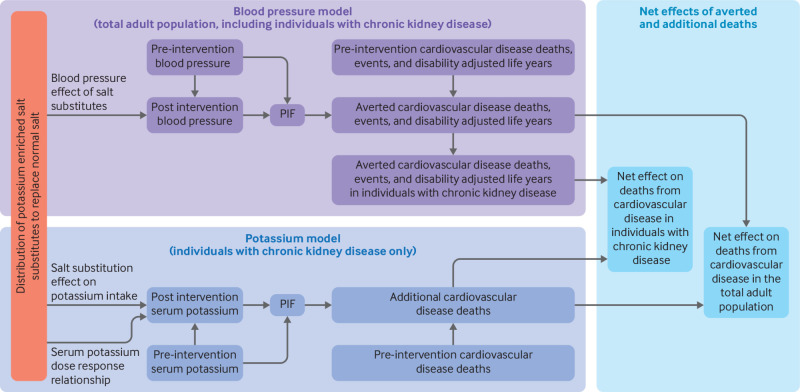
Fig 1.
Conceptual models used to estimate benefits, harms, and net effects of replacing dietary salt (sodium chloride) with potassium enriched salt substitutes. Distribution of potassium enriched salt substitutes to replace dietary salt was expected to reduce blood pressure in the adult population, with greater effects at older ages. In 24 age-sex groups, blood pressure distribution before the intervention and the lower blood pressure distribution after the intervention (that is, after replacement) were used to calculate a potential impact fraction (PIF), with risk estimates for blood pressure on outcomes of cardiovascular disease, for each of 11 subtypes of cardiovascular disease. The age, sex, and subtype specific PIF was multiplied by the pre-intervention estimates of the same groups for deaths from cardiovascular disease, non-fatal events, or disability adjusted life years to estimate the number of averted deaths, non-fatal events, or disability adjusted life years. In each age-sex group, the total number of averted deaths from cardiovascular disease, prevalence of chronic kidney disease, and the death risk from cardiovascular disease in patients with chronic kidney disease (compared with others) were used to estimate the number of averted deaths from cardiovascular disease attributed to individuals with chronic kidney disease. For each chronic kidney disease stage (G3a, G3b, G4, and G5), estimates of the expected increase in potassium intake from replacement of dietary salt with potassium enriched salt substitutes, the dose-response relation of dietary and serum potassium, and pre-intervention serum potassium distribution were used to estimate the post-intervention serum potassium distribution. The serum potassium distributions (before and after the intervention) and known risk estimates of serum potassium with deaths from cardiovascular disease were used to calculate a PIF for each chronic kidney disease stage. The PIF and stage specific estimate of pre-intervention deaths from cardiovascular disease were used to calculate the additional deaths from cardiovascular disease. The additional deaths were subtracted from averted deaths to estimate net benefits (averted deaths) in individuals with chronic kidney disease exclusively and in the total adult population, including those with chronic kidney disease. Table 1 presents the model inputs and the appendix provides detailed information and rationales on model calculations and assumptions