Figure 1. Bile acid signaling in the intestine.
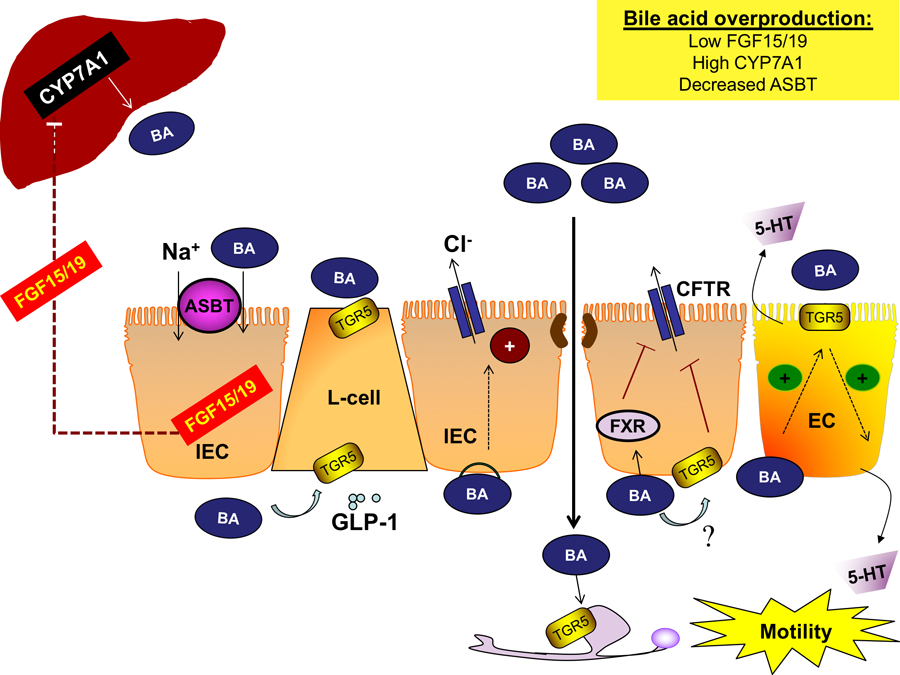
Bile acids are synthesized in the liver by the rate-limiting enzyme CYP7A1 and secreted into the intestine. Bile acids are reabsorbed by IECs in the distal ileum via ASBT where they activate FXR, inducing the expression and secretion of FGF15/19 to inhibit hepatic bile acid synthesis. Luminal and basolateral bile acids activate TGR5 in enteroendocrine L-cells, resulting in the release of the incretin GLP-1, promoting glucose tolerance. Overproduction of bile acids can promote diarrhea by several distinct mechanisms. In the colon, bile acids disrupt barrier integrity allowing bile acids to reach the basolateral membrane of epithelial cells and induce chloride secretion, though the receptor(s) underlying this phenomenon is unknown. Interestingly, colonic FXR and TGR5 activation inhibits the secretion of chloride and other electrolytes, which may be a compensatory mechanism. Excessive bile acids also promote gut motility. Colonic bile acids activate TGR5 on ECs, promoting 5-HT release and motility. Bile acids activate neuronal TGR5, which either stimulates or inhibits motility, depending on the type of neuron and region of the GI tract. Overall, overproduction of bile acids induces colonic secretion and enhances motility, producing a diarrheal phenotype. Abbreviations: 5-HT, 5-hydroxytryptamine; ASBT, apical sodium-dependent bile acid transporter; BA, bile acid; CFTR, cystic fibrosis transmembrane conductance regulator; CYP7A1, cytochrome P450 7A1; EC, enterochromaffin cells; FGF15/19, fibroblast growth factor 15/19; FXR, farnesoid X receptor; GI, gastrointestinal; GLP-1, glucagon-like peptide-1; IEC, intestinal epithelial cell; TGR5, Takega G protein-coupled receptor 5
