In late 2019 a novel human coronavirus, now named severe acute respiratory syndrome coronavirus 2 emerged in Wuhan, China. In early February, first cases were registered in Italy and in the last week sharply increased. From March 1 to 11 the Italian government issued a series of social distancing measures.
Here we describe changes in access to coronary care unit (CCU) for acute coronary syndrome (ACS) following COVID-19 spread in 10 cardiological centers of the Veneto Region, in northern Italy, members of the Padua School of Cardiology Network (PSCN)*.
A specific changepoint in ACS admission to CCU has been identified using a Bayesian approach, where the longitudinal sequence of CCU admissions changed speed as compared to what was to be expected. This level shift day of the time series was identified through a Bayesian Changepoint Detection Method.1
The posterior distribution was estimated via the Markov Chain Monte Carlo method with 500 iterations and 50 burn-in replications. Longitudinal over time behavior was modeled by a Generalized Additive Model. The 95% confidence bounds have been also estimated. All the analyses have been performed using the R-System (R Core Team, 2019).2
No extramural funding was used to support this work. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents.
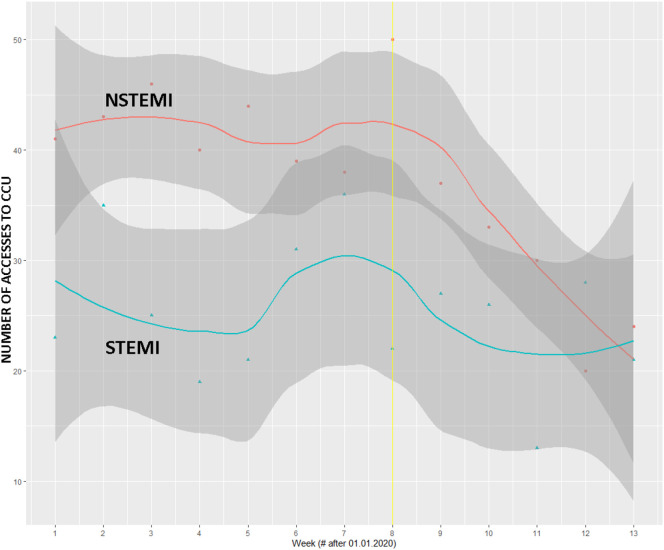
Starting from the ninth week of 2020, we observed a significant reduction in access to the CCU for non-ST segment elevation myocardial infarction (NSTEMI) (P = .0071), but not for ST segment elevation myocardial infarction (STEMI) (P = .475) (Figure 1 ).
Figure 1.
Number of NSTEMI and STEMI admitted to ICU since 01.01.2020. Points are observed data and line is a smoothed estimated of the trend over time. Grayed areas represent 95% confidence bands around the trend. Data are cases per week.
In the first 8 weeks of 2019, hospitalizations for NSTEMI were 260, and in the following 5 weeks 221 (P = .075). In the same two periods of 2019, 22 and 21 STEMI were recorded, respectively (P = .878).
Our results showed that after the eighth week of 2020 there was a significant reduction in access to CCU for NSTEMI if compared to the same period of the previous year, but not for STEMI.
It is interesting to observe that hospitalizations for NSTEMI decreased before the introduction of restrictive measures.
Our study cannot provide explanations for the results obtained, but we can draw some hypotheses.
First, since the beginning of the epidemic in Italy the population has shown to be reluctant to go to healthcare facilities, fearing to get infected. In the following days, the National Health System asked patients with urgent health problems not to go directly to emergency department, but to contact their family doctor first. This measure may have discouraged even more patients with mild symptoms to reach the hospital.
In this sense, a recent report showed a significant increase in the time from symptom onset to first medical contact for patients with chest pain and suspected myocardial infarction.3
On the other hand, since the first days of March 2020, there has been a progressive drop in NO2 concentration in northern Italy, particularly after the most restrictive measures were issued, causing a dramatic reduction in the use of motor vehicles. In previous studies, this pollutant has been associated with an increased risk of myocardial infarction.4 , 5
We speculate that the reduction of NO2 may have contributed, in part, to the reduction of less severe acute coronary syndromes, such as NSTEMI, but may not have been able to influence the development of more severe coronary thrombotic events.
The reduction of noise related to air and ground transportation could be another factor implicated in the reduction in access for NSTEMI.6
The stable number of STEMI registered during COVID-19 epidemic, could be due to the more severe clinical picture of this ACS. We consider unlikely that these patients, usually characterized by severe chest pain, would not have referred to emergency department.
Moreover, in the Veneto Region, a specific health protocol for myocardial infarction is operative, providing an accurate telephone triage for patients with chest pain and, in case of a high probability of STEMI, an ambulance is sent to home. This protocol could have favored the maintenance of normal access to the cardiological centers for patients with a more severe clinical picture.
The decrease of hospital access for patients with chest pain and NSTEMI represents a severe public health problem, reducing patients with ACS obtaining adequate care. In the future, population should receive precise information on how to access health facilities, reassuring about the presence of dedicated paths for non-COVID-19 patients inside the hospitals.
* Padua School of Cardiology Network (PSCN): Department of Cardiac, Thoracic, Vascular Sciences and Public Health, University of Padua, Padua, Italy; Department of Cardiology, Ca′ Foncello Hospital, Treviso, Italy; Department of Cardiology, Immacolata Concezione Hospital, Piove di Sacco, Italy; Department of Cardiology, Ospedali Riuniti Padova Sud, Monselice, Italy; Department of Cardiology, Rovigo General Hospital, Rovigo, Italy; Department of Cardiology, Mirano General Hospital, Mirano, Italy; Department of Cardiology, dell'Angelo Hospital, Mestre, Italy; Department of Cardiology, San Martino Hospital, Belluno, Italy; Department of Cardiology, Cittadella General Hospital, Cittadella, Italy; Camposampiero General Hospital, Camposampiero, Italy.
References
- 1.Barry D., Hartigan J.A. A Bayesian analysis for change point problems. Journal of the American Statistical Association. 1993;88(421):309–319. doi: 10.1080/01621459.1993.10594323. [DOI] [Google Scholar]
- 2.Core Team R. R: A Language and Environment for Statistical Computing. 2019. https://www.R-project.org/ R Foundation for Statistical Computing.
- 3.Tam Chor-Cheung Frankie, Cheung Kent-Shek, Lam Simon. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roswall N., Raaschou-Nielsen O., Ketzel M. Long-term residential road traffic noise and NO2 exposure in relation to risk of incident myocardial infarction - A Danish cohort study. Environ Res. 2017 Jul;156:80–86. doi: 10.1016/j.envres.2017.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Liu H., Tian Y., Xiang X. Air pollution and hospitalization for acute myocardial infarction in China. Am J Cardiol. 2017 Sep 1;120(5):753–758. doi: 10.1016/j.amjcard.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Héritier H., Vienneau D., Foraster M. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J. 2019 Feb 14;40(7):598–603. doi: 10.1093/eurheartj/ehy650. [DOI] [PubMed] [Google Scholar]