corresponding author, meant that the negative rate of the histological margin was not indicated in those studies; furthermore, the corresponding author provided us with unpublished data of the negative histological margin rate. In each group, 849 polyps were evaluated for incomplete resection. The RR and RD of incomplete resection for CSP compared with HSP were 1.36 (95% CI, 0.92-2.01) and 0.02 (−0.00-0.04), respectively, which was not significantly different (Figure 2a). Heterogeneity between CSP and HSP studies was moderate (I2 = 50% in RR analysis).
Figure 2.
Forest plots of cold snare polypectomy (CSP) versus hot snare polypectomy (HSP) to determine incomplete resection rates according to polyp size. Risk of bias legend: A, random sequence generation (selection bias); B, allocation concealment (selection bias); C, blinding of participants and personnel (performance bias); D, blinding of outcome assessment (detection bias); E, incomplete outcome data (attrition bias); F, selective reporting (reporting bias); and G, other bias.
CSP vs. HSP for 6-10 mm and 4-5 mm polyps
The incomplete resection rate of 6-10 mm polyps was evaluated by 3 randomized controlled trials. There were 431 polyps in the CSP group and 426 polyps in the HSP group. According to the meta-analysis, there was no significant difference in the incomplete resection rate between the two groups (RR, 1.53; 95% CI, 0.80-2.94; RD, 0.02; 95% CI, −0.01-0.04); however, heterogeneity was large among the studies (I2 = 72% in RR analysis, Figure 2b). Only 2 randomized controlled trials evaluated the incomplete resection rate of 4-5 mm polyps. No significant difference was observed (RR, 1.75; 95% CI, 0.69-4.46; RD, 0.02; 95% CI, −0.01-0.05), and the heterogeneity was also large (I2 = 63% in RR analysis, Figure 2c).
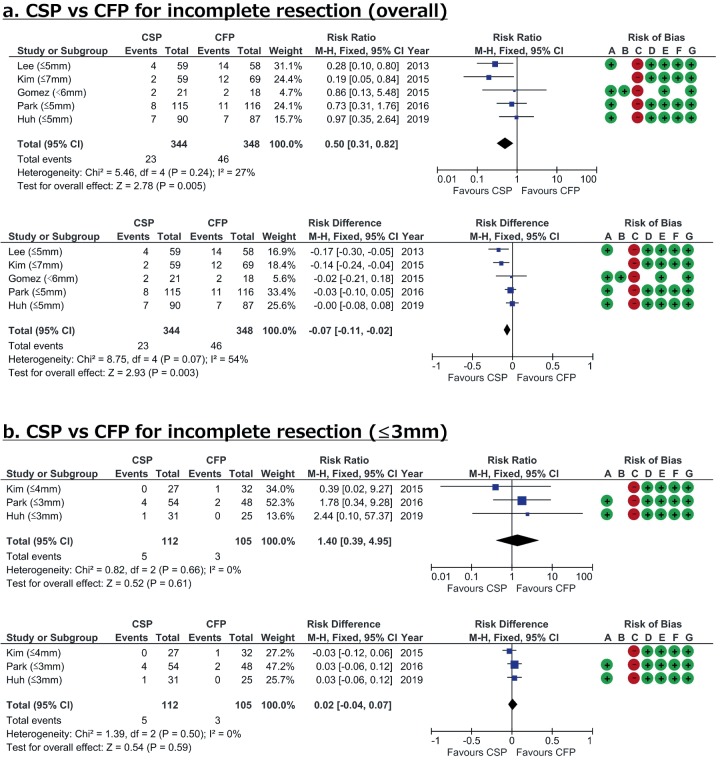
CSP vs. CFP for small polyps
The meta-analysis including all randomized controlled trials comparing CSP and CFP indicated that the incomplete resection rate was significantly higher for CFP than for CSP. The RR and RD for incomplete removal using CSP compared with CFP were 0.50 (95% CI, 0.31-0.82), and −0.07 (95% CI, −0.11 to −0.02), respectively, with relatively small heterogeneity among studies (I2 = 27% in RR analysis, Figure 3a). However, in the case of polyps ≤3 mm (≤4 mm in the study by Kim et al.[31]), there was little difference in the incomplete resection rate between groups, with no heterogeneity among studies (I2 = 0%, Figure 3b).
