Highlights
-
•
Always consider acute toxoplasmosis when a lymphoproliferative syndrome is establish in an immunocompetent patient.
-
•
Screen cardiac enzymes in every acute toxoplasmosis, even in the absence of cardiac symptoms.
-
•
Cardiac MRI, elevation of cardiac enzymes and positive IgM Toxoplasma gondii serology confirms myocarditis by such agent diagnosis.
-
•
Currently, toxoplasma encephalitis has no specific gold standard test, supporting the diagnosis on the clinical manifestations.
-
•
There is no robust evidence that supports sulfadoxine plus pyrimethamine as a superior therapy in contrast of trimethoprim/sulfamethoxazole.
Keywords: Toxoplasma gondii, Toxoplasmosis, Myopericarditis, Encephalitis
Abstract
We document a case of a 34-year-old man with no medical previous history, presenting with lymphoproliferative syndrome associated to Toxoplasma gondii infection complicated with myopericarditis and possible encephalitis, whose diagnosis was made with lymph node biopsy, cardiac imaging, serology compatible with acute toxoplasmosis and clinical response after treatment.
Introduction
Toxoplasmosis is a common zoonotic infection with high prevalence in many undeveloped countries, like Peru. The etiology, Toxoplasma gondii, is an intracellular protozoan parasite usually seeing causing cerebral abscess by reactivation in HIV infected patients with acquire immunodeficiency syndrome (AIDS) deeply immunocompromised [1].
In the immunocompetent patient, Toxoplasma gondii is frequently asymptomatic in almost 90 % of the infected persons. The remaining 10 % develops a mononucleosis like syndrome with no further complications, secondary to the primo infection with the parasite [1]. Humans get infected after consuming raw or poorly cooked meat, or after the accidental oral ingestion of the cat’s oocyst, being this last route of infection linked with more possibilities of clinical manifestations in the immunocompetent patient [2,3].
Complications such as myocarditis and encephalitis in the immunocompetent host are extremely rare, with only few reports in the current medical literature due to the absence of gold standard tests, making them entities of challenging diagnosis [4,5]. Below we present the case of a 34-year-old man from Arequipa, Peru, with the diagnosis of myocarditis and possible encephalitis secondary to Toxoplasma gondii infection.
Case presentation
A 34-year-old male, natural from Arequipa, Peru, with no previous medical conditions, presented with a seven-day history of progressive headache and photophobia, associated with fever, rash, weakness, myalgia and arthralgia. During physical examination on admission, patient showed irritability due to photophobia and high intensity headache, with 100.4 °F temperature, erythematous macular and papular lesions on thorax and extremities; enlarged, superficial and tender lymph nodes in cervical, supraclavicular, axillar and inguinal areas; and hepatomegaly. No other significant alterations were found.
Viral encephalitis was presume. Brain magnetic resonance imaging (MRI) and cerebrospinal fluid (CSF) biochemistry were normal, with negative results on bacterial, fungus and viral etiologies by direct, culture and molecular research on CSF. Leukopenia (mild lymphopenia) with 13 % atypical lymphocytes was seen in the complete blood count. In addition, elevated values of lactate dehydrogenase, T troponin, creatine kinase – MB (CK-MB), aspartate and alanine aminotransferase, fibrinogen, ferritin, erythrocyte sedimentation rate (ESR) and beta-2 microglobulin were also present.
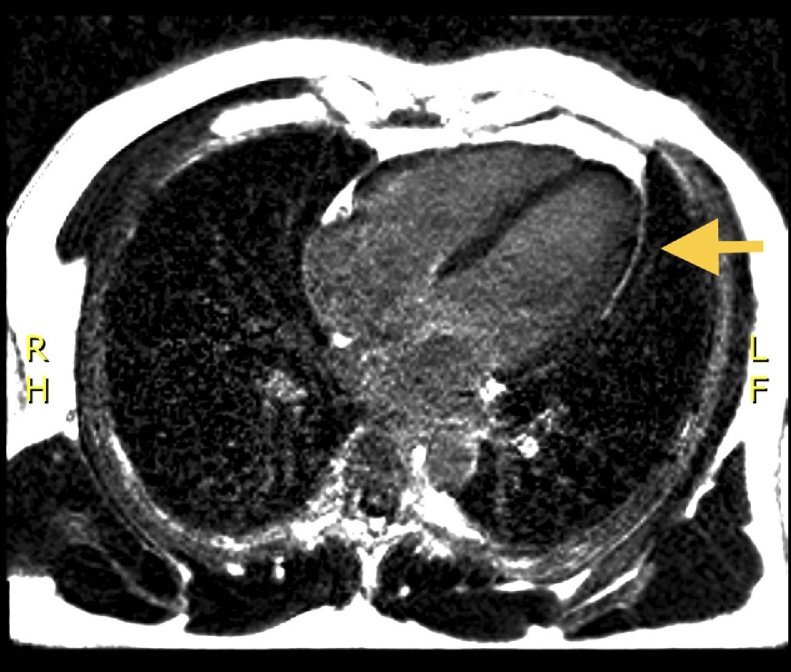
The suspicion of asymptomatic myocarditis with T troponin and CK-MB elevation was confirmed with cardiac MRI, which revealed subepicardic late enhancement and mild pericardial effusion with normal ventricular function (Fig. 1). In addition a cardiac computed tomography was perform, verifying normal coronary arteries. In the patient studied, cardiology prescribed nevibolol 2.5 mg per day. This therapy was initiated due to episodes of tachycardia unrelated to fever and chest pain that disappeared when the pulse decreased.
