Figure 25:
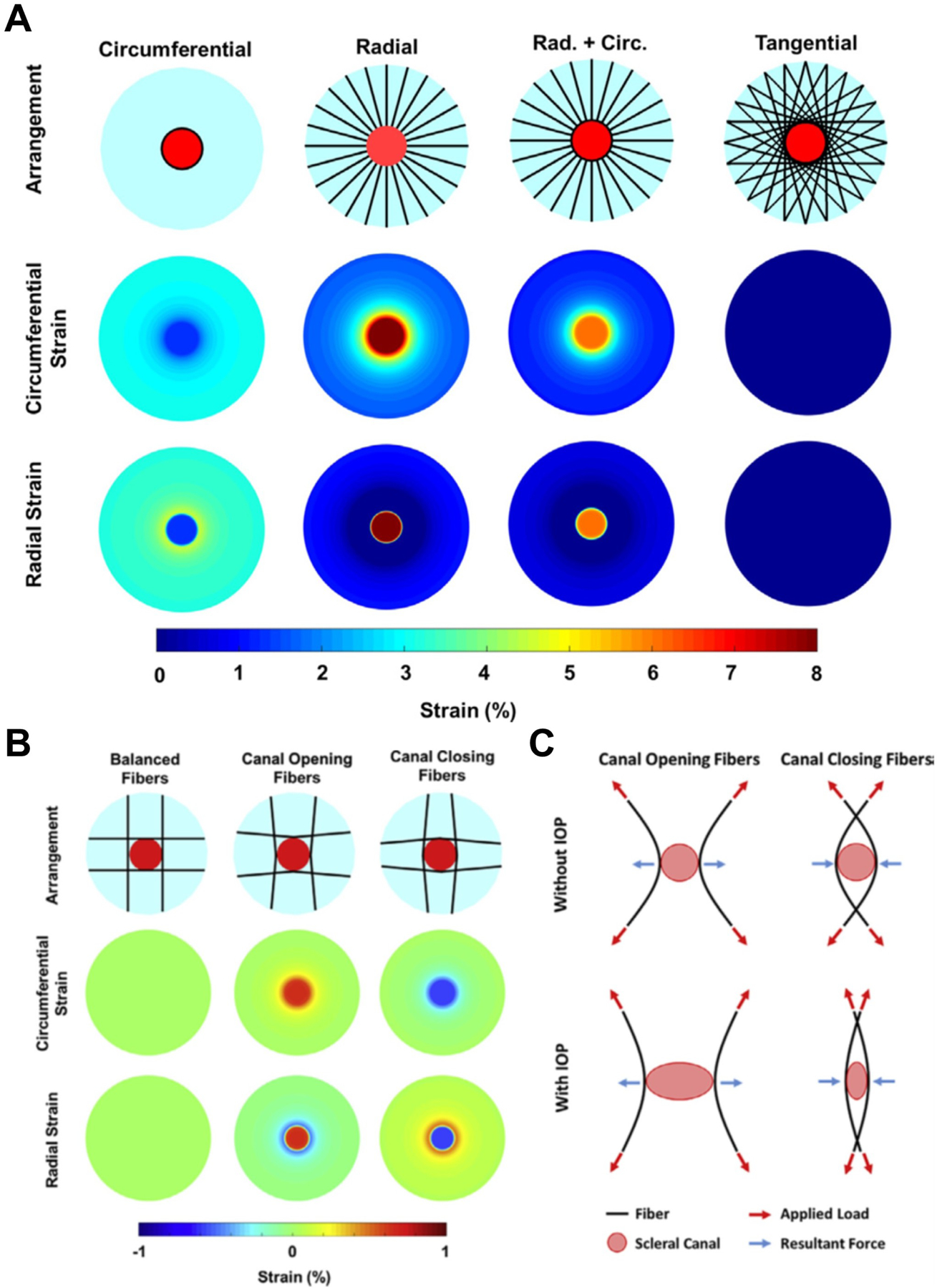
A) Computational models used to simulate the biomechanical behavior of four theoretical collagen fibre arrangements (top row). Shown in light blue is the posterior sclera, with the scleral canal as a red disc. The black lines represent the collagen fibres. On the middle and bottom row are shown contour levels of the magnitude of the deformations (strain) due to an IOP elevation of 50 mmHg. A simple reinforcement of the canal with circumferential fibres limited the strain in the lamina due to IOP but did provide support to the sclera. Conversely, a radial arrangement of fibres reduced the strain in the sclera, but lead to high strains within the lamina. The combination of radial and circumferential fibres still caused high strains in the lamina. A tangential arrangement of fibres provided the best reinforcement for both the sclera and the lamina, reducing the strains to near zero-levels. Depending on the fibre curvature, long fibres tangential to the canal can have substantially different responses to IOP increases. B) Maps of IOP-induced strain for three different fibre curvatures. When the fibres were concave to the canal (Canal Closing Fibers), increased IOP caused the canal to close, and lamina compression. When the fibres were convex (Canal Opening Fibers), increased IOP caused the canal to open and the lamina to stretch. Note that the models incorporated many fibres. For simplicity, only a few are shown. C) Diagram of the mechanism of action of long tangential fibres. For concave fibres, the load from IOP results in an outward tensile force at the canal boundary as the fibres straighten. For convex fibres, the load from IOP results in an inward compressive force at the canal boundary as the fibres straighten. Figure adapted from (Voorhees et al., 2018) with permission of Acta Biomaterialia.
