Abstract
The risk of vertical transmission during vaginal delivery in COVID-19 pregnant patients is currently a topic of debate. Obstetric norms on vaginal birth assistance to reduce the potential risk of perinatal infection should be promoted by ensuring that the risk of contamination from maternal anus and faecal material is reduced during vaginal delivery.
Keywords: COVID-19, SARS-CoV-2, Pregnancy outcome, Vertical transmission, Maternal feacal contamination, Neonatal outcome, Vaginal, Mode of delivery
Introduction
The World Health Organization (WHO) named the new coronavirus (SARS-CoV-2) disease Coronavirus Disease 19 (COVID-19) and have stated that COVID-19 is a pandemic. SARS-CoV-2 is a betacoronavirus, similar to SARS-CoV and MERS-CoV, with multiple possible transmission routes, including fecal-oral, and is characterized by a high infectivity [1,2].
The outcomes of perinatal COVID-19 in infants are still under debate. Differently to some reassuring data about neonatal outcomes [3], other reports have discussed adverse effects on newborns, such as fetal and respiratory distress, thrombocytopenia accompanied by abnormal liver function and even death [4].
Concern is rising on the possibility that SARS-CoV-2 may be vertically transmitted [5], even if current evidence is inconclusive. IgM virus-specific antibodies have recently been detected in neonatal blood sera samples, obtained from one mother who tested positive for COVID-19 [6]. However, as SARS-CoV-2 was not detected in amniotic fluid, cord blood or breastmilk [7] at RT-PCR assays, this may exclude two possible vertical transmission pathways, i.e. intrauterine infection and breastfeeding.
Vertical transmission can also occur during vaginal delivery, through neonatal contact with fluids of both the vagina and the rectum, as is already well known for pathogens such as Group B Streptococcus [8] and Human Papilloma Virus (HPV) [9]. The presence of SARS-CoV-2 in the vaginal fluid of women with severe COVID-19 has been excluded [10]. However, SARS-CoV-2 has been found in the stools of one out of three non-pregnant positive COVID-19 patients [2]. The first potential vertical transmission, occurring during vaginal delivery in a COVID-19 positive pregnant woman with rectal and stool maternal positive swabs for SARS-CoV-2, has recently been reported [11]. This case suggests that SARS-CoV-2 can enter the neonatal nasopharynx during vaginal delivery, potentially triggering neonatal infection.
Current recommendations for pregnant women who tested positive for COVID-19 suggest that delivery mode should be determined primarily by obstetric indication and the mode of birth should not be influenced by the presence of COVID-19, unless the woman’s respiratory condition demands urgent intervention for birth complications [12,13].
Practical limitations of Pre-labour screening
On the basis of this evidence, we suggest a pre-labor anorectal swab be taken from pregnant women who test positive for COVID-19 to identify newborns at risk of perinatal infection and reduce the potential risk of vertical transmission [11]. However, the heavy workloads laboratories currently have to deal with for the diagnosis of COVID-19 worldwide makes the hypothesis of further scaling up for anorectal screening in all women programmed for vaginal birth and potential SARS-CoV-2 carriers, an unlikely proposition. Currently, there is no strong evidence in support of elective Caesarean section (CS) either in these patients if anorectal swab results are not available.
We propose some preventive measures to be taken in an effort to reduce the potential risk of vertical transmission of SARS-CoV-2 during vaginal birth in women. This advice is not intended to replace that proposed by international associations, such as the WHO, RCOG and ACOG, and should rather be considered additional information provided in the light of the most recent evidence on the consequences of COVID-19 in pregnancy and during vaginal birth.
Advice and Rationale for prevention of potential vertical transmission of COVID-19 at Vaginal delivery
Recommendation 1
An admission evaluation should be made in the obstetric unit, taking accurate notes of when the woman tested positive for COVID-19. Data on the type and timing of the onset of any signs and symptoms that could have been associated with the COVID-19 infection should be collected.
Rationale
Although the typical incubation period for COVID-19 is about five days, it may range from two to 14 days [14].
The most common symptoms are fever, acute persistent cough, hoarseness and/or nasal discharge/congestion, although diarrhea has also been reported in 2.0–10.1% of patients who tested positive for COVID-19 [15].
