Figure 1.
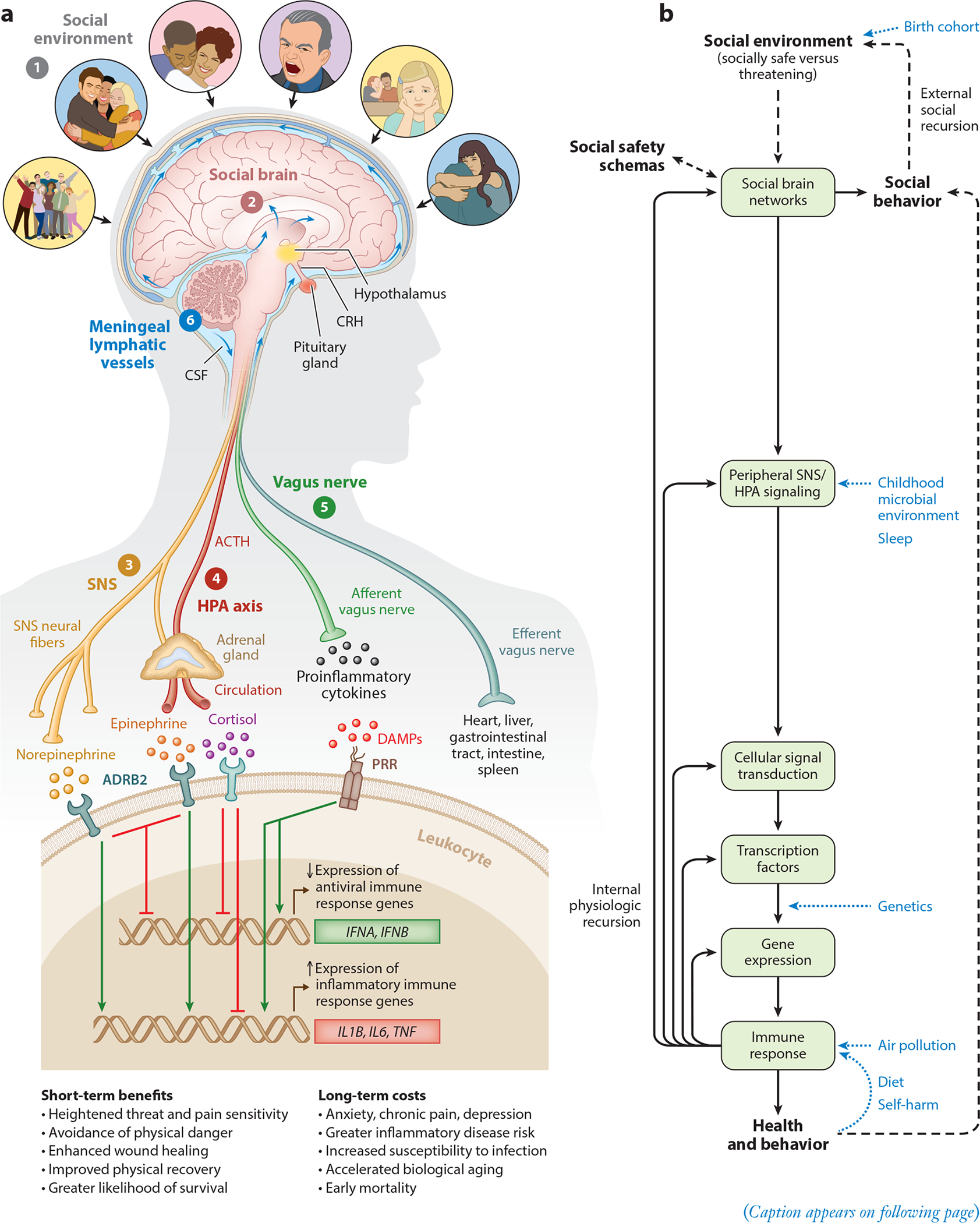
Social Safety Theory is grounded in the understanding that the primary purpose of the human brain and immune system is to keep the body biologically and physically safe. To accomplish this challenging task, humans developed a fundamental drive to create and maintain friendly social bonds and to mount anticipatory biobehavioral responses to social, physical, and microbial threats that increased risk for physical injury and infection over the course of evolution. (a) Accordingly, the brain continually monitors the (❶) social environment, interprets social signals and behaviors, and judges the extent to which its surroundings are socially safe versus threatening. These appraisals are subserved by the (❷) amygdala network, mentalizing network, empathy network, and mirror neuron system (i.e., the social brain). When a potential social threat is perceived, the brain activates a multilevel response that is mediated by several social signal transduction pathways—namely, the (❸) SNS, (❹) HPA axis, (❺) vagus nerve, and (❻) meningeal lymphatic vessels. These pathways enable the brain to communicate with the peripheral immune system and vice versa. Whereas the main end products of the SNS (i.e., epinephrine and norepinephrine) suppress transcription of antiviral type I interferon genes (e.g., IFNA, IFNB) and upregulate transcription of proinflammatory immune response genes (e.g., IL1B, IL6, TNF), the main end product of the HPA axis (i.e., cortisol) generally reduces both antiviral and inflammatory gene expression but also can lead to increased inflammatory gene expression under certain physiologic circumstances (e.g., glucocorticoid insensitivity/resistance). The vagus nerve in turn plays a putative role in suppressing inflammatory activity, whereas meningeal lymphatic vessels enable immune mediators originating in the CNS to traffic to the periphery, where they can exert systemic effects. (b) This multilevel “Biobehavioral Response to Social Threat” is critical for promoting well-being and survival. However, it can also increase risk for negative health and behavioral outcomes when it is sustained by internal physiologic or external social recursion. Several factors can also moderate these effects, including birth cohort, childhood microbial environment, sleep, genetics, air pollution, diet, and self-harm behavior. A person’s developmentally derived social safety schemas play a particularly important role in this multilevel process as they shape how social-environmental circumstances are appraised. Social safety schemas thus influence neurocognitive dynamics that initiate the full range of downstream biological interactions that ultimately structure disease risk and human behavior. Abbreviations: ACTH, adrenocorticotropin hormone; ADRB2, β2-adrenergic receptor; CNS, central nervous system; CRH, corticotropin-releasing hormone; CSF, cerebrospinal fluid; DAMPs, damage-associated molecular patterns; HPA, hypothalamic– pituitary–adrenal; PRR, pattern recognition receptor; SNS, sympathetic nervous system. Adapted with permission from Slavich & Cole (2013), SAGE Publishing; Slavich & Irwin (2014), American Psychological Association; and Slavich & Sacher (2019), Springer Nature.