Figure 3.
Forest plots of cold snare polypectomy (CSP) versus cold forceps polypectomy (CFP) for incomplete resection rates according to polyp size. Risk of bias legend: A, random sequence generation (selection bias); B, allocation concealment (selection bias); C, blinding of participants and personnel (performance bias); D, blinding of outcome assessment (detection bias); E, incomplete outcome data (attrition bias); F, selective reporting (reporting bias); and G, other bias.
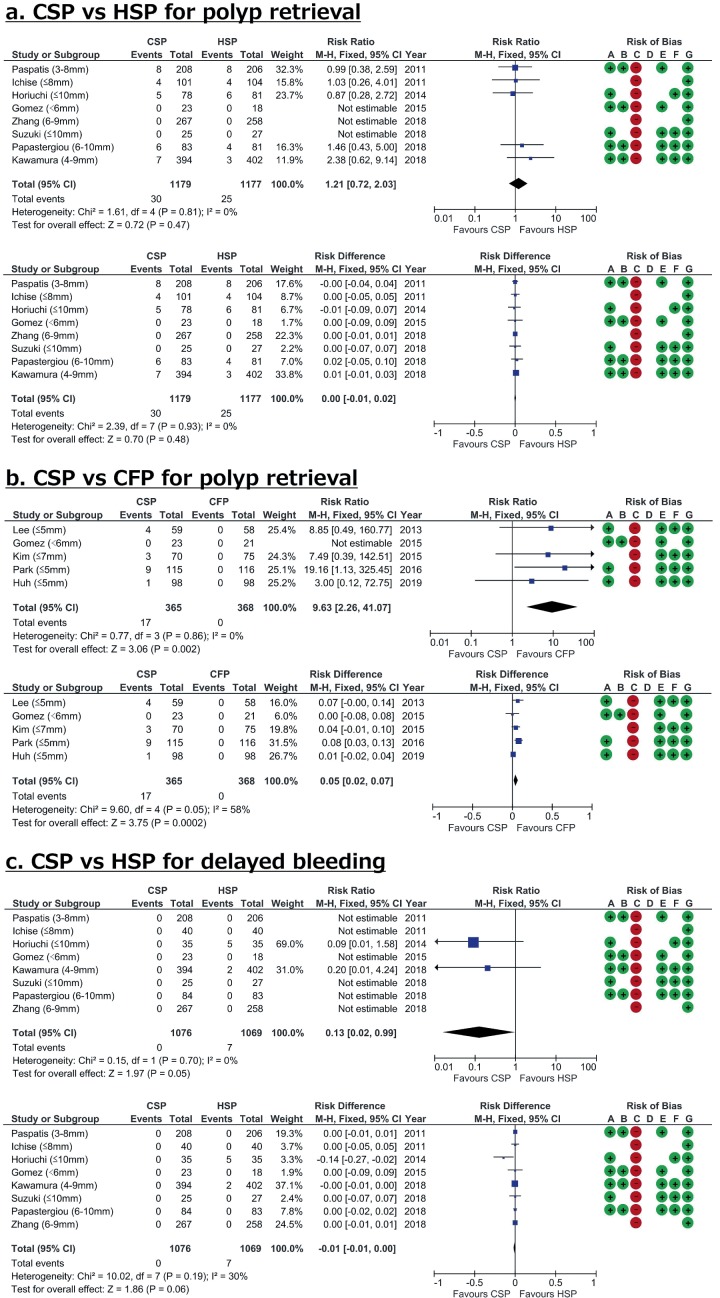
Polyp retrieval rate
There was no significant difference in the polyp retrieval rates of CSP and HSP, and there was no heterogeneity (I2 = 0%, Figure 4a). However, the retrieval rate for CFP was significantly higher than that for CSP, and no heterogeneity was observed among the studies (I2 = 0%). The RD for successful polyp retrieval using CFP compared with CSP was 0.05 (95% CI, 0.02-0.07, Figure 4b).
