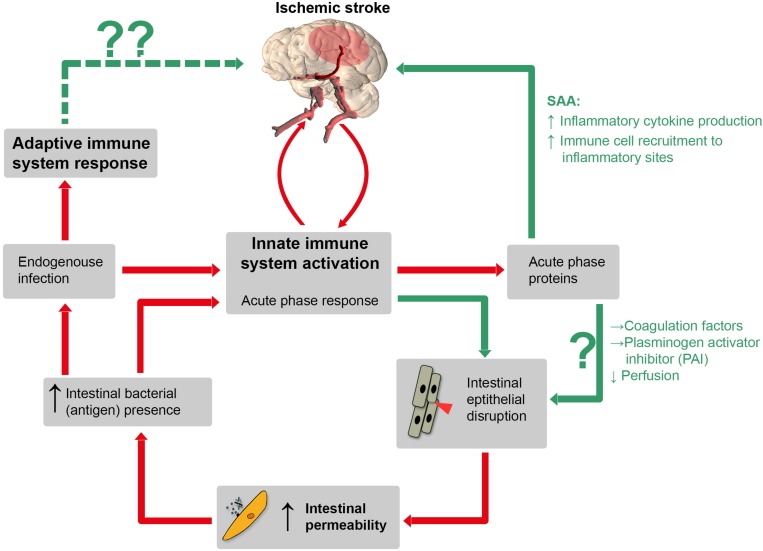
FIGURE 1.
Schematic illustration of a hypothetical pathophysiological cascade following ischemic stroke (IS): the innate immune system is activated by cerebral ischemia due to release of inflammatory cytokines after blood-barrier-breakdown. Hence, these cytokines could directly inflict “off-site” damage to the intestinal mucosa and induce the production of APPs such as serum amyloid A (SAA), coagulation factor and plasminogen activator inhibitor (PAI). SAA itself stimulates further inflammatory cytokine production via positive feedback stimulation. Other APPs, such as coagulation factors and PAI can impair capillary perfusion and, importantly, increase IP which is associated with bacterial translocation. Consequently, both pathways increase the amount of pro-inflammatory mediators, which leads to a prolonged inflammatory stage following IS. Red lines: established mechanisms, green lines: potential mechanisms (according to our hypothesis). Whether or not adaptive immune processes, augmented by the translocation of bacteria and bacterial antigens from the gut, can inflict secondary brain damage is entirely speculative (dotted green line, upper left).