Abstract
During the extensive outbreak of coronavirus disease 2019 (COVID-19) in South Korea, many strategies in the hospital setting, such as stratified patient care, the assignment of hospitals/beds by a task force team, and the establishment of dedicated COVID-19 hospitals, dedicated COVID-19 emergency centers, COVID-19 community facilities, and respiratory care split hospitals, were adopted to mitigate community transmission and prevent nosocomial infection. Most of these strategies were used during the Middle East Respiratory syndrome outbreak and were applied again successfully during the COVID-19 outbreak. The reallocation of health care capacity, repurposing of hospitals, and close collaboration between the government and the health care committee might have been the key to successfully addressing the crisis of COVID-19 given the shortage of health care resources.
Keywords: COVID-19, Outbreak, Nosocomial infection, South Korea
Highlights
-
•
Repurposing and reshaping of hospitals could be working on containing COVID-19 outbreak and limiting nosocomial infections.
-
•
Dedicated COVID-19 hospitals and COVID-19 emergency centers provided focused care during COVID-19 outbreak in South Korea.
-
•
COVID-19 community facilities and respiratory care split hospitals were established to mitigate the outbreak in South Korea.
-
•
Reallocation of healthcare personnel/facilities was critical given the shortage of health care resources.
1. Introduction
The fear of coronavirus disease 2019 (COVID-19) has spread all over the world. Chinese doctors first recognized the COVID-19 outbreak in December 2019, and we are now in the middle of a battle against it, which we are fighting without any specific treatments. With an exponential increase in the number of COVID-19 patients, the fight against COVID-19 has now entered a new chapter.
South Korea was strongly affected by COVID-19 very early, and it was the most affected country outside of China in the beginning. However, due to the rigorous efforts and stringent regulations, the incidence of new cases is abating. More noticeably, the case fatality rate in South Korea was 2.1% compared to an approximate case fatality rate of 6–7% worldwide [1,2]. The paper by Her et al. described in detail how COVID-19 spread in South Korea and what strategies were used for the early detection and isolation of cases [3]. In addition to extensive COVID-19 screening and rigorous contact tracing, stratified patient care was effectively applied in hospitals nationwide to care for COVID-19 patients.
During the Middle East Respiratory syndrome (MERS) outbreak in South Korea in 2015, South Korea was the hardest hit country outside of the Middle East. The infection rate related to hospitals was 40–90%, and the fatality rate was reported to be 19% [4,5]. During the MERS outbreak, the MERS taskforce team, MERS-dedicated hospitals, and respiratory care split hospitals were established to decrease nosocomial infections and avoid closing hospitals due to contagion. During the COVID-19 outbreak, we adopted those strategies from the beginning, and the COVID-19 community facility and dedicated COVID-19 emergency center were also established to address the transmission of COVID-19. This paper details how the lessons learned during the MERS outbreak were applied to contain the spread of COVID-19, especially in hospital settings in South Korea.
2. Stratified patient care directed by task force team and repurposing of treatment locations
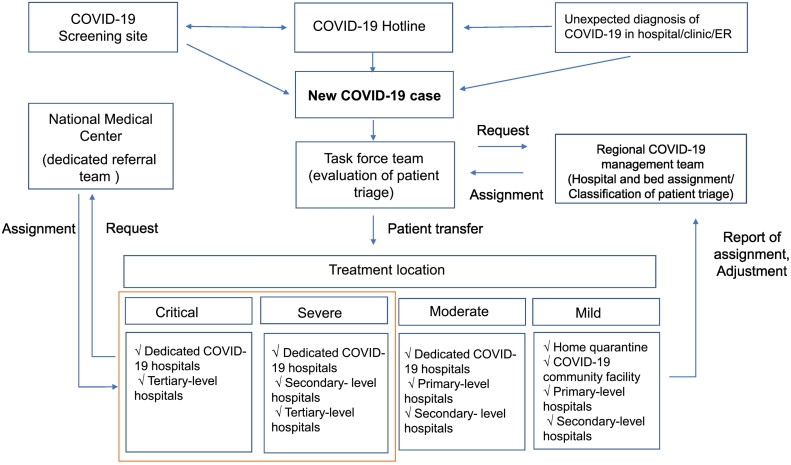
During the massive outbreak in Daegu, the epicenter of COVID-19 in South Korea, the shortage of beds would led to patient deaths due to the lack of timely care. Increasing the number of beds and reallocating health care personnel and facilities was needed to provide optimal health care. Therefore, the treatment locations were strategically determined by a collaboration between health care personnel and the task force team (Fig. 1) [6]. When a new confirmed COVID-19 case was detected, the COVID-19 task force team and regional COVID-19 management team were notified of the result. The regional COVID-19 management team assigned the patients to hospitals and beds depending on the disease severity and room availability. The treatment locations were divided into home quarantine, COVID-19 community facility, dedicated COVID-19 hospitals, and primary, secondary and tertiary hospitals, and the assignment was based on the results of patient triage. Those systems worked to offer focused patient care, distribute the medical burden and prevent a shortage of beds.