Figure 4.
Forest plots of the polyp retrieval rate and delayed bleeding rate. Risk of bias legend: A, random sequence generation (selection bias); B, allocation concealment (selection bias); C, blinding of participants and personnel (performance bias); D, blinding of outcome assessment (detection bias); E, incomplete outcome data (attrition bias); F, selective reporting (reporting bias); and G, other bias.
Delayed bleeding rate
For both CSP and HSP, the delayed bleeding rates were extremely low (Figure 4c). If the evaluation of delayed bleeding was insufficient when data from only randomized controlled trials were used, then we included prospective observational studies in the analysis. We found 3 observational studies and conducted a meta-analysis. The results indicated that 3446 polyps were removed by CP (2518 by CSP and 928 by CFP) and there was no delayed bleeding. The delayed bleeding rate after CP was expected to be <0.03%.
Certainty in cumulative evidence
Endoscopists were not blinded in all studies; therefore, there was a high risk of performance bias (Figure 2-4). The levels of the risk of bias for other domains were considered low or unclear. The overall risk of bias was considered serious for the GRADE system (Table 3, 4). Furthermore, the numbers of total events and sample sizes were small, even if all studies were integrated. Therefore, the imprecision domain was considered serious. Because two domains were evaluated as serious limitations in the GRADE system, the overall certainty of the evidence was evaluated as low for CSP compared with HSP and for CSP compared with CFP.
Table 3.
CSP Compared with HSP for Small Colorectal Polyps.
| Certainty assessment | Summary of findings | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of participants (studies) Follow-up | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Study event rates (%) | Relative effect (95% CI) | Anticipated absolute effects | ||
| With HSP | With CSP | Risk with HSP | Risk difference with CSP | ||||||||
| Incomplete resection rate | |||||||||||
| 1698 (7 RCTs) | serious a | not serious | not serious | serious b | none c | ⊕⊕◯◯ LOW | 41/849 (4.8%) | 55/849 (6.5%) | RR 1.36 (0.92 to 2.01) | Study population | |
| 5 per 100 | 2 more per 100 (from 0 fewer to 4 more) e | ||||||||||
| Low | |||||||||||
| 3 per 100 d |
1 more per 100 (from 0 fewer to 3 more) | ||||||||||
| High | |||||||||||
| 11 per 100 d |
4 more per 100 (from 1 fewer to 11 more) | ||||||||||
CI, confidence interval; RR, risk ratio
a. In all studies, the endoscopists were not blinded.
b. Few total events and small sample sizes.
c. Because there were fewer than 10 studies involved, funnel plots could not be created.
d. Regarding the incomplete resection rate, the control group risks in the 7 studies were 1.5%, 2.6%, 3.7%, 5.6%, 7.7%, 10.7%, and 15%. The second lowest from the bottom and the second highest from the top were taken as baseline estimates of “low risk” and “high risk,” respectively.
e. Calculated using Review Manager version 5.3.
Table 4.
CSP Compared with CFP for Diminutive Polyps.
| Certainty assessment | Summary of findings | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of participants (studies) Follow-up | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Overall certainty of evidence | Study event rates (%) | Relative effect (95% CI) | Anticipated absolute effects | ||
| With CFP | With CSP | Risk with CFP | Risk difference with CSP | ||||||||
| Incomplete resection rate | |||||||||||
| 692 (5 RCTs) | serious a | not serious | not serious | serious b | none c | ⊕⊕◯◯ LOW | 46/348 (13.2%) | 23/344 (6.7%) | RR 0.50 (0.31 to 0.82) | Study population | |
| 13 per 100 | 7 fewer per 100 (from 11 fewer to 2 fewer) e | ||||||||||
| Low | |||||||||||
| 10 per 100 d |
5 fewer per 100 (from 7 fewer to 2 fewer) | ||||||||||
| High | |||||||||||
| 17 per 100 d |
9 fewer per 100 (from 12 fewer to 3 fewer) | ||||||||||
CI, confidence interval; RR, risk ratio
a. In all studies, the endoscopists were not blinded.
