Abstract
The association between hyperparathyroidism and sarcoma is extremely rare with other reported cases describing the development of osteosarcoma and chondrosarcomas in middle-aged adults. This case describes an adolescent male with hyperparathyroidism and a pathologic fracture of a biopsy-proven brown tumor in the distal right femur. The fracture healed but later developed an undifferentiated pleomorphic sarcoma of the bone at the site of the known brown tumor. Although in vitro and in vivo studies have demonstrated the risks of elevated parathyroid hormone with development of sarcomas, there is limited evidence of a human association. The effects of elevated parathyroid hormone on the skeletally immature bone in the setting of sarcoma formation are currently not well understood without current description of adolescent hyperparathyroidism-associated sarcomas. This case highlights a sarcoma originating at a pathologically proven brown tumor within an adolescent male, discusses the association of sarcoma with hyperparathyroidism, and reviews the other nine reported cases in the literature.
Development of bone sarcomas in patients with hyperparathyroidism is rare, with nine other reported cases in the literature to our knowledge.1,2,3,4,5,6 Parathyroid hormone (PTH) is a primary modulator of bone remodeling in the setting of calcium homeostasis. PTH effects on modulating osteoblasts and gene expression has been shown to alter skeletal structure,7-9 and PTH analogs have been used subsequently for treatment of osteoporosis.10 It has also been suggested that PTH may stimulate abnormal osteoblastic activity, and an association between elevated PTH and risk for osteosarcoma formation has been demonstrated in several in vitro11,12 and rat studies.13 Based on these findings in rat models, there have been several human cohort studies6,14,15 evaluating whether there is a relationship between PTH and sarcomas. We present a unique case of a young man with a history of adolescent primary hyperparathyroidism and fracture through a histologically proven brown tumor with subsequent development of an undifferentiated pleomorphic sarcoma (UPS) of the bone to make clinicians aware of this rare presentation. Identifying a possible association between sarcoma development in hyperparathyroidism is important because the delayed diagnosis of both can lead to poor clinical outcomes.
Case Report
A 22-year-old man presented to our clinic for right distal femur pathologic fracture management in the setting of treated primary hyperparathyroidism. Three years before presentation, he had a right femur medial femoral condyle pathologic fracture through a lytic lesion, which was histologically diagnosed as a brown tumor (Figure 1) at an outside facility and primary hyperparathyroidism with an elevated serum calcium (16.8 units) and PTH (389 units). A bone scan revealed multiple lesions within the pelvis, skull, femora, and tibiae which were favored to represent additional brown tumors. He was managed by an endocrinologist with eventual parathyroid adenoma resection with resultant resolution of hyperparathyroidism. Two years before presentation, he was in a motor vehicle accident and fractured his right mid femoral shaft, managed with intramedullary nailing. Follow-up radiographs confirmed the distal femur pathologic fracture healed with progressive brown tumor sclerosis (Figure 2). Two months before presentation, he had a distal right femur periprosthetic fracture involving the medial femoral condyle brown tumor (Figure 3). At the time of current presentation, his hyperparathyroidism was well controlled with normal calcium and PTH levels. While awaiting surgical clearance, he had progressive right knee swelling; radiographs obtained after our initial clinic visit demonstrated destructive changes of the distal femur fracture and associated soft-tissue mass (Figure 4). CT imaging and angiography confirmed osseous destruction and soft-tissue mass displacing popliteus vasculature (Figures 5 and 6). Biopsy and histology of the lesion demonstrated a high-grade sarcoma without osteoid formation (Figure 7). Outside histology slides from the previously biopsied distal femur lytic lesion confirmed the initial distal femur brown tumor diagnosis (Figure 8). Subsequent positron emission tomography-computed tomography demonstrated no evidence for metastatic disease. An above-the-knee amputation was done (Figure 9), with histology confirming undifferentiated pleomorphic sarcoma (UPS) of the bone.
