Abstract
The COVID-19 outbreak has drawn heightened attention from public health scholars researching ways to limit its spread. Much of the research has been focused on minimizing transmission in hospitals and in the general community. However, a particularly vulnerable community that has received relatively little attention is elders residing in long-term care facilities (LTCFs). In this article we address this relative lack of attention, arguing that enhanced traffic control bundling (eTCB) can and should be adopted and implemented as a means of protecting LTCF residents and staff. Enhanced TCB has been widely applied in hospital settings and has proven effective at limiting droplet and fomite transmissions both within hospitals and between hospitals and the general community. By effectively adapting eTCB to LTCF conditions, particularly by incorporating compartmentalization within zones plus active surveillance, COVID-19 transmission into and throughout LTCFs can be minimized, thereby saving numerous lives among an especially vulnerable population.
Keywords: Long-term care facility, Enhanced traffic control bundling, Compartmentalization, COVID-19, Pandemic, Mitigation
Introduction
Coronavirus disease 2019 (COVID-19) erupted in Wuhan China in late December 2019. On January 30, 2020, the WHO declared COVID-19 a Public Health Emergency of International Concern. On March 11, 2020, the WHO affirmed the rapid spreading of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) leading to a pandemic.1 COVID-19 is highly transmissible and yet of lower pathogenicity than SARS-CoV 2003. Based on current data, we estimate that over 80% of identified cases are self-limited mild illness. Severe cases occur largely among those aged over 60, while case-fatality rates are highest among elderly people suffering from co-morbidities.2
In general, the elderly suffer from weakened immunity and underlying diseases. When the aged population living together in semi-confined spaces such as long term care facilities (LTCFs) they are among the populations most vulnerable to infection and rapid spread.3 , 4 As a result, there is at a high risk of widespread transmission within LTCFs with the potential for high case-fatality rates and then spread back into the community thereby contributing to overall disease spread.5 , 6 It is therefore essential that the health care community develop infection control guidelines on prevention measures to address pandemic preparedness and response in LTCFs.7 , 8
Here we offer recommendations based on what we consider the “gold standard” for pandemic preparedness and response in LTCFs. However, we recognize that the ideal response we describe is likely not an option for LTCFs in the midst of the current COVID-19 pandemic. Therefore, we urge LTCF officials to view these recommendations as both guidance to address the current situation as well as long-term recommendations they should consider in preparation for future epidemics.
Infection risk in LTCFs
LTCFs serve as residences for the elderly (often with various co-morbidities) who can no longer live independently in the broader community. In LTCFs, the elderly live in close proximity while under the care of often inadequately trained and under-resourced nurse assistants.3 Unsurprisingly, LTCFs are often a locus of infection. And, due to high transmissibility rates via droplet and contact transmission, respiratory viral infections are among the infections most frequently plaguing LTCFs.4 , 9, 10, 11 These infections arrive in LTCFs from hospitals and the general community. The infections are brought in by people entering the facilities, including employees, family members and other visitors, workers and new residents. It is to be expected that SARS-CoV-2 will enter LTCFs in this manner, initiating an outbreak within the facility.
Complicating conditions, COVID-19 has both a long incubation period and an extended period of viral shedding. In addition, while many ill patients have either trivial symptoms or remain asymptomatic throughout their illness, are all capable of transmitting the virus to others.12 These people are difficult to identify but they may unwittingly spread the infection through droplet and fomite transmission while in the LTCF. Invariably, these unwitting transmissions will result in infection clusters that may erupt in a surge affecting the entire institution.6