Fig. 1.
Stratification of hospital/room assignments (Edited from the figure pertaining to assignments of beds/hospitals during the COVID-19 outbreak [6])
3. COVID-19 community facility
The COVID-19 community facility was first launched in March 2020 in Daegu to care for patients with mild cases and monitor them using preexisting nonmedical infrastructure and the minimum of health care resources. In Daegu, the sudden increase in patients was threatening to cause a shortage of hospital rooms, and the number of beds needed to be increased. Mild patients were expected to quarantine at home, but some mild patients still needed to be monitored. Community facilities that were originally used for nonmedical purposes, such as training centers, resorts, and dormitories, were repurposed as monitoring stations for patients with mild COVID-19. Usually, freestanding buildings with good ventilation systems were used. Patients who do not need oxygen, especially those younger than sixty-five years old without underlying diseases, were candidates for monitoring in the COVID-19 community facility [7]. While patients stayed in the patients' zone, patients reported their body temperature and any symptom changes using a mobile app or the telephone twice a day [8]. Their general condition was monitored by health care professionals. Chest X-ray, pulse oximetry, and COVID-19 reverse transcription polymerase chain reaction (RT-PCR) test could be performed there, and simple medication such as antipyretics could be prescribed [8]. If their symptoms showed clinically meaningful changes, they were transferred to the hospital.
By running this system, hospitals could secure enough rooms for patients who needed further evaluation and treatment or intensive care. Additionally, even patients with mild COVID-19 could rapidly deteriorate while in home quarantine. If they were monitored in the community facility, they could be transferred to the hospital without delay. As of now, more than fourteen COVID-19 community facilities have been working successfully, and the number has continued to increase.
4. Dedicated COVID-19 hospital and COVID-19 emergency center
Dedicated COVID-19 hospitals are the hospitals take care of COVID-19 patients only. The majority were public health care hospitals that are run by the government, and some secondary and tertiary private hospitals were included. In total, sixty-seven hospitals offering more than 7000 beds became dedicated COVID-19 hospitals nationwide. Dedicated COVID-19 hospitals were renovated to ensure they had a negative-pressure isolation room, negative-pressure transport chamber, anteroom, dividing walls and enough space between beds. Usually, they treat moderate to severe/critical patients depending on the facility. For example, Dongsan Hospital in Daegu, a hot spot for COVID-19, had more than 400 beds to care for mainly severe/critical COVID-19 patients. If the number of health care personnel and resources were insufficient, they could be dispatched from other hospitals.
The dedicated COVID-19 emergency center was the center for potential COVID-19 patients who needed emergency treatment. In South Korea, most COVID-19 patients were diagnosed at the COVID-19 screening sites, of which there were more than 600 [3]. Easy access to COVID-19 screening sites meant that patients were diagnosed early and received proper treatment early, preventing unexpected visits of potential COVID-19 patients to the emergency room. Despite these efforts, COVID-19 patients could suddenly deteriorate before their admission. Dedicated COVID-19 emergency centers were usually the emergency rooms of tertiary-level hospitals with negative-pressure isolation rooms.
Through the use of dedicated COVID-19 hospitals and emergency centers, the patients were received focused care, and health care professionals and personal protection equipment were rationally allocated to address the outbreak. Additionally, other hospitals are still operational and could take care of patients with other diseases and other emergency situations.
5. Respiratory care split hospital
During the MERS outbreak in 2015 in South Korea, 40–90% of cases were related to nosocomial infections, and superspreaders were reported in hospitals [4,5] Although the exact number of nosocomial infections of COVID-19 in South Korea has not yet been reported, the hospital infection rate has increased to 4–7%, especially given the shortage of hospital resources, as in China [9,10].