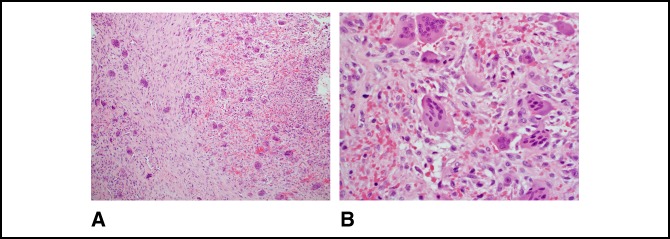
Figure 1.
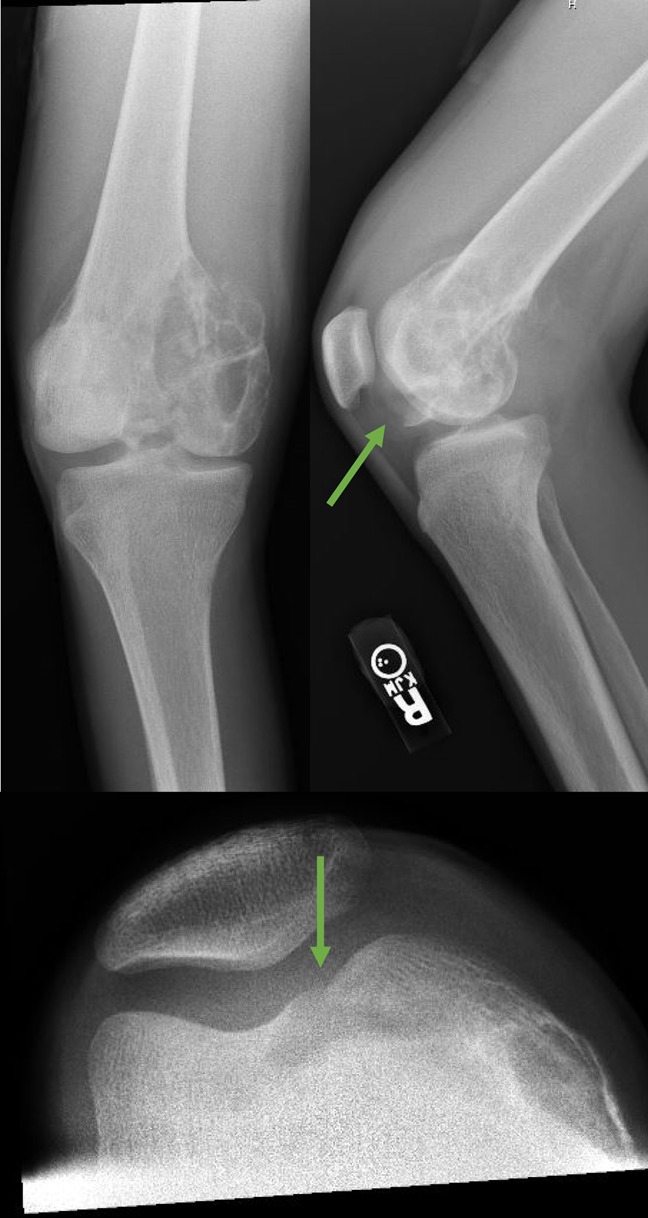
A radiograph 3 years before presentation demonstrating a lytic lesion within the right knee medial femoral condyle with associated pathologic fracture (green arrows), which was histologically proven to be a brown tumor.
Figure 2.

A radiograph 2 years before presentation showing a nailed right mid femoral shaft fracture and healed medial femoral condyle fracture with increased sclerosis of the brown tumor.
Figure 3.
A radiograph 1 month before presentation demonstrating a pathologic fracture of the distal right femur at the apex of the intramedullary nail and extending to the biopsy-proven brown tumor. Left proximal tibia lesion with features of an additional brown tumor.
Figure 4.
