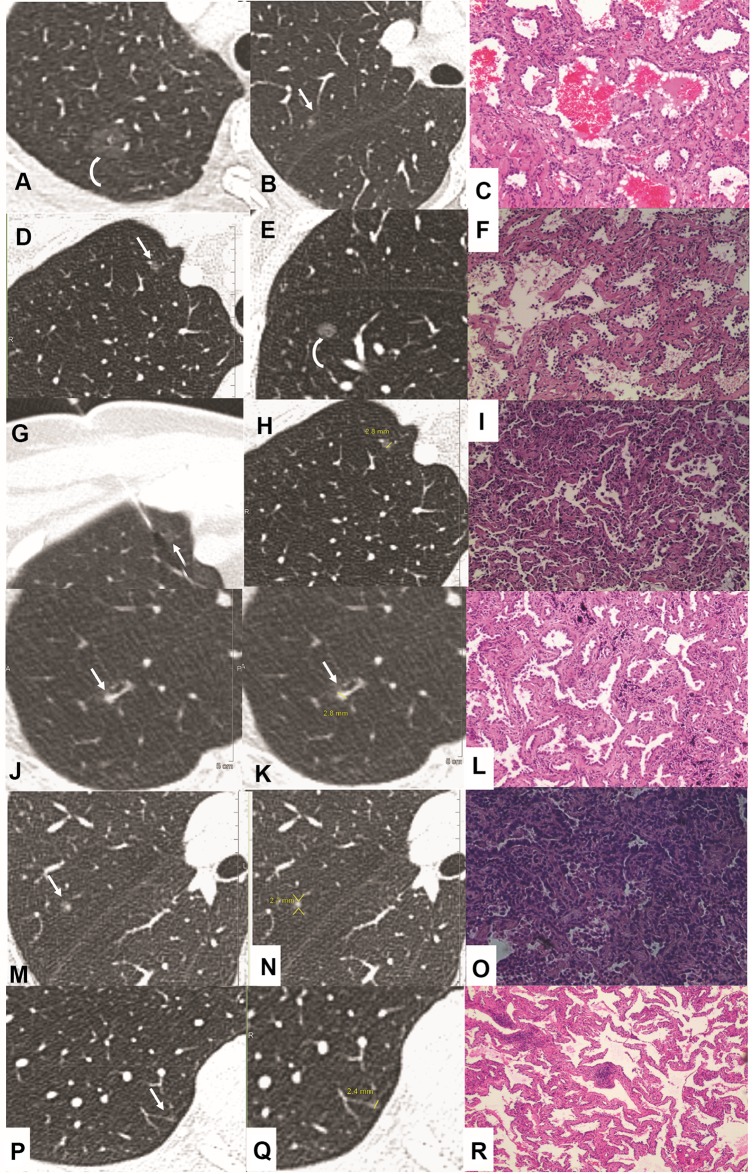
Figure 5.
Imaging and pathology in patients with pulmonary nodules<3 mm in size at baseline CT (hematoxylin and eosin staining). Case 1(A–C): Transverse 1.5-mm CT sections showed two sub-solid nodules in the right upper lobe. (A) Growth developed in the pure ground glass nodule (A, curve arrow) at 2 years follow-up CT. Surgical resection was performed with the diagnosis of minimally invasive adenocarcinoma (MIA). (B, C) However, the incidentally resected nodule (B, arrow) in the same lobe proved to be acinar predominant adenocarcinoma (C, magnification: ×200). Case 2(D–I): Transverse 1.0-mm CT sections showed two sub-solid nodules in the right upper (D, G, H) and lower lobe (E). (E, F) Solid component developed (E, curve arrow) during 1 year follow-up, and resection was performed with a diagnosis of chronic inflammation (F, magnification: x100). (D, G–I) CT guided location was performed (G, H, arrow) for the following surgery with a diagnosis of MIA (I, magnification: ×40). Case 3(J–L): Highly suspicious case with a persistent solid nodule (J–K, arrow) and developed bronchiectasis. Surgery was performed with a diagnosis of MIA (L, magnification: ×100). Case 4 (M–O): Incidentally resected nodule (M, arrow) with a diagnosis of acinar predominant adenocarcinoma (O, magnification: ×100). Case 5 (P–R): Incidentally resected nodule (P, arrow) with a diagnosis of adenocarcinoma in situ (AIS) (R, magnification: ×40).