Abstract
EDTA dependent pseudothrombocytopenia (EDTA-PCTP) is a phenomenon that characterized by a spurious decrease of platelets in vitro due to the aggregation of platelets in EDTA anticoagulant blood samples. We report the first case of a transient appearance of EDTA-PCTP in a patient with 2019 novel coronavirus pneumonia (COVID-19). A 59-year-old woman was admitted to the isolated ward for severe type of 2019 novel coronavirus pneumonia. At the time of admission, her platelet count was in a normal range. Two days later, her platelet count decreased gradually without any signs or symptoms of bleeding. Since the peripheral blood smear showed a platelet aggregation, a blood sample anticoagulanted with citrate was tested and the number of platelet was normal. The phenomenon disappeared after 17 days when the patient was cured. This case emphasized the importance of peripheral blood smear and clinical manifestation, especially in the differential diagnosis of thrombocytopenia.
Keywords: 2019 novel coronavirus pneumonia, COVID-19, EDTA, pseudothrombocytopenia
Introduction
EDTA dependent pseudothrombocytopenia(EDTA-PCTP) is a phenomenon that described by a lower platelet count which do not reflect the patient’s real status because of platelets aggregation in EDTA anticoagulant blood samples. The incident of EDTA-PCTP is only approximate 0.12–0.15% in hospitalized patients [1,2], but it is not uncommon that clinicians make misdiagnosis leading to excessive examination and unnecessary treatment.
Since the outbreak of 2019 novel coronavirus pneumonia (COVID-19) in December 2019 in China, it has already spread to several countries around the world. According to the reports of China, the incident of thrombocytopenia complicated by COVID-19 is about 5%-36.2% [3–5]. In this report, we described a 59-year-old woman who was diagnosed with EDTA-PCTP complicated by COVID-19. This case was misdiagnosed as a true thrombocytopenia in vivo at first.
Case Report
A 59-year-old woman was admitted to the isolated ward with a 10-day history of fever and cough. Her nucleic acid of SARS-CoV-2 was positive by the high-throughput sequencing or real-time reverse-transcriptase polymerase-chain-reaction (RT-PCR) assay for upper respiratory throat swab specimens. Combing the Chest CT scanning and other laboratory tests, she was finally confirmed with COVID-19. At the time of admission, her platelet count was in a normal range (100–400 × 109/L). Although receiving the antiviral treatments with Lopinavir, Arbidol and Oseltamivir, the patient developed shortness of breath after 3 days of admission. The arterial blood oxygen partial pressure/oxygen concentration was 276 mmHg, and IL-6 was up to140.50 pg/ml indicating a severe type. The patient was transferred to the intensive care unit (ICU). At that time, her platelet count was still normal.
In addition to the antiviral treatment, the patient was also under an antibiotic treatment with Imipenem Cilastatin in ICU. We collected the blood samples in EDTA tubes and monitored the routine blood cell counts. Two days later, we suddenly found a low platelet count of 91 × 109/L. Her platelet count was decreasing progressively from then on. She was treated with platelet infusion twice but failed to respond. In spite of the lowest value of 17 × 109/L, the patient had no signs or symptoms of bleeding. The peripheral blood smear presented platelet aggregation. Meanwhile, the IgG/IgM antibody of SARS-CoV-2 in her serum was conformed qualitatively to be positive. We collected the blood samples with both EDTA tube and citrate tube on the same day. The number of platelet with citrate was normal (118 × 109/L), while that with EDTA was lower with 17 × 109/L. Thus, the patient was diagnosed with EDTA-PCTP. With the remission of COVID-19, the platelet count in the citrate anticoagulant samples remained normal, and the platelet count in the EDTA anticoagulant samples eventually returned to normal (Figure 1). One week after discharged, the patient was negative to the repeated result of IgG/IgM antibody of SARS-CoV-2, and her platelet count in the EDTA anticoagulant samples remained normal.
Figure 1.
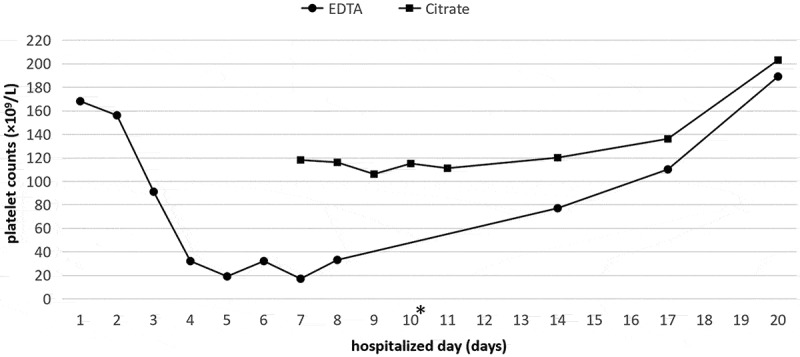
Changes of platelet counts in the patient with COVID-19 in EDTA (round) and citrate (square) blood samples. On the third hospitalized day, the patient developed a shortness of breath. On the 10th the IgG/IgM antibody of COVID-19 was conformed qualitatively to be positive. On the 14th the patient improved and left ICU. The difference of platelet count between EDTA and citrate indicated the presence of EDTA-PTCP.