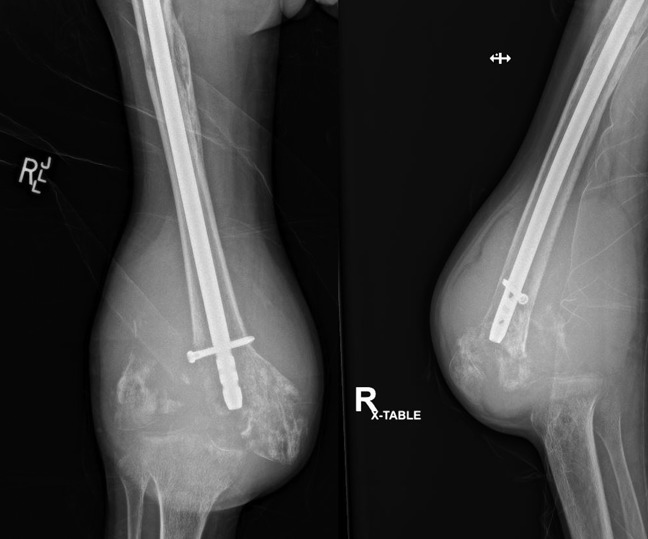
A radiograph at our initial clinical encounter demonstrating increased fracture displacement and osseous destruction of the distal right femur fracture with soft-tissue component.
Figure 5.
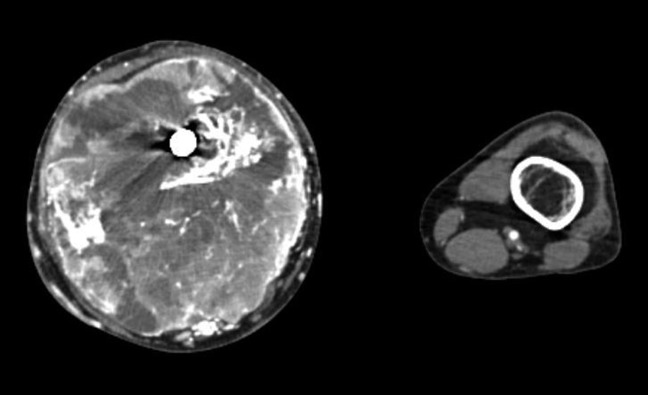
Photograph showing CT contrast-enhanced transaxial imaging demonstrating a large soft-tissue lesion with necrosis and osseous destruction of the distal femur.
Figure 6.

Angiogram of the right lower extremity showing patency of the right popliteus artery and hypervascularity of the soft-tissue lesion.
Figure 7.
A, Micrograph showing a tumor composed of a haphazard and fascicular proliferation of bland spindle cells and osteoclast-type giant cells. Giant cells have an uneven distribution and cluster around the areas of hemorrhage (100×, H&E). B, Micrograph showing spindle cells with a disorderly arrangement with extravasated red blood cells and giant cells. The nuclear features of the spindle cells and giant cells are distinct from one another and significant atypia is absent (400×, H&E).
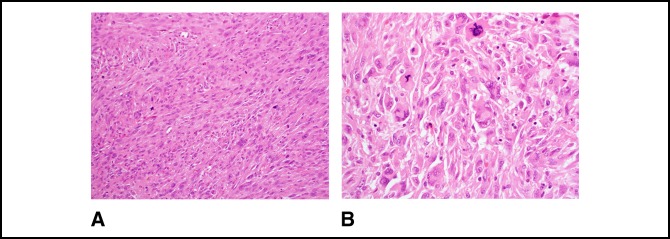
Figure 8.
A, Photograph showing microscopically markedly atypical spindle cells arranged in fascicles with brisk mitotic activity including atypical forms. Scattered tumor giant cells and epithelioid cells are also present (200×, H&E). B, Photograph showing other areas show more sheet-like growth with elongated and polygonal cells. Tumor giant cells and atypical mitotic figures are conspicuous (400×, H&E).