b. Few total events and small sample sizes.
c. Because there were fewer than 10 studies involved, funnel plots could not be created.
d. Regarding the incomplete resection rate, the control group risks in the 5 studies were 8.0%, 9.5%, 11.1%, 17.4%, and 24.1%. The second lowest from the bottom and the second highest from the top were taken as baseline estimates of “low risk” and “high risk,” respectively.
e. Calculated using Review Manager version 5.
Discussion
We showed that the incomplete resection rate for polyps ≤10 mm using CSP was not significantly different compared with that using HSP in this meta-analysis. Furthermore, the incomplete resection rate of CFP was significantly higher than that of CSP. These results are comparable with those of a previous systematic review and meta-analysis[7-11]. However, we performed a subgroup analysis stratified by polyp size, which was not performed in previous reports. As a result, the difference between CFP and CSP was not significant for polyps ≤3 mm. These results support the clinical guidelines of the European Society of Gastrointestinal Endoscopy that suggest that CSP is recommended for small polyps and CFP may be used only for polyps 1-3 mm[35].
The incomplete resection rate of CSP tended to be higher than that of HSP; however, they were not significantly different. This seems to be because HSP is a procedure that uses electrocoagulation and is advantageous for complete eradication because of its burning effect. However, heterogeneity between CSP and HSP studies was moderate (I2 = 50% in RR analysis). Zhang et al.[26] reported that HSP is more favorable than CSP (RR, 5.75; 95% CI, 1.72-19.21) for complete resection; their randomized controlled trial was large (n = 415), however, it seemed to have a high risk of bias. We also reported a large-scale randomized controlled trial (n = 687) in which the results showed no statistical significance regarding the complete resection rates for CSP and HSP[13]. However, there were inconsistencies between the results of the two large-scale randomized controlled trials[13,26]. Other small studies[14,15,25,28,33] have shown no statistical significance and the risk of bias was high. Therefore, the statistical differences may change if further studies with a low risk of bias are performed.
Dedicated snares for CSP were not used in many studies, and it is possible that the CSP procedure itself was highly variable among studies. It has been reported that the use of a dedicated snare may contribute to improved incomplete resection rates[36]; therefore, the type of snare used in the studies may affect the results.
The size of polyps in studies comparing CSP and CFP was smaller than in those comparing CSP and HSP. In the present meta-analysis, CSP had significantly lower incomplete resection rates compared with CFP, and there was less heterogeneity between studies. However, the polyp retrieval rate was significantly higher for CFP. If polyp retrieval is the primary outcome, then CFP may be the better procedure. However, if a “resect and discard strategy” that does not require polyp retrieval or histopathological examinations[37] is adopted, then CSP might be the better choice because of the lower incomplete resection rate.
There was no significant difference between CSP and CFP for polyps ≤3 mm, and there was less heterogeneity between studies. Because of the aforementioned advantages of polyp retrieval with CFP, it is advantageous for polyps ≤3 mm. In this meta-analysis, there were studies of CFP that involved jumbo forceps and those that involved normal biopsy forceps. However, a randomized controlled trial showed the superior performance of jumbo biopsy forceps compared with standard biopsy forceps for the eradication of small polyps[38]. Furthermore, the most recent randomized controlled trial[29] that compared CSP with CFP using jumbo biopsy forceps showed comparative incomplete resection rates for both procedures when polyps were ≤5 mm; therefore, jumbo forceps might contribute to better removal rates for polyps ≤5 mm.
