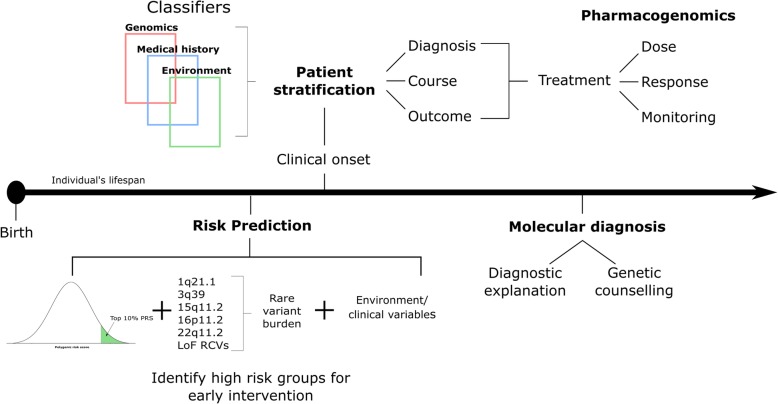
Fig. 2.
Illustration of what precision psychiatry might look like. With the increasing use of high-throughput genomic technologies in clinical genetics (e.g., the 100 K Genomes Project), it is likely that genomics will eventually have a role in psychiatric healthcare. Quantitative measures of the genetic liability to psychiatric disorders, such as polygenic risk scores, could be combined with additional clinical variables and psycho-social risk factors to help tailor treatment to the individual at several junctures across the lifespan. We briefly highlight here four key areas (risk prediction, patient stratification, pharmacogenomic and molecular diagnostics) where precision psychiatry would directly benefit the management and treatment of patients and provide a general timeline for when they could impact healthcare across an individual’s lifespan (Fig. 2). Risk prediction: Genetic risk scores could help target early intervention strategies towards those at greatest risk for developing a major psychiatric disorder. For example, schizophrenia genomic risk scores could be used to help predict which individuals from phenotypically defined high-risk groups are more likely to develop psychosis. Moreover, individuals who carry a pathogenic copy number variant could receive additional monitoring and/or screening for psychiatric and/or physical comorbidities. Patient stratification: Psychiatric disorders are associated with marked clinical variability in disease course and outcome, both within and across diagnostic categories. Research into biological and environmental exposures associated with this variability will inform stratification of patients into those that could benefit from tailored programs of treatment. Pharmacogenomics: Pharmacogenomic variants are known to influence variation in drug response. Precision psychiatry could therefore impact the way drugs are prescribed, by identifying patients most likely to benefit, predicting the dose required to maximize their therapeutic effects, and identifying patients who require additional monitoring for adverse side effects. Molecular diagnosis: No individual genetic variant is either necessary or sufficient to cause psychiatric disorders; however, the identification of rare, highly penetrant risk mutations, such as 22q11.2 deletions, can help towards providing a diagnostic explanation for the development of a psychiatric disorder. As our knowledge about the penetrance and phenotypic variability associated with rare risk variants improves, their identification among psychiatric patients will inform both genetic counseling and the examination of comorbidities