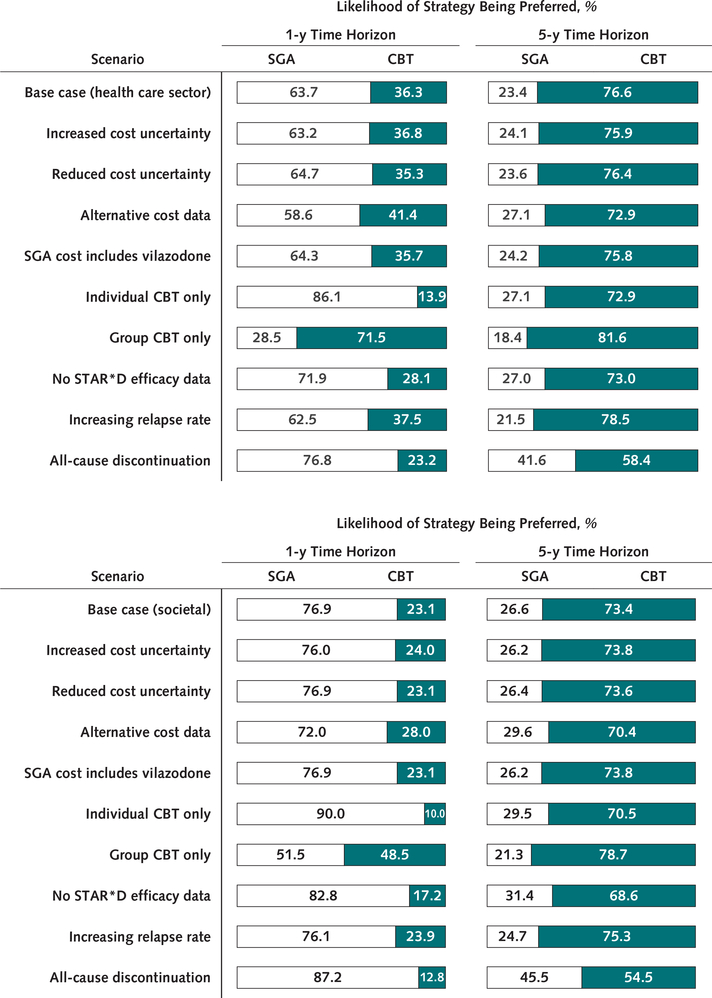
Figure 2. Scenario sensitivity analyses.
Bars show the percentage of 10 000 probabilistic model runs in which either SGA or CBT is the preferred treatment strategy (i.e., that which produces the greatest net monetary benefit), at a willingness-to-pay threshold of $100 000 per quality-adjusted life-year. Results are shown for both 1- and 5-year time horizons. The vertical axis shows the scenario being modeled, indicating a change in either parameter values or model structure relative to the base case. CBT = cognitive behavioral therapy; SGA = second-generation antidepressant; STAR*D = Sequenced Treatment Alternatives to Relieve Depression. Top. Results from a health care sector perspective. Bottom. Results from a societal perspective. Scenarios include increased or reduced cost uncertainty (SEs of first-line SGA and CBT cost estimates are increased or reduced to 30% or 10% of the mean); alternative cost data (annual background depression costs of $12 389 for remission and $17 551 for nonremission); SGA cost includes vilazodone (vilazodone is incorporated into SGA costing analysis, increasing annual cost of SGA from $48 to $72); individual or group CBT only (exclusively individual sessions or exclusively group sessions are used to calculate CBT costs); no STAR*D efficacy data (odds of remission and response are reduced by 19% with each successive treatment rather than using STAR*D data on remission and response rates); increasing relapse rate (by a relative 15% with each successive treatment); all-cause discontinuation (all-cause discontinuation [rather than discontinuation due to adverse events] is simulated; annual probability is 46.0% for SGA, with a relative risk of 1.00 [95% CI, 0.55 to 1.81] for CBT vs. SGA).