As indicated in this systematic review, the delayed bleeding rate of CSP is extremely low. It has also been reported that the delayed bleeding rate of CSP was significantly lower than that of HSP for anticoagulated patients[15]. If the difference in incomplete resection rates for these methods is not large, then the safer procedure should be chosen. Therefore, we recommend CSP rather than HSP for the treatment of polyps ≤10 mm because of its lower delayed bleeding rate.
In the present study, the analysis focused only on the polyp size. However, it should be avoided to decide the indication of CSP only by the size of the polyp. Lesions with advanced histology are present even if the polyp is <10 mm, and it is important to carefully diagnose endoscopically before resection. CSP could be disadvantageous compared with HSP to obtain submucosal tissue[14,39]. In order to avoid performing CSP for small invasive cancer, endoscopic diagnosis before resection is important.
This study had several limitations. First, CP has only been actively researched in recent years; therefore, there were insufficient studies on CP to create funnel plots to evaluate publication bias. Furthermore, non-English language papers were not evaluated. Second, it is challenging to endoscopically measure the exact polyp size. Usually, we compare polyps using the snare or forceps when we estimate the polyp size; however, this estimation may vary among endoscopists. Third, there could be a difference in the cost-effectiveness of CP and other procedures, but we could not evaluate it. Finally, methods of measuring incomplete resection rates, as a primary endpoint of this study, varied among studies.
Despite these limitations, we believe this meta-analysis showed the usefulness of CP for polyps ≤10 mm. From the viewpoint of resection ability, CSP had non-inferior performance compared to HSP for polyps ≤10 mm. Because of its safety profile, CSP should be recommended for polyps ≤10 mm. When polyp retrieval is the main outcome, CFP may be considered for polyps ≤3 mm.
Conflicts of Interest
Takuji Kawamura received a research grant from Boston Scientific for the previous study. This meta-analysis was self-funded.
Author Contributions
TK: study concept and design, acquisition of data, analysis and interpretation of data, and drafting of the manuscript. YT: acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content. NT: critical revision of the manuscript for important intellectual content, study supervision. IY: statistical review. All authors approved the final version of this manuscript.
Approval by Institutional Review Board (IRB)
N/A
Acknowledgements
We thank Dr. Akira Horiuchi (Showa Inan General Hospital), Prof. Takuji Gotoda (Nihon University School of Medicine), Dr. Sho Suzuki (Nihon University School of Medicine), and Dr. Yuichi Shimodate (Kurashiki Central Hospital) for providing unpublished data of their work. We also thank Dr. Yutaka Saito (National Cancer Center Hospital) and other members of the Japanese screening and surveillance colonoscopy guideline committee for providing us the opportunity to perform this systematic review. Furthermore, we thank Editage (www.editage.jp) for English language editing.
References
- 1.Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012 Feb; 366(8): 687-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brenner H, Chang-Claude J, Seiler CM, et al. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011 Jan; 154(1): 22-30. [DOI] [PubMed] [Google Scholar]
- 3.Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013 Sep; 369(12): 1095-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Repici A, Hassan C, Vitetta E, et al. Safety of cold polypectomy for <10mm polyps at colonoscopy: a prospective multicenter study. Endoscopy. 2012 Jan; 44(1): 27-31. [DOI] [PubMed] [Google Scholar]
- 5.Singh N, Harrison M, Rex DK. A survey of colonoscopic polypectomy practices among clinical gastroenterologists. Gastrointest Endosc. 2004 Sep; 60(3): 414-8. [DOI] [PubMed] [Google Scholar]
- 6.Tappero G, Gaia E, De Giuli P, et al. Cold snare excision of small colorectal polyps. Gastrointest Endosc. 1992 May-Jun; 38(3): 310-3. [DOI] [PubMed] [Google Scholar]
- 7.Shinozaki S, Kobayashi Y, Hayashi Y, et al. Efficacy and safety of cold versus hot snare polypectomy for resecting small colorectal polyps: Systematic review and meta-analysis. Dig Endosc. 2018 Sep; 30(5): 592-9. [DOI] [PubMed] [Google Scholar]
- 8.Qu J, Jian H, Li L, et al. Effectiveness and safety of cold versus hot snare polypectomy: A meta-analysis. J Gastroenterol Hepatol. 2019 Jan; 34(1): 49-58. [DOI] [PubMed] [Google Scholar]
- 9.Fujiya M, Sato H, Ueno N, et al. Efficacy and adverse events of cold vs hot polypectomy: A meta-analysis. World J Gastroenterol. 2016 Jun; 22(23): 5436-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jung YS, Park CH, Nam E, et al. Comparative efficacy of cold polypectomy techniques for diminutive colorectal polyps: a systematic review and network meta-analysis. Surg Endosc. 2018 Mar; 32(3): 1149-59. [DOI] [PubMed] [Google Scholar]
- 11.Raad D, Tripathi P, Cooper G, et al. Role of the cold biopsy technique in diminutive and small colonic polyp removal: a systematic review and meta-analysis. Gastrointest Endosc. 2016 Mar; 83(3): 508-15. [DOI] [PubMed] [Google Scholar]
- 12.https://www.crd.york.ac.uk/PROSPERO.