Fig. 1.
Cardiac MRI (T1) subepicardic enhancement during late phase of gadolinium administration in the absence of subendocardial isquemic pattern (arrow), compatible with myopericarditis.
Immunoglobulin M (IgM) and G (IgG) for Toxoplasma gondii were slightly positive and negative respectively on the first examination. Other serology studies for Epstein Barr virus (EBV), cytomegalovirus (CMV), human immunodeficiency virus (HIV), hepatitis B virus, hepatitis C virus, measles, Brucella spp and syphilis were negative. Lymph node biopsy describe reactive mixed (follicular and paracortical) lymphoid hyperplasia. Microbiology and pathology studies on lymphoid tissue ruled out neoplasm, tuberculosis, fungal or other bacterial infections.
Nevertheless, protein chain reaction in lymph node tissue was positive for Toxoplasma spp, in concordance with a progressive increase in serum IgM Toxoplasma gondii observed during internship, confirming the diagnosis of acute toxoplasmosis with asymptomatic myopericarditis and possible encephalitis (Table 1). Therefore, trimethoprim/sulfamethoxazole (cotrimoxazole) 160/800 mg (2 pills) bid orally was added to the treatment and maintained for four weeks. During ambulatory consult progressive neutropenia forced change the anti-parasitic therapy to azithromycin plus clindamycin for the next final two weeks, under the suspicious of cotrimoxazole myelotoxicity. Clinical, laboratory and MRI improvement was seeing during the ambulatory controls, with no relapse of the symptoms after more than 12 months of follow up.
Table 1.
Increased serological progression of antibodies against Toxoplasma gondii.
| First DOH | Fourth DOH | Seventh DOH | Twenty-third DOH | First MOC | |
|---|---|---|---|---|---|
| IgG T. gondii (IU/mL) | 0.00 | – | 34.00 | 309.60 | 300 |
| RR: Negative= < 4.00 | |||||
| IgM T. gondii (IU/mL) | 0.58 | 5.95 | 7.13 | 59.27 | 6.08 |
| RR: Negative= < 0.55 |
RR: Reference ranges; DOH: Day of hospitalization; MOC: Monthly outpatient control.
Discussion
In the immunocompetent, acute toxoplasmosis is usually asymptomatic [2]. Exceptionally, cardiac symptoms can be evidenced. However, the affection of this organ is usually underdiagnosed until its advanced stage of dilated heart disease, when the risk of sudden death is high [5]. The Fig. 1challenge for its diagnosis consists in avoiding histopathology due to the lethal danger involved in collecting the sample. In a few reported cases, as in this one, the diagnosis of myopericarditis was made by Toxoplasma gondii seroconversion with signs of cardiac compromise on magnetic resonance imaging, associated with progressive elevation of specific cardiac enzymes and in the absence of other causes [[2], [3], [4], [5], [6], [7], [8]]. In other cases, those affected can develop right bundle branch block [5,8]. In the approach to the patient, considering these aspects, clinicians can prevent progression towards the last stages of the disease and the consequent severe complications [[7], [8], [9]]. The rationality for nevibolol prescription in the patient, was due beta-blocker treatment with vasodilator effect by nitric oxide may have antioxidant and antifibrotic effect [10].
The estimated frequency of cerebral toxoplasmosis in the immunocompetent is extremely unusual [2]. In this patient, the diagnosis of encephalitis was difficult due to the slowly progressive clinical course, the unchanged brain structure, and the normality of CSF study including FilmArray meningitis/encephalitis (bacterial, viral and fungal) panel. The progressive and intense headache associated with limiting photophobia, without clear etiology, in the context of having detected the presence of Toxoplasma spp by molecular biology in the lymph node, is highly suggestive of encephalitis by this agent [2,4]. In the immunocompetent, this diagnosis must be suspected in the presence of evidence of neuroradiologic disorders, even in the absence of classic clinical and laboratory signs.(4)
Although, to date, there are no clinical studies that demonstrate a clear benefit, treatment for acute toxoplasma infection in the immunocompetent patient is reserved only for cases with symptomatic persistence or vital organ involvement [11]. Currently, the individual drug, or any combination, has not been determined to be superior in the treatment of toxoplasma myopericarditis [[2], [3], [4], [5], [6], [7], [8],12,13]; however, sulfadiazine-pyrimethamine (P-S) conjugation is considered the main therapy [5,7,13]. In this case, the cardiac compromise justified the start of trimethoprim/sulfamethoxazole (TMP/SMX), a controversial pharmacological combination selected due to the greater experience in its use, and the low availability of P-S in the country. When comparing TMP/SMX and P-S, Hernandez et al. [13] determined that the clinical, laboratory and radiological outcomes, as well as the adverse events rates were similar in both groups. This is consistent with the good response and evolution evidenced in the patient after 12 months of follow-up, although the need for subsequent comparative studies that evaluate new drugs with similar efficacy, low rate of adverse events and greater long-term tolerability is clear.