Infection control guidelines for LTCFs
Designate a chief officer responsible for epidemic preparedness and response
LTCF leadership should designate a staff member to lead epidemic preparation and response in the LTCF. The designated person should be trained in the basics of infection control, including surveillance and reporting such as web-reporting through the syndromic surveillance system; hand hygiene, cleaning and environmental disinfection, and maintaining essential stockpiles.7 , 8
Maintaining surveillance and reporting for healthcare workers/caregivers and residents
In addition to routine chest x-rays at regular interval, all people at the LTCF should be vaccinated against influenza and pneumonia. During an outbreak staff and residents should receive and know how to engage in timely reporting after the appearance of any COVID-19 related symptoms/signs and /or discomfort. In addition, a regular health log should be maintained for both staff and residents noting in particular any potential exposure. Healthcare workers (HCWs) should be discouraged from engaging in work in more than one LTCF in order to avoid the possibility of inter-facility infection.13
Ensuring education and training
Staff and residents should be informed about COVID-19 and major infection control procedures including hand disinfection and fomite control. Special attention must be given to training part time workers or inadequately trained nurse assistants.8 , 14
Allocating epidemic/pandemic prevention equipment
LTCFs must ensure that they are adequately supplied with personal protective equipment (PPE) including masks, gloves and alcohol-based disinfectant. Plans must be in place to ensure equipment is effectively utilized and replaced as needed during a pandemic.15
Engage in environmental cleaning and disinfection
As fomite transmission may play a major role in SARS-CoV-2 transmission, environmental disinfection must be highlighted as a routine daily practice according to general infection control guidelines. Disinfection is essential for all frequently touched surfaces such as door handles, bed rails, tables, light switches, bathrooms, etc.. In all locations, disinfection requires a two-step process including preliminary cleaning with a regular detergent followed by disinfection with hospital-grade disinfectant or a diluted concentration of bleach.7
Enhanced traffic control bundling in LTCF to minimize COVID-19 risk
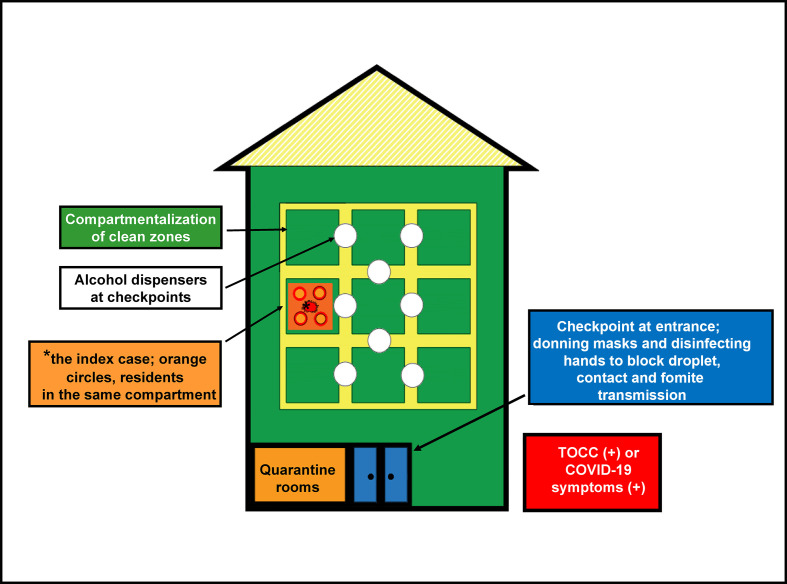
Based on lessons learned from SARS 2003, Taiwan developed the enhanced traffic control bundling (eTCB) model to contain the SARS-CoV-2's spread.14 , 16 Enhanced TCB evolved from TCB (Traffic Control Bundling) which focuses on protecting HCWs and patients in hospitals.17 TCB is based on ‘Six Sigma which describes ‘streamlined quality control’ that achieve error-free outcomes 99.99966 percent of the time.18 Given the significant vulnerability of LTCF residents and staff to the COVID-19 pandemic, here we recommend adopting eTCB, and adapting it to LTCFs. Enhanced TCB protects LTCF staff and residents from droplet, contact and fomite transmission through a process including triage prior to entering the facility, separate zones of risk within the facility and checkpoint hand hygiene throughout.17 (Fig. 1 ) Successful eTCB implementation will minimize the danger of cluster infections and ultimately, the risk of a facility lockdown.
Figure 1.
Compartmentalization in long-term care facilities (LTCFs). The goal of compartmentalization in LTCFs is to supplement enhanced traffic control bundling as a further means of limiting COVID-19 (or other infectious disease) transmission. According to this approach, LTCFs establish distinct compartments within clean zones. Each compartment is staffed by healthcare workers and support staff who are specifically designated to that compartment. Compartments are, ideally, in separate buildings. However, since this is rarely an option, separate floors in the same building or even clearly differentiated zones on the same floor are options. Movement among compartments should be minimized, but when necessary must involve proper hand hygiene at designated hand disinfection checkpoints established between each compartment. TOCC, travel, occupation, contact, and cluster.