- 13.Kawamura T, Takeuchi Y, Asai S, et al. A comparison of the resection rate for cold and hot snare polypectomy for 4-9 mm colorectal polyps: a multicentre randomised controlled trial (CRESCENT study). Gut. 2018 Nov; 67(11): 1950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suzuki S, Gotoda T, Kusano C, et al. Width and depth of resection for small colorectal polyps: hot versus cold snare polypectomy. Gastrointest Endosc. 2018 Apr; 87(4): 1095-103. [DOI] [PubMed] [Google Scholar]
- 15.Horiuchi A, Nakayama Y, Kajiyama M, et al. Removal of small colorectal polyps in anticoagulated patients: a prospective randomized comparison of cold snare and conventional polypectomy. Gastrointest Endosc. 2014 Mar; 79(3): 417-23. [DOI] [PubMed] [Google Scholar]
- 16.Shimodate Y, Mizuno M, Takezawa R, et al. Safety of cold polypectomy for small colorectal neoplastic lesions: a prospective cohort study in Japan. Int J Colorectal Dis. 2017 Sep; 32(9): 1261-6. [DOI] [PubMed] [Google Scholar]
- 17.Schett B, Wallner J, Weingart V, et al. Efficacy and safety of cold snare resection in preventive screening colonoscopy. Endoscopy Int Open. 2017 Jul; 5(7): E580-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011 Oct; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011 Apr; 64(4): 383-94. [DOI] [PubMed] [Google Scholar]
- 20.Arimoto J, Chiba H, Ashikari K, et al. Safety of Cold Snare Polypectomy in Patients Receiving Treatment with Antithrombotic Agents. Dig Dis Sci. 2019 Nov; 64(11): 3247-55. [DOI] [PubMed] [Google Scholar]
- 21.Din S, Ball AJ, Taylor E, et al. Polypectomy practices of sub-centimeter polyps in the English Bowel Cancer Screening Programme. Surg Endosc. 2015 Nov; 29(11): 3224-30. [DOI] [PubMed] [Google Scholar]
- 22.Komeda Y, Kashida H, Sakurai T, et al. Removal of diminutive colorectal polyps: A prospective randomized clinical trial between cold snare polypectomy and hot forceps biopsy. World J Gastroenterol. 2017 Jan; 23(2): 328-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Din S, Ball AJ, Riley SA, et al. A randomized comparison of cold snare polypectomy versus a suction pseudopolyp technique. Endoscopy. 2015 Nov; 47(11): 1005-10. [DOI] [PubMed] [Google Scholar]
- 24.Aslan F, Camci M, Alper E, et al. Cold snare polypectomy versus hot snare polypectomy in endoscopic treatment of small polyps. Turk J Gastroenterol. 2014 Jun; 25(3): 279-83. [DOI] [PubMed] [Google Scholar]
- 25.Papastergiou V, Paraskeva KD, Fragaki M, et al. Cold versus hot endoscopic mucosal resection for nonpedunculated colorectal polyps sized 6-10 mm: a randomized trial. Endoscopy. 2018 Apr; 50(4): 403-11. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Q, Gao P, Han B, et al. Polypectomy for complete endoscopic resection of small colorectal polyps. Gastrointest Endosc. 2018 Mar; 87(3): 733-40. [DOI] [PubMed] [Google Scholar]