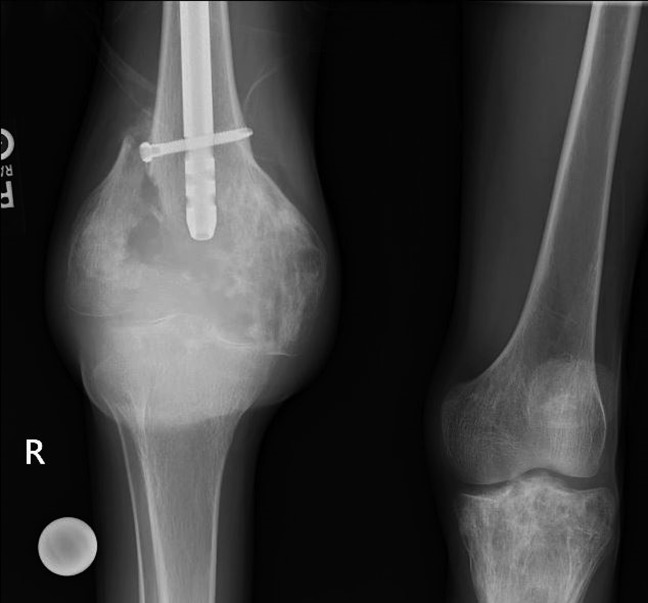
Figure 9.

Radiographs of the right femur after above-the-knee amputation.
Discussion
There has been concern for an association between PTH and osteosarcomas after in vivo and in vitro studies11-13 demonstrating a link in rat models and the current clinical use of PTH analogs as a treatment of osteoporosis. Although there have been a few case reports, a few retrospective human studies were not able to find an obvious association,6,14,15 with a need for further studies. Hyperparathyroidism in the pediatric population typically presents during adolescence, as with this case, and there appears to have higher incidence of bone involvement then adults.16 The effects of hyperparathyroidism on skeletally immature bone and development of sarcoma are not known, but an in vitro study13 suggests that exposure to PTH in younger rats may have a higher risk for sarcoma development than in rats exposed later in life. To our knowledge, there are no case reports of hyperparathyroidism associated with an UPS of the bone. Furthermore, no case has been reported of an UPS of the bone from a biopsy-proven brown tumor; however, UPS-like tumors may clearly arise in the setting of dedifferentiation or progression of other mesenchymal tumors (e.g. dedifferentiated chondrosarcoma) [17], suggesting that this patient's sarcoma may represent a very rare instance of progression of the brown tumor.
This case highlights an atypical presentation of undifferentiated pleomorphic sarcoma of the bone that developed in a young man with hyperparathyroidism at the site of a biopsy-proven brown tumor. The association of sarcomas with hyperparathyroidism is extremely rare with this representing the 10th case in the English literature to our knowledge (Table 1).1,2,3,4,5,6 Of the now 10 reported cases, the age range is 15 to 69, with only 2 cases reported in men. No correlation can be made between the time of hyperparathyroidism diagnosis, treatment, and sarcoma location. Reported sarcoma pathologies include osteosarcoma, chondrosarcoma, and this case is the first report on an UPS. From these 10 cases, only 4 have either a corresponding pathologic diagnosis of a brown tumor or osteitis fibrosa cystica; 2 cases have radiographic evidence of other skeletal brown tumors, which the authors of this study believe is also significant because this is evidence of osseous changes related to hyperparathyroidism. In the four cases without these supporting findings of bone-related hyperparathyroidism changes, it is particularly uncertain whether the two cases reported by Keen et al are truly related to hyperparathyroidism, given that the chondrosarcoma diagnoses occurred in the background of other cartilaginous neoplasm; a well-established association is known between osteochondroma and enchondroma malignant transformation into chondrosarcomas. In our case, a potential confounder is the adjacent intramedullary nail. There is a rare reported association between sarcomas and orthopaedic prostheses/implants.18-20 Various bone and soft-tissue sarcoma subtypes have been reported with orthopaedic implants of differing metallic composition.21 The histological relation between these sarcomas and implants are not well delineated but initially favored to represent a foreign-body response18 leading to a hyperimmune state.22 In the review of orthopaedic implant-related sarcomas by Keel et al,21 the time range between implant placement and sarcoma diagnosis was 2.5 to 33 years (mean 11 years) in the 12 reviewed cases; our patient's intramedullary femoral nail was placed 2 year before sarcoma diagnosis. In our case, the UPS development appears adjacent to both the nail and brown tumor near the intercondylar eminence with pathologic fracture through the lateral femoral condyle. A limitation of this case is that it is difficult to delineate where the epicenter of the sarcoma is in relation because of extensive destructive changes that occurred by the time cross-sectional imaging was done.