Triage prior to entering the facility
During outbreaks of COVID-19, the threat originates outside the LTCF.6 To protect residents and staff, entry to the facility should be limited to essential personnel only. These essential personnel include, HCWs, nurse assistants, new resident and support personnel responsible for laundry, kitchen and daily tasks such as cleaning and waste disposal. All entrants must be assessed based on history of TOCC (travel, occupation, contact, cluster-detailed below). TOCC is potentially the most valuable surveillance and risk assessment tool available at the initial stage and site in both the containment and mitigation phases of the COVID-19 response.19 TOCC involves taking a travel history for each person entering the facility as well as assessing their occupational history regarding potential encounters with foreign travelers. Contact history must also be taken to identify those who may have visited a hospital or emergency room in the previous two weeks. Finally, in the phase of community circulation, a history of encounters with potential clusters should be identified. Importantly, symptoms of COVID-19 including fever, cough, general malaise, influenza-like illness or diarrhea, loss of taste, and skin rashes are contraindicated and as such, people exhibiting such symptoms should be forbidden entry to the facility. When found to be symptom-free and thus permitted entry to the facility, all entrants shall wear surgical face masks and disinfect their hands to protect residents and the facility from any potential COVID-19 outbreaks arising from droplet, contact and/or fomite transmission by asymptomatic individuals.14 , 17
Separate zones of risks
In addition to the checkpoint controls at the LTCF entrance, there should be transition and clean zones inside the facility.
The transition zone is the first stop for those moving from medical facilities to LTCFs. The goal is to avoid multi-drug resistant organism (MDRO) colonization from these outside medical facilities .13 , 20 Similar rules should be applied to LTCFs as asymptomatically SARS-CoV-2 infected persons or those household contacts with near symptom onset may still transmit SARS-CoV-2.21 All new residents must reside in the LTCF transition zone for the full COVID-19 incubation period before being assigned a living space in the LTCF clean zone. HCWs taking care of new residents held in the transition zone must don standard PPE, adhere to strict infection control and utilize checkpoint hand disinfection when moving between zones.16
Correct clean zone design for LTCFs are necessary because SARS-CoV-2 can be transmitted asymptomatically. As a result, it is clear that standard preventive measures cannot guarantee protection from this SARS-CoV-2 infection. Therefore, the last line of defense must involve mitigation to minimize any possible opportunities for infection to occur.
According to Six Sigma principles, the more you compartmentalize response planning into individual steps, the more likely you are to identify details that might otherwise be overlooked when developing infection control protocols.15 Drawing on Six Sigma, we developed eTCB as a multi-layered system. For example, the clean zone itself is divided into distinct compartments to block the potential spread of SARS-CoV-2 throughout the system (Fig. 1). Compartmentalization can be adapted to specific conditions in each LTCF. For example, while ideally compartmentalization in the clean zone may involve separate buildings, compartmentalization can also occur using different floors within one building, or even distinct wards/blocks on the same floor. Each distinct compartment is staffed by designated staff including a HCW and nurse attendant who do not rotate to other compartments. By remaining in only one compartment, the potential for transmission within the LTCF clean zone and beyond is minimized. Ideally, support staff (including part-time staff working in cleaning, laundry and catering) should also be assigned to only one compartment. However, if staffing is insufficient, support staff should be trained in hand disinfection (to block fomite transmission) in addition to daily environmental cleaning and disinfection to minimize the risk of cross-compartment spread.16
During a pandemic, it is also important to limit to the extent possible regular group activities conducted in public spaces (including public dining). If a gathering is deemed necessary, the public space to be used must be disinfected both in advance of and following the gathering. In addition, participants should be required to wear masks, disinfect their hands (prior to and following any activity), and adhere to proper social distancing. If dining in a common area is necessary, residents should maintain 2 meters separation and refrain from sitting in groups, speaking loudly or laughing, in order to minimize droplet or contact/fomite transmission.22
Checkpoint hand disinfection
Hand disinfection should not be limited to the entrance of the LTCF. We recommend disbursing disinfection stations equipped with alcohol-based hand disinfectant throughout the LTCF between zones and compartments, including at the entrance, in quarantine rooms and throughout public spaces in clean zones. To ensure compliance with hand hygiene guidelines, appropriate signage should be placed as this will increase the likelyhood that everyone engages in hand disinfection appropriately and conveniently, particularly after contacting with fomites in the environment.14 , 17
In clean zones, alcohol-based sanitizer dispensers should be positioned at checkpoints along traffic routes connecting each compartment (Fig. 1). In compliance with eTCB, all personnel transitioning across compartments should follow strict checkpoint hand disinfection and decontamination to ensure hand hygiene and facilitates containment of contact/fomite transmission14 , 17
Specific consideration for medical care in LTCF
LTCF residents tend to be older and suffer from various co-morbidities. As a result, residents depend on receiving regular care from outside healthcare facilities. Once they leave the LTCF, residents are at heightened risk of exposure to infection.