Respiratory care split hospitals separated patients who had respiratory symptoms from patients without respiratory symptoms from the initial visit to the outpatient clinic through the duration of hospitalization. The purpose of this hospital is to limit unnecessary contact between respiratory patients who might have COVID-19 and other patients to minimize the transmission of COVID-19 in hospitals. Additionally, patients without respiratory symptoms could receive proper treatment for their diseases with less concern about being unexpectedly exposed to COVID-19 in the hospital.
The entrance to and the location of the respiratory disease outpatient clinic was separate from the main hospital, and the transit routes of the patients with respiratory diseases were separate from those of other patients. If the patients were suspected of having COVID-19 based on their symptoms or epidemiological factors, they were sent to the COVID-19 screening site first and then the dedicated COVID-19 hospital, not the outpatient clinic or inpatient ward of the respiratory care split hospital.
All patients who had respiratory symptoms were admitted to the designated floor or building. Most patients were tested for COVID-19 before their admission to the respiratory department. Based on their symptoms, patients with respiratory symptoms had to stay on their own floor or in their own room. Among the approximately 3600 hospitals nationwide, more than three hundred hospitals have reshaped their facilities to function as respiratory care split hospitals during the COVID-19 outbreak. Isolating respiratory patients during the whole process meant that the remaining areas could be protected from unexpected exposure to contagion. However, despite these efforts, unexpected hospital infections sometimes occurred.
6. Conclusion
During the MERS outbreak in 2015, South Korea had the 2nd largest outbreak after Saudi Arabia. The lack of preparation for an emerging infectious disease, an improper approach to preventing nosocomial infections, the poor detection of close contacts and lack of isolation of patients with confirmed cases were all heavily criticized. However, during the MERS outbreak, many strategies were devised that have been successfully adopted during the COVID-19 outbreak, such as the creation of task force teams for COVID-19, dedicated COVID-19 hospitals, dedicated COVID-19 emergency centers, COVID-19 community facilities, and respiratory care split hospitals.
Extensive screening for COVID-19 and meticulous contact tracing are regarded as having been key to controlling COVID-19 in South Korea. However, more detailed approaches were applied in every step to flatten the curve and lower the risk of nosocomial infection. The close collaboration among the health care department, municipal government and national government, and public acceptance of stringent hospital restrictions were also important.
The COVID-19 outbreak has entered a new chapter, and many countries face trying to effectively control this outbreak with limited resources and protect healthcare personnel. The repurposing and reshaping of hospitals and the reallocation of healthcare personnel and facilities might be critical to prepare for the next wave of COVID-19.
Declaration of Competing Interest
None of the authors have any conflict of interests.
Acknowledgements
None. No funding to declare.
References
- 1.Korean centers for Disease Control and Prevention. Coronavirus Disease-19. Republic of Korea; 2020. http://ncov.mohw.go.kr/ accessed April 17, 2020. [Google Scholar]
- 2.COVID 19 Dashboard by the Center for systems science and Engineering (CSSE) at Johns Hopkins University (JHU) 2020. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed April 17,2020) [DOI] [PMC free article] [PubMed]
- 3.Her M. How is COVID-19 affecting South Korea? What is our current strategy? Disaster Med. Public Health Prep. 2020;3:1–3. doi: 10.1017/dmp.2020.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim K.H., Tandi T.E., Choi J.W., Moon J.M., Kim M.S. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. J. Hosp. Infect. 2017;95:207–213. doi: 10.1016/j.jhin.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oh M.D., Park W.B., Park S.W., Choe P.G., Bang J.H., Song K.H. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J. Intern. Med. 2018;33:233–246. doi: 10.3904/kjim.2018.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Strategies against Coronavirus Disease-19 Outbreak. 7–4 edition. 2020. Korean centers for Disease control and prevention.http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=28 (accessed April 17,2020) [Google Scholar]
- 7.Management for Coronavirus Diseas-19 Community Facilities. 2020. Korean centers for Disease control and prevention.http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=28 (accessed April 17,2020) [Google Scholar]
- 8.Park P.G., Kim C.H., Heo Y., Kim T.S., Park C.W., Kim C.H. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J. Korean Med. Sci. 2016;35 doi: 10.3346/jkms.2020.35.e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 10.He Y., Li W., Wang Z., Chen H., Tian L., Liu D. Nosocomial infection among patients with coronavirus disease-2019: a retrospective data analysis of 918 cases from a single center in Wuhan city. China.Infect. Control Hosp. Epidemiol. 2020 Apr;13:1–6. doi: 10.1017/ice.2020.126. [DOI] [PMC free article] [PubMed] [Google Scholar]