Recommendation 2
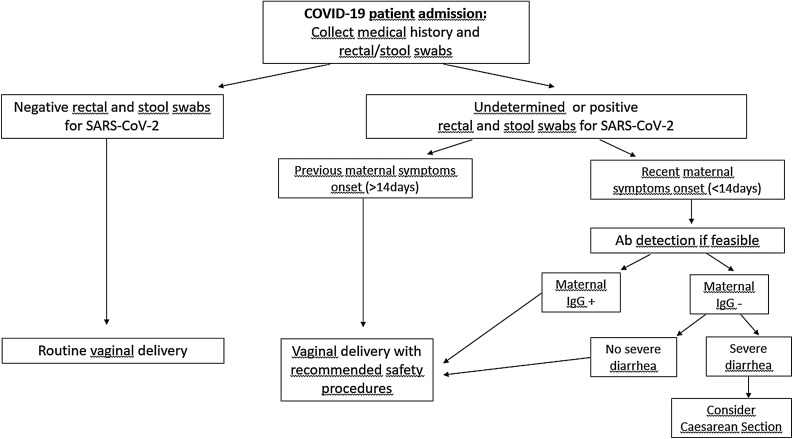
A rectal and stool swab should be taken if there is an adequately equipped reference laboratory available (see Flowchart 1 ).
Chart 1.
Pathway showing how to deal with COVID-19 Pregnant women in Labour (Flowchart 1).
Rationale
SARS-CoV-2 has been found in the stools of non-pregnant and pregnant patients with COVID-19 [1,9]. Patients with a positive rectal and/or stool test did not always have gastrointestinal symptoms and the presence/absence of these symptoms had no association with the severity of the lung infection [16].
It has been estimated that IgG can be detected in positive patients’ serum 14 days after symptom onset [17] and reported that SARS CoV-2 IgG can be passively transferred across the placenta from mother to fetus [18]. Among women who had a recent appearance of COVID 19 symptoms, there may not have been enough time for the development and the transplacental passage of IgG antibodies. These infants are possibly at greater risk of developing severe COVID-19 if infected at birth.
Recommendation 3
Routine vaginal delivery can be proposed if the woman has negative rectal and faecal swabs. Should swab results not be available, vaginal birth can be proposed once the safety measures listed below have been carried out, at least in patients who do not have severe diarrhea (see Flowchart 1).
Recommendation 4
Enema during the prodromic phase and/or the first stage of labour is not recommended.
Rationale
Although enema could potentially avoid stool leakage during the second stage of labour, reducing the amount of viral load at birth, current evidence on neonatal infections other than SARS-CoV-2, do not support its systematic use [19].
Recommendation 5
Water birth is not recommended.
Rationale
Should rectal and stool swab results not be available and as SARS-CoV-2 has been detected in the rectum and faeces of one out of three non-pregnant patients, delivery in water should not be allowed, since water birth promotes the dispersal of faecal material [16]. If both pre-labour swabs are negative, there is currently no evidence to favour one mode of birth over another and, therefore, the mode of birth should be discussed with the woman, taking into consideration her preferences.
Recommendation 6
During the second stage of labour, all positions that allow proper visualization and hygiene of the genito-anal area should be used.
Rationale
Women should be encouraged to adopt any position they find comfortable during the early phase of the second stage of labour [20]. However, in order to facilitate disinfection of the external genitalia and reduce contact with maternal faecal material, vaginal birth should be performed in a position that ensures proper visualization of the anus to reduce the risk of neonatal contamination with faecal material.
Recommendation 7
Clean the perineum with standard disinfection methods before the second stage of labour and when the fetal head is engaged or after bowel movement.
Rationale
The virus is susceptible to simple disinfectants, such as Povidone‐iodine (7.5%) or Chlorhexidine (0.05%) [21].
Perineal care involves thorough cleaning of the patient’s external genitalia and surrounding skin, for at least 5 min. Recommended disinfectants should be used to wash the labia majora, inner labia and anal area. The non-dominant hand should gently retract the labia from the thigh and the inside of skin folds be washed with the dominant hand. Wiping should be done from front to back, from perineum to rectum. This process should be repeated on the opposite side, using new sterile swabs. The area should then be rinsed and dried thoroughly.
Recommendation 8
Preferably use warm compresses, soaked in recommended disinfectant, which should be applied onto the perineum during the second stage of labour to prevent severe perineal trauma.
Rationale
Warm compresses, applied during the second stage of labour, and selective episiotomy policies should be adopted to lower the risk of severe perineal trauma [22,23], including sphincter and rectal damage. A midline episiotomy is likely to extend into the anal sphincter causing a third- or fourth degree tear and should, therefore, be avoided [23].
Recommendation 9
Apply a discreet sticky anoperineal dressing to cover the anus before the expulsion phase of the presenting part. Once the fetal head has crowned from the vaginal canal, place your hand covered by a sterile glove between the nose and mouth of the newborn and the perineum, whilst waiting for the next contraction.
Rationale
Contact of the head, in particular the nasopharynx and neonatal conjunctiva, with the maternal anus should be avoided to reduce the risk of the newborn being contaminated with faecal material. Should the neonate come into contact with faeces, its face should be washed thoroughly with soap and water immediately.
Recommendation 10
Try to avoid instrumental delivery to minimize risk of third- or fourth- degree perineal tears, hemorrhage and potential risk of infection to the obstetrician.