Facilities offering day programming for non-resident elderly
LTCF sometimes provide programming for non-resident elderly. In many cases, both the LTCF and the day programming are accessed through the same entryway and shared lobby. In terms of controlling infection spread, this is not ideal.
Transportation to daily programming for non-resident elderly
Regardless of vehicle types, the vehicle interior should be cleaned with 500 ppm bleach before and after each trip. Drivers should self-monitor their health based on TOCC/symptoms and should wear a mask. To the extent possible, drivers should avoid travelling among multiple facilities during a single trip. All passengers must wear a mask and disinfect their hands before embarking. While in the vehicle, passengers should maintain maximum possible distance from each other.
Checkpoint control at facility entrances
Where separate entrances are not an option, LTCF residents and those coming for day programs should have staggered access times. Between these times the facility entrance should be disinfected to restore clean zone conditions.
Nursing homes
Many elderly people reside in nursing homes. Those in independent living are able to care of themselves. They often live alone or in couples in a single suite or separate apartment. They are free to engage in social and leisure activities throughout the community. However, during a pandemic, these residents must adhere to strict guidelines and, when moving through their facility must maintain safe social distance.8 Residents' basic needs should be purchased through the LTCF central agency. Any resident who exits the facility must quarantine for two weeks upon returning to the facility.
Within nursing homes there is often a dependent living section. Dependent living residents are unable to care for themselves. These residents must be segregated from the rest of the nursing home residents. Ideally segregation involves separate buildings, or at minimum, separate floors.
Skilled nursing department
Residents of Skilled Nursing are least independent, living in conditions close to those found in hospitals. During the COVID-19 outbreak, visiting skilled nursing should be banned in order to protect this population. This is supported by evidence from a 2020 Taiwan Centers for Disease Control (TCDC) study that found especially high attack rate among household contact.21 , 23 As an alternative to physical visits, family and friends should resort to video meetings.24 When urgent needs occur, meeting with residents should only occur in a controlled public area such as lobby, should be limited to 30 min and should involve social distancing of 3 meters and no physical contact.
Managing medical needs
To the extent possible, reduce all hospital visits. Many medical needs can be met through telemedicine or applying “the hospital at home” program where a physician visit the patient in the LTCF.25 If residents need to refill prescriptions for medications, these should be obtained by LTCF employees on their behalf. Should residents seek to attend a regularly scheduled hospital visit, they should first consult with their physician regarding alternatives to physical meetings. If hospital visits are required such as cancer therapy or rehabilitation, they should be minimized during this critical time period and a number of steps taken:
Hospitals implementing eTCB are most likely to be safe for LTCF residents. For example, considering a visit for hemodialysis (HD). To minimize the danger of infection, hospitals designed with eTCB usually compartmentalize their HD ward into different compartments operating on different time schedules. However, as routine visits for hemodialysis remains high risk opportunities for COVID-19 infection, patients coming from HD treatment should be closely monitored for COVID-19 symptoms as well as daily activity in a controlled area of the clean zone.
LTCF residents admitted to hospital should be quarantined for two weeks following discharge and return to the facility. Ideally, residents returning to the LTCF after a hospital visit should be placed in 14 day quarantine and isolated from all other residents in their compartment. This approach necessitates additional staff and space. However, recognizing that facilities lack adequate space and will therefore struggle to implement the quarantine, we recommend that residents returning from hospital visits be concentrated in one designated compartment where they undergo observation for the 14 day quarantine period.
Case surveillance, reporting and managing clusters/outbreaks
As LTCFs are extremely vulnerable to SARS-CoV-2, LTCF staff should expect an outbreak within their facility. The TCDC provides important support to LTCFs. It has developed and implemented syndromic surveillance for all facilities with high population densities including LTCFs. Surveillance includes collecting data based on region as well as age-specific COVID-19 cases. Data are also collected on those presenting symptoms of COVID-19 who have yet to be tested.26, 27, 28 Once an index case has been identified,the LTCF's should view this as evidence it is suffering either weak control at its entrance or unidentified COVID-19 clusters within its facility. In response, facility administrators should immediately launch an epidemiological investigation coupled with contact tracing to identify any additional cases. As discussed below, there are additional steps that LTCF should then take.
Plan for on-site management
As eTCB incorporates compartmentalization, it is possible to transfer residents in the same compartment as the index case to a quarantine zone (Fig. 1). The quarantine zone may be within the same facility or in a separate location. Because of the compartmentalization it is possible for the remaining compartments in the LTCF to continue operations as usual, though heightened surveillance and infection control should be implemented.