Author’s statement
AC, IV and VM have participated in the conception of the article and its writing. AC then collected and summarized the data. AC, IV and VM made a critical review of the article. Then, IV made the article corrections gradually. Finally, AC and VM approved the final version.
Sources of funding
No sources of funding to declare.
Declaration of Competing Interest
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
The authors declare having no conflict of interest in the publication of this case report.
References
- 1.Ramachandran R., Radhan P., Anand R., Subramanian I., Santosham R., Sai V. CNS toxoplasmosis in an immunocompetent individual. Radiol Case Rep. 2015;9(December (1)) doi: 10.2484/rcr.v9i1.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carme B., Bissuel F., Ajzenberg D., Bouyne R., Aznar C., Demar M. Severe acquired toxoplasmosis in immunocompetent adult patients in French Guiana. J Clin Microbiol. 2002;40(November (11)):4037–4044. doi: 10.1128/JCM.40.11.4037-4044.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Teutsch S.M., Juranek D.D., Sulzer A., Dubey J.P., Sikes R.K. Epidemic toxoplasmosis associated with infected cats. N Engl J Med. 1979;300(March (13)):695–699. doi: 10.1056/NEJM197903293001302. [DOI] [PubMed] [Google Scholar]
- 4.Pustorino G., Ferlazzo E., Carpentieri M.S., Cianci V., Gasparini S., Campello M. Cerebral toxoplasmosis diagnosed by brain tissue PCR analysis in an immunocompetent patient. Neurol Clin Pract. 2017;7(October (5)):436–438. doi: 10.1212/CPJ.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roubille F., Roubille C., Lattuca B., Gervasoni R., Vernhet-Kovacsik H., Leclercq F. Recent toxoplasmosis infection with acute myopericarditis and persistent troponin elevation in an immunocompetent patient. Cardiol Res. 2012;3(August (4)):189–191. doi: 10.4021/cr200w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guérot E., Assayag P., Morgant C., Hess M., Valère P.E. [Pericardial manifestations of toxoplasmosis] Arch Mal Coeur Vaiss. 1992;85(January (1)):109–111. Review. [PubMed] [Google Scholar]
- 7.Pergola G., Cascone A., Russo M. Acute pericarditis and myocarditis by Toxoplasma gondii in an immunocompetent young man: a case report. Infez Med. 2010;18(March (1)):48–52. [PubMed] [Google Scholar]
- 8.Chandenier J., Jarry G., Nassif D., Douadi Y., Paris L., Thulliez P. Congestive heart failure and myocarditis after seroconversion for toxoplasmosis in two immunocompetent patients. Eur J Clin Microbiol Infect Dis. 2000;19(5):375–379. doi: 10.1007/s100960050498. [DOI] [PubMed] [Google Scholar]
- 9.Machado S., Roubille F., Gahide G., Vernhet-Kovacsik H., Cornillet L., Cung T.T. Can troponin elevation predict worse prognosis in patients with acute pericarditis? Ann Cardiol Angeiol (Paris) 2010;59(1):1–7. doi: 10.1016/j.ancard.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Lüscher Thomas F. Novel insights in HFpEF, cardiomyopathies, and myocarditis. Eur Heart J. 2018;39(March 10):819–822. doi: 10.1093/eurheartj/ehy105. [DOI] [PubMed] [Google Scholar]
- 11.Liesenfeld O., Remington J.S. Toxoplasmosis. In: Martens M., Faro S., Soper D., editors. Infectious diseases in women. WB Saunders; Philadelphia: 2001. pp. 57–79. [Google Scholar]
- 12.Basit K.A., Nasir S., Vohra E., Shazlee M.K. Toxoplasmosis in an immunocompetent patient. Pak J Med Sci. 2018;34(6):1579–1581. doi: 10.12669/pjms.346.15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hernandez A.V., Thota P., Pellegrino D., Pasupuleti V., Benites-Zapata V.A., Deshpande A. A systematic review and meta-analysis of the relative efficacy and safety of treatment regimens for HIV-associated cerebral toxoplasmosis: is trimethoprim-sulfamethoxazole a real option? HIV Med. 2017;18(Febuary (2)):115–124. doi: 10.1111/hiv.12402. [DOI] [PubMed] [Google Scholar]