Table 1.
List of Other Reported Cases of Sarcomas Occurring in the Setting of Hyperparathyroidism
| Case | Patient demographics | Time between hyperparathyroidism diagnosis and sarcoma diagnosis | Treatment of hyperparathyroidism | Sarcoma pathology | Sarcoma location |
| 1 (Spiro et al) | 46-year-old woman | 3 years | Parathyroidectomy | Dedifferentiated chondrosarcomaa | Distal left tibia |
| 2 (Spiro et al) | 34-year-old woman | 2 months | Parathyroidectomy | High-grade osteosarcoma | Mandible |
| 3 (Mercuri et al) | 56-year-old woman | Simultaneous diagnosis | Parathyroidectomy | High-grade osteosarcomab | Proximal left tibia |
| 4 (Vassilopoulou et al & Gagel et al) | 69-year-old woman | Not reported | Not reported | High-grade fibroblastic osteosarcomaa | Right proximal femur |
| 5 (Harell et al) | 50-year-old woman | 3 years | Untreated | Osteosarcoma | Mandible |
| 6 (Keen et al) | 66-year-old woman | Simultaneous diagnosis | Not reported | Low-grade chondrosarcoma arising from osteochondroma | Right scapula |
| 7 (Keen et al) | 36-year-old woman | Simultaneous diagnosis | Not reported | Low-grade chondrosarcoma arising from enchondroma | Left tibia |
| 8 (Gagel et al) | 15-year-old man | Simultaneous diagnosis | Not reported | Fibroblastic osteosarcomaa | Right femur and pelvis |
| 9 (Gagel et al) | 65-year-old woman | 3 years | Not reported | Fibroblastic osteosarcomab | Distal right femur |
| 10 (our case) | 22-year-old man | 3 years | Parathyroidectomy | Undifferentiated pleomorphic sarcomaa | Distal right femur |
Brown tumor or osteitis fibrosa cystica on pathology
Brown tumors on radiographs
This case demonstrates a young man with a history of adolescent hyperparathyroidism who ultimately developed an undifferentiated pleomorphic sarcoma of the bone in the distal femur. The difficulty in the diagnosis included osseous changes of hyperparathyroidism including multiple brown tumors, metal implant, pathologic fracture, and delayed presentation. This case highlights the possible rare association of hyperparathyroidism and sarcomas and difficulty in diagnosis because of the challenging clinical scenarios. Early recognition in the subset of patients is imperative by the clinicians and radiologist to improve clinical outcomes.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Herrmann, Dr. Stanborough, Dr. Chrisinger, and Dr. Jennings.
References
- 1.Smith J, Huvos AG, Chapman M, Rabbs C, Spiro RH: Hyperparathyroidism associated with sarcoma of bone. Skeletal Radiol 1997;26:107-112. [DOI] [PubMed] [Google Scholar]
- 2.Jutte PC, Rosso R, de Paolis M, et al. : Osteosarcoma associated with hyperparathyroidism. Skeletal Radiol 2004;33:473-476. [DOI] [PubMed] [Google Scholar]
- 3.Betancourt M, Wirfel KL, Raymond AK, Yasko AW, Lee J, Vassilopoulou-Sellin R: Osteosarcoma of bone in a patient with primary hyperparathyroidism: A case report. J Bone Miner Res 2003;18:163-166. [DOI] [PubMed] [Google Scholar]
- 4.Cinamon U, Avinoach I, Harell M: Neurofibromatosis type 1, hyperparathyroidism, and osteosarcoma: Interplay? Eur Arch Otorhinolaryngol 2002;259:540-542. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia A, Cannon S, Briggs T, Keen RW: Case report: Chondrosarcoma in association with primary hyperparathyroidism. J Bone Miner Res 2004;19:1200-1203. [DOI] [PubMed] [Google Scholar]