Discussion
EDTA-PCTP can occur both in the normal subjects and the patients with various diseases, such as autoimmune diseases, tumor, infections and so on [6–11]. The mechanism is not completely clear, but autoimmune antibody is considered to be a key factor [12,13]. In vitro, the cryptic platelet antigen on the membrane of platelets can be exposed to the autoimmune antibody when EDTA exists. The active antigen-antibody reaction is attributed to the aggregation of platelets. What we present is the first typical case of EDTA-PCTP complicated by COVID-19. Since the patient was transferred to ICU, the medication was unchanged till the platelet count of EDTA anticoagulant returned to normal. The possible reason is that the antibody of coronavirus has the epitope binding to the cryptic platelet antigen to cause a cross-reaction of antigen-antibody. Notably, after the anti-virus treatments, the IgG/IgM antibody of SARS-CoV-2 changed from positive to negative as well as the disappearance of EDTA-PCTP. It’s proved by the return of platelet counts through the blood routine examinations of EDTA anticoagulant. Thus, it’s the evidence to support our inference. Due to the higher value of IL-6 which reflected the severity of COVID-19 [14], we speculated that inflammatory factors are essential to EDTA-PTCP.
It is not unusual to misdiagnose EDTA-PTCP as immune thrombocytopenia and disseminated intravascular coagulation, which leads to an excessive treatment[7]. In our case, unnecessary platelet transfusions were administered to the patient. Therefore, it’s important for clinicians to identify the diagnosis of EDTA-PTCP. In case of thrombocytopenia without bleeding tendency, the peripheral blood smear analysis should be applied, because it is the cheapest and the most convenient laboratory test. Furthermore, a blood sample anticoagulant with citrate is recommended to use for analysis.
Acknowledgements
We would like to acknowledge the patient in this case report. We declare that there is no conflict of interest regarding to the publication of this case report.
References
- 1.García SJ, Merino JL, Rodríguez M, Velasco A, Moreno MC.. Pseudothrombocytopenia: incidence, causes and methods of detection. Sangre (Barc) 1991;36(3):197–200. [PubMed] [Google Scholar]
- 2.Vicari A, Banfi G, Bonini PA. EDTA-dependent pseudothrombocytopaenia: a 12-month epidemiological study. Scand J Clin Lab Invest 1988;48(6):537–542. doi: 10.3109/00365518809085770 [DOI] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei-jie Guan, Zheng-yi Ni, Yu Hu, Wen-hua Liang, Chun-quan Ou, Jian-xing He, Lei Liu, Hong Shan, Chun-liang Lei, David SC Hui, et al Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv2020Feb06.20020974. [Google Scholar]
- 5.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bai M, Feng J, Liang G. Transient EDTA-dependent pseudothrombocytopenia phenomenon in a patient with antiphospholipid syndrome. Clin Lab 2018;64(9):1581–1583. doi: 10.7754/Clin.Lab.2018.180337 [DOI] [PubMed] [Google Scholar]
- 7.Berkman N, Michaeli Y, Or R, Eldor A. EDTA-dependent pseudothrombocytopenia: a clinical study of 18 patients and a review of the literature. Am J Hematol 1991;36(3):195–201. doi: 10.1002/ajh.2830360307 [DOI] [PubMed] [Google Scholar]
- 8.Wei-jie Guan, Zheng-yi Ni, Yu Hu, Wen-hua Liang, Chun-quan Ou, Jian-xing He, Lei Liu, Hong Shan, Chun-liang Lei, David SC Hui, et al Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv2020Feb06. 20020974. [Google Scholar]
- 9.Shi X, Lin Z, He L, Li W, Mo L, Li Y, Yang Z, Mo W-N Transient appearance of EDTA-dependent pseudothrombocytopenia in a postoperative patient with sepsis: A case report. Medicine (Baltimore)2017;96(11):e6330. doi: 10.1097/MD.0000000000006330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sousa SM, Sousa TM, Silva CF, Mendes CC. Pseudothrombocytopenia: a case of platelet satellitism and phagocytosis by neutrophils. Platelets 2019:1–3. doi: 10.1080/09537104.2019.1664733. [DOI] [PubMed] [Google Scholar]
- 11.Wenzel F, Lasshofer R, Rox J, Fischer J, Giers G. Transient appearance of postoperative EDTA-dependent pseudothrombocytopenia in a patient after gastrectomy. Platelets 2011;22(1):74–76. doi: 10.3109/09537104.2010.516847 [DOI] [PubMed] [Google Scholar]
- 12.Chae H, Kim M, Lim J, Oh EJ, Kim Y, Han K. Novel method to dissociate platelet clumps in EDTA-dependent pseudothrombocytopenia based on the pathophysiological mechanism. Clin Chem Lab Med 2012;50(8):1387–1391. doi: 10.1515/cclm-2011-0892 [DOI] [PubMed] [Google Scholar]
- 13.Lippi G, Plebani M. EDTA-dependent pseudothrombocytopenia: further insights and recommendations for prevention of a clinically threatening artifact. Clin Chem Lab Med 2012;50(8):1281–1285. doi: 10.1515/cclm-2012-0081 [DOI] [PubMed] [Google Scholar]
- 14.The Seventh Revised Trial Version of the Novel Coronavirus Pneumonia Diagnosis and Treatment Guidance Available at: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- The Seventh Revised Trial Version of the Novel Coronavirus Pneumonia Diagnosis and Treatment Guidance Available at: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.