- 27.Paspatis GA, Tribonias G, Konstantinidis K, et al. A prospective randomized comparison of cold vs hot snare polypectomy in the occurrence of postpolypectomy bleeding in small colonic polyps. Colorectal Dis. 2011 Oct; 13(10): e345-8. [DOI] [PubMed] [Google Scholar]
- 28.Ichise Y, Horiuchi A, Nakayama Y, et al. Prospective randomized comparison of cold snare polypectomy and conventional polypectomy for small colorectal polyps. Digestion. 2011; 84(1): 78-81. [DOI] [PubMed] [Google Scholar]
- 29.Huh CW, Kim JS, Choi HH, et al. Jumbo biopsy forceps versus cold snares for removing diminutive colorectal polyps: A prospective randomized controlled trial. Gastrointest Endosc. 2019 Jul; 90(1): 105-11. [DOI] [PubMed] [Google Scholar]
- 30.Park SK, Ko BM, Han JP, et al. A prospective randomized comparative study of cold forceps polypectomy by using narrow-band imaging endoscopy versus cold snare polypectomy in patients with diminutive colorectal polyps. Gastrointest Endosc. 2016 Mar; 83(3): 527-32. [DOI] [PubMed] [Google Scholar]
- 31.Kim JS, Lee BI, Choi H, et al. Cold snare polypectomy versus cold forceps polypectomy for diminutive and small colorectal polyps: a randomized controlled trial. Gastrointest Endosc. 2015 Mar; 81(3): 741-7. [DOI] [PubMed] [Google Scholar]
- 32.Lee CK, Shim JJ, Jang JY. Cold snare polypectomy vs. Cold forceps polypectomy using double-biopsy technique for removal of diminutive colorectal polyps: a prospective randomized study. Am J Gastroenterol. 2013 Oct; 108(10): 1593-600. [DOI] [PubMed] [Google Scholar]
- 33.Gomez V, Badillo RJ, Crook JE, et al. Diminutive colorectal polyp resection comparing hot and cold snare and cold biopsy forceps polypectomy. Results of a pilot randomized, single-center study (with videos). Endoscopy Int Open. 2015 Feb; 3(1): E76-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. https://handbook-5-1.cochrane.org/ (Higgins JP, Green S, editors.). https://handbook-5-1.cochrane.org/.
- 35.Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017 Mar; 49(3): 270-97. [DOI] [PubMed] [Google Scholar]
- 36.Horiuchi A, Hosoi K, Kajiyama M, et al. Prospective, randomized comparison of 2 methods of cold snare polypectomy for small colorectal polyps. Gastrointest Endosc. 2015 Oct; 82(4): 686-92. [DOI] [PubMed] [Google Scholar]
- 37.Ignjatovic A, East JE, Suzuki N, et al. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): a prospective cohort study. Lancet Oncol. 2009 Dec; 10(12): 1171-8. [DOI] [PubMed] [Google Scholar]
- 38.Draganov PV, Chang MN, Alkhasawneh A, et al. Randomized, controlled trial of standard, large-capacity versus jumbo biopsy forceps for polypectomy of small, sessile, colorectal polyps. Gastrointest Endosc. 2012 Jan; 75(1): 118-26. [DOI] [PubMed] [Google Scholar]
- 39.Shichijo S, Takeuchi Y, Kitamura M, et al. Does cold snare polypectomy completely resect the mucosal layer? A prospective single-center observational trial. J Gastroenterol Hepatol. 2020 Feb; 35(2): 241-8. [DOI] [PubMed] [Google Scholar]