- 6.Jimenez C, Yang Y, Kim HW, et al. : Primary hyperparathyroidism and osteosarcoma: Examination of a large cohort identifies three cases of fibroblastic osteosarcoma. J Bone Mineral Res 2005;20:1562-1568. [DOI] [PubMed] [Google Scholar]
- 7.Swarthout JT, D'Alonzo RC, Selvamurugan N, Partridge NC: Parathyroid hormone-dependent signaling pathways regulating genes in bone cells. Gene 2002;282:1-17. [DOI] [PubMed] [Google Scholar]
- 8.Okimoto N, Tsurukami H, Okazaki Y, et al. : Effects of a weekly injection of human parathyroid hormone (1-34) and withdrawal on bone mass, strength, and turnover in mature ovariectomized rats. Bone 1998;22:523-531. [DOI] [PubMed] [Google Scholar]
- 9.Sato M, Vahle J, Schmidt A, et al. : Abnormal bone architecture and biomechanical properties with near-lifetime treatment of rats with PTH. Endocrinology 2002;143:3230-3242. [DOI] [PubMed] [Google Scholar]
- 10.Seeman E, Delmas PD: Reconstructing the skeleton with intermittent parathyroid hormone. Trends Endocrinol Metab 2001;12:281-283. [DOI] [PubMed] [Google Scholar]
- 11.Bidwell J, Xu W, Onyia J, Alvarez M, Hock J, Long H: Rat osteoblast and osteosarcoma nuclear matrix proteins bind with sequence specificity to the rat type I collagen promoter 1. Endocrinology 2014;138:482-489. [DOI] [PubMed] [Google Scholar]
- 12.Onishi T, Zhang W, Cao XU, Hruska K: The mitogenic effect of parathyroid hormone is associated with E2F-dependent activation. J Bone Miner Res 1997;12:1596-1605. [DOI] [PubMed] [Google Scholar]
- 13.Vahle JL, Long GG, Sandusky G, Westmore M, ma YL, Sato M: Bone neoplasms in F344 rats given teriparatide [rhPTH(1-34)] are dependent on duration of treatment and dose. Toxicol Pathol 2004;32:426-438. [DOI] [PubMed] [Google Scholar]
- 14.Subbiah V, Madsen VS, Raymond AK, Benjamin RS, Ludwig JA: Of mice and men: Divergent risks of teriparatide-induced osteosarcoma. Osteoporos Int 2010;21:1041-1045. [DOI] [PubMed] [Google Scholar]
- 15.Cinamon U, Turcotte RE: Primary hyperparathyroidism and malignancy: “Studies by nature.” Bone 2006;39:420-423. [DOI] [PubMed] [Google Scholar]
- 16.Kollars J, Zarroug AE, van Heerden J, et al. : Primary hyperparathyroidism in pediatric patients. Pediatrics 2005;115:974-980. [DOI] [PubMed] [Google Scholar]
- 17.Matushansky I, Charytonowicz E, Mills J, Siddiqi S, Hricik T, Cordon-Cardo C: MFH classification: Differentiating undifferentiated pleomorphic sarcoma in the 21st century. Expert Rev Anticancer Ther 2009;9:1135-1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams JE, Jaffe KA, Lemons JE, Siegal GP: Prosthetic implant associated sarcomas: A case report emphasizing surface evaluation and spectroscopic trace metal analysis. Ann Diagn Pathol 2003;7:35-46. [DOI] [PubMed] [Google Scholar]
- 19.Kavalar R, Fokter SK, Lamovec J: Total hip arthroplasty-related osteogenic osteosarcoma: Case report and review of the literature. Eur J Med Res 2016;21:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richter H, Vinh TN, Mizel MS, Temple HT: Malignant fibrous histiocytoma associated with remote internal fixation of an ankle fracture. Foot Ankle Int 2006;27:375-379. [DOI] [PubMed] [Google Scholar]
- 21.Keel SB, Jaffe KA, Nielsen GP, Rosenberg AE: Orthopaedic implant-related sarcoma: A study of twelve cases. Mod Pathol 2001;14:969-977. [DOI] [PubMed] [Google Scholar]
- 22.Wooley PH, Nasser S, Fitzgerald RH: The immune response to implant materials in humans. Clin Orthop Relat Res 1996;326:63-70. [DOI] [PubMed] [Google Scholar]