Plan for evacuation/shut down
Should the facility fail to effectively implement eTCB, there may be more than one compartment affected and an epidemic surge bacomes increasingly likely. In such a case, the entire facility is at risk. The recommended action is to remove the sick to hospital, shut down the facility and evacuate all residents and HCWs while the facility undergoes disinfection prior to reopening. Until the facility is safe, evacuated residents/HCWs should be housed in another healthcare setting that has implemented eTCB. Those who tested negative for COVID-19 should be housed in compartments separate from those who tested positive, both for quarantine and further management.29
Realities and limitations
We recognize that the recommendations made here describe ideal conditions. We are aware that there will be overcrowding in LTCFs and that there will be shortage of space, PPE, and well trained staff. In responding to COVID-19, we therefore urge LTCFs to view these recommendations as a gold standard. LTCF officials should familiarize themselves with the recommendations and then adapt them to their own realities, seeking where possible to adhere to them closely.
In anticipation of future outbreaks, when considering allocation of scarce resources, LTCF officialswith government support should prioritize conducting a systematic audit in order to identify gaps in preparedness. Based on the audit, LTCF officials and government officials should together develop top-down planning and training programs for staff and residents, including counseling programs. They should also ensure adequate human resources and PPE exist to provide surge capacity when needed.
As environmental cleaning, disinfection and checkpoint hand cleaning is of particular importance during an epidemic, these should be prioritized when training LTCF HCWs and support staff.
Conclusion
As the COVID-19 pandemic has caused high case-fatality rates in many parts of the world, we advocate here to start by minimizing infection through public health prevention measures successfully implemented in Taiwan. These measures include eTCB as well as active surveillance, particularly of the elderly residing in LTCFs. As we note, eTCB has proven effective at limiting droplet and fomite transmissions both within hospitals and between hospitals. By effectively adapting eTCB to LTCFs, with further compartmentalization of clean zones plus active integrated syndromic and virological surveillance, we argue that eTCB can and should be adopted and implemented as a means of protecting LTCF residents and staff, thus saving lives within this vulnerable population.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Acknowledgement
The funding of the retrospective study in confirming the efficacy of traffic control bundling (reference 16. Yen MY, et al. Taiwan's traffic control bundle and the elimination of nosocomial severe acute respiratory syndrome among health care workers. J Hosp Infect 2011; 77:332–7.) was financially supported by Taiwan CDC grant (DOH 92-DC-SA01) in 2003.
References
- 1.Taylor D.B. The New York Times, A timeline of the coronavirus pandemic. 2020. https://www.nytimes.com/article/coronavirus-timeline.html available from:
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. Published online February 24. [DOI] [PubMed] [Google Scholar]
- 3.Utsumi M., Makimoto K., Quroshi N., Ashida N. Types of infectious outbreaks and their impact in elderly care facilities: a review of the literature. Age Ageing. 2010;39:299–305. doi: 10.1093/ageing/afq029. [DOI] [PubMed] [Google Scholar]
- 4.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 Mar 23 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 5.Johnson C.K., Stobbe M. Sick Workers fueled coronavirus outbreak in Seattle-area care centers: CDC. 2020. https://time.com/5805823/seattle-nursing-home-coronavirus-investigation/
- 6.McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G. Epidemiology of COVID-19 in a long-term care facility in King County, Washington. New Engl J Med. 2020 doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Infection prevention and control guidance for long-term care facilities in the context of COVID-19 interim guidance. 21 March 2020. https://apps.who.int/iris/handle/10665/331508 [Google Scholar]
- 8.Preparing for COVID-19: Long-term Care Facilities, Nursing Homes. Centers for Disease Control and Prevention (CDC) 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Fpreventspread- in-long-term-care-facilities.html