Rationale
Instrumental vaginal delivery is the most significant risk factor for post partum hemorrhage and obstetric anal sphincter injuries, even with elective mediolateral episiotomy [24] and therefore should be performed only when unavoidable. The risk factors for obstetric anal sphincter injury include primiparity, macrosomia and occipito- posterior position [25]. Appropriate care should be taken to minimize risks to the women from post partum hemorrhage and pelvic floor injuries.
Recommendation 11
Caesarean section should be considered in women who tested positive for COVID-19 with a recent onset of symptoms (<14 days) and with severe diarrhea that compromise the aforementioned standard procedures, as the risk of perinatal transmission is higher and the development of neonatal COVID-19 cannot be excluded (see Flowchart 1).
Rationale
The presence of diarrhea does not allow the exclusion of pre-labour vaginal and/or neonatal contamination during vaginal delivery. If a recent onset of maternal symptoms has been reported, then the newborn is potentially at a higher risk of developing COVID-19 infection, due to the absence of maternal IgG in their serum, that usually appears 14 days after the onset of maternal symptoms [17]. Therefore, an elective Caesarean section should be considered. The introduction of serological assays into clinical practice will help the clinician to better assess the individual risk.
Footnotes
European Board and College of Obstetrics and Gynaecology (EBCOG): Clinical Practice Advice 
References
- 1.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol. 2020:100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu H., Wang L., Fang C., Peng S., Zhang L., Chang G. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9:51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzamora M.C., Paredes T., Caceres D., Webb C.M., Valdez L.M., La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020 doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong L., Tian J., He S., Zhu C., Wang J., Liu C. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020 doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simonsen K.A., Anderson-Berry A.L., Delair S.F., Davies H.D. Early-onset neonatal Sepsis. Clin Microbiol Rev. 2014;27:21–47. doi: 10.1128/CMR.00031-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chatzistamatiou K., Sotiriadis A., Agorastos T. Effect of mode of delivery on vertical human papillomavirus transmission - a meta-analysis. J Obstet Gynaecol. 2016;36:10–14. doi: 10.3109/01443615.2015.1030606. [DOI] [PubMed] [Google Scholar]
- 10.Qiu L., Liu X., Xiao M., Xie J., Cao W., Liu Z. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis n.d. 2020 doi: 10.1093/cid/ciaa375. https://doi.org/10.1093/cid/ciaa375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carosso A., Cosma S., Borella F., Marozio L., Coscia A., Ghisetti V. Pre-labor anorectal swab for SARS-CoV-2 in COVID-19 patients: is it time to think about it? Eur J Obstet Gynecol Reprod Biol. 2020 doi: 10.1016/j.ejogrb.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Favre G., Pomar L., Qi X., Nielsen-Saines K., Musso D., Baud D. Guidelines for pregnant women with suspected SARS-CoV-2 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Royal College of Obstetricians & Gynaecologists; 2020. Coronavirus (COVID-19) infection and pregnancy. n.d. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/ (Accessed April 10, 2020) [Google Scholar]
- 14.Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop Med Int Health. 2020;25:278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong S.H., Lui R.N., Sung J.J. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020 doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J., Wang S., Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol. 2020 doi: 10.1002/jmv.25742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.KK-W To, OT-Y Tsang, Leung W.-S., Tam A.R., Wu T.-C., Lung D.C. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng H., Xu C., Fan J., Tang Y., Deng Q., Zhang W. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020 doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reveiz L., Gaitán H.G., Cuervo L.G. Enemas during labour. Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD000330.pub4. CD000330. [DOI] [PubMed] [Google Scholar]
- 20.Guidance | NICE; 2020. Recommendations | Intrapartum care for healthy women and babies. n.d. https://www.nice.org.uk/guidance/cg190/chapter/recommendations#first-stage-of-labour (Accessed April 11, 2020) [Google Scholar]
- 21.Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30003-3. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Magoga G., Saccone G., Al-Kouatly H.B., Dahlen G.H., Thornton C., Akbarzadeh M. Warm perineal compresses during the second stage of labor for reducing perineal trauma: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2019;240:93–98. doi: 10.1016/j.ejogrb.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 23.Jiang H., Qian X., Carroli G., Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017;2 doi: 10.1002/14651858.CD000081.pub3. CD000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chi Wai T., Cecilia C.W., Anny T.W.M., Hau Yee L. Incidence and risk factors of obstetric anal sphincter injuries after various modes of vaginal deliveries in chinese women. Chin Med J (Engl) 2015;128:2420–2425. doi: 10.4103/0366-6999.164874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lund N.S., Persson L.K.G., Jangö H., Gommesen D., Westergaard H.B. Episiotomy in vacuum-assisted delivery affects the risk of obstetric anal sphincter injury: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016;207:193–199. doi: 10.1016/j.ejogrb.2016.10.013. [DOI] [PubMed] [Google Scholar]