- 9.Gaillat J., Chidiac C., Fagnani F., Pecking M., Salom M., Veyssier P. Morbidity and mortality associated with influenza exposure in long-term care facilities for dependent elderly people. Eur J Clin Microbiol Infect Dis. 2009;28:1077–1086. doi: 10.1007/s10096-009-0751-3. [DOI] [PubMed] [Google Scholar]
- 10.Haber N. Respiratory syncytial virus infection in elderly adults. Med Maladies Infect. 2018;48:377–382. doi: 10.1016/j.medmal.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Tse M.M., Pun S.P., Benzie I.F. Experiencing SARS: perspectives of the elderly residents and health care professionals in a Hong Kong nursing home. Geriatr Nurs. 2003;24:266–269. doi: 10.1016/S0197-4572(03)00251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai C.C., Liu Y.H., Wang C.Y., Wang Y.H., Hsueh S.C., Yen M.Y. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARSCoV-2): facts and myths. J Microbiol Immunol Infect. 2020;53:404–412. doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith P.W., Bennett G., Bradley S., Drinka P., Lautenbach E., Marx J. SHEA/APIC Guideline: infection prevention and control in the long-term care facility. Infect Control Hosp Epidemiol. 2008;29:785–814. doi: 10.1086/592416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yen M.Y., Schwartz J., Chen S.Y., King C.C., Yang G.Y., Hsueh P.R. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020;53:377–380. doi: 10.1016/j.jmii.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yen M.Y., Chiu A.W.-H., Schwartz J., King C.C., Lin Y.E., Chang S.C. From SARS in 2003 to H1N1 in 2009: lessons learned from Taiwan in preparation for the next pandemic. J Hosp Infect. 2014;87:185–193. doi: 10.1016/j.jhin.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yen M.Y., Lin Y.E., Lee C.H., Ho M.S., Huang F.Y., Chang S.C. Taiwan's traffic control bundle and the elimination of nosocomial severe acute respiratory syndrome among health care workers. J Hosp Infect. 2011;77:332–337. doi: 10.1016/j.jhin.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz J., King C.C., Yen M.Y. Protecting health care workers during the COVID-19 coronavirus outbreak-lessons from Taiwan's SARS response. Clin Infect Dis. 2020 March 12 doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sehwail L., DeYong C. Six Sigma in health care. Leader Health Serv. 2003;16:1–5. [Google Scholar]
- 19.Taiwan Centers for Diseases Control Taiwan timely identifies first imported case of 2019 novel coronavirus infection returning from Wuhan, China through onboard quarantine; Central Epidemic Command Center (CECC) raises travel notice level for Wuhan, China to Level 3: Warning. 2020. https://www.cdc.gov.tw/En/Bulletin/Detail/pVg_jRVvtHhp94C6GShRkQ?typeid=158
- 20.Liu C.Y., Lai C.C., Chiang H.T., Lu M.C., Wang L.F., Tsai T.L. Predominance of methicillin-resistant Staphylococcus aureus in the residents and environments of long-term care facilities in Taiwan. J Microbiol Immunol Infect. 2019;52:62–74. doi: 10.1016/j.jmii.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H. High transmissibility of COVID-19 near symptom onset. medRxiv bioRxiv. March 19, 2020 doi: 10.1101/2020.03.18.20034561. [DOI] [Google Scholar]
- 22.Xie X., Li Y., Sun H., Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009;6:S703–S714. doi: 10.1098/rsif.2009.0388.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCleary L., Munro M., Jackson L., Mendelsohn L. Impact of SARS visiting restrictions on relatives of long-term care residents. J Soc Work Long Term Care. 2006;3:3–20. [Google Scholar]
- 24.WHO . 2020. Video on COVID-19: stay at home! the importance of social distancing, Mar. 17, 2020.https://www.ecdc.europa.eu/en/publications-data/video-covid-19-stay-home-importance-social-distancing [Google Scholar]
- 25.Leff B. A vision for “hospital at home” programs. Harvard Bus Rev. 2015 https://hbr.org/2015/12/a-vision-for-hospital-at-home-programs [Google Scholar]
- 26.Taiwan centers for disease control (Taiwan-CDC) 2019. https://www.cdc.gov.tw/Category/MPage/hxfvlpFPB8MM3_tU9-5UnA
- 27.Wu T.S., Shih F.Y., Yen M.Y., Wu J.S., Lu S.W., Chang K.C. Establishing a nationwide emergency department-based syndromic surveillance system for better public health responses in Taiwan. BMC Publ Health. 2008;8:18. doi: 10.1186/1471-2458-8-18. PMID: 18201388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheng H.Y., Chen W.C., Chou Y.J., Huang A.S.E., Huang W.T. Containing influenza outbreaks with antiviral use in long-term care facilities in Taiwan, 2008-2014. Influ Other Respir Virus. 2018 Mar;12(2):287–292. doi: 10.1111/irv.12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen W.T., CNA Nursing staff first confirmed of COVID-19 pneumonia in long term care facility. March 22, 2020. https://www.cna.com.tw/news/firstnews/202003225007.aspx