Figure 1.
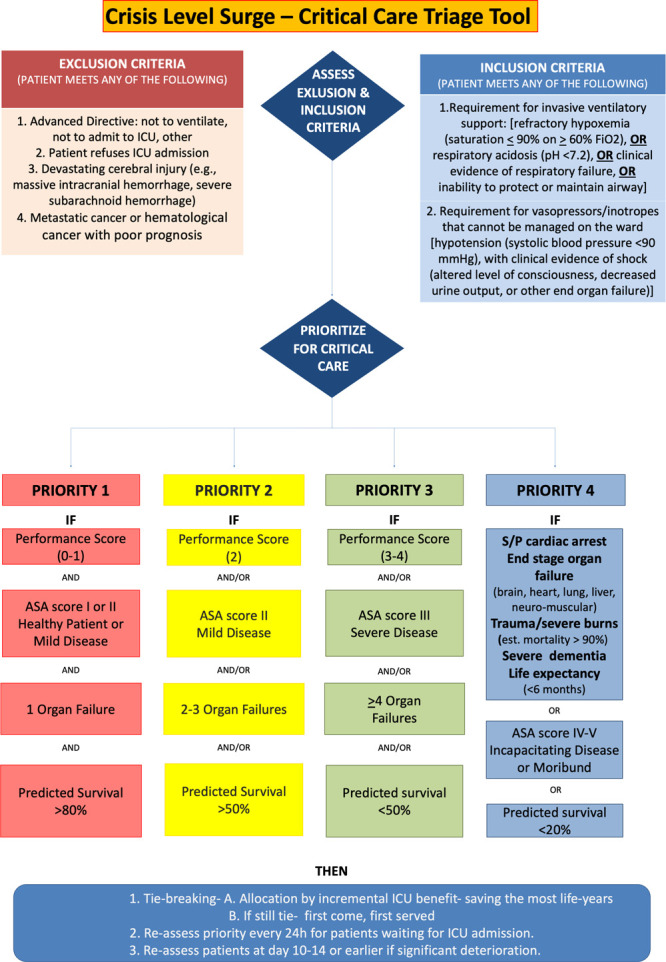
This tool provides an element of objectivity to help enhance consistency. It is not considered, however, a complete substitute for the carefully considered judgment of an experienced intensive care clinician. The presented algorithm is an example and each institution can decide on which performance score, comorbidities, and organ system failures to use based on their experience and what their staff ifs most comfortable using. A triage (prioritization) decision is a complex clinical decision made when ICU beds are limited. A structured decision-making process is important to maximize transparency and improve consistency in decision-making. A clinical estimation of likely benefit (outcomes from ICU admission compared with outcomes expected if the patient remained on the ward/other care area) is necessary so that patients who will benefit most from ICU are given priority. Examples of clinical conditions that the expert group believe would likely result in a failure of a patient to meet sufficient priority for admission is provided (priority 4). This conceptual algorithm outlines a recommended process for making an individual triage decision, based on a likelihood that survival without ICU care would be low (5–10% or less), and if admission criteria as laid out are met, survival would be estimated to be in excess of 50% short- to medium-term survival. The initial exclusion criteria are based on exclusion criteria used under “normal” conditions so that the same patients are eligible during pandemic conditions and given priority based on their likelihood to benefit. Then patients must meet one of the inclusion criteria. Priorities are then based on those to be “considered first” (priority 1 and then priority 2) and “considered last” (priority 3 and then priority 4) with priority ranking from priority 1 to 4. These exclusions should help foster trust in a fairer triage system with less chance of discrimination. Each decision is assisted on the basis of an agreed criterion thresholds for the particular ICU at a specific time and will be dependent on available resources and the number of patients queuing for admission (e.g., stricter thresholds may be required during the peak of the pandemic, and less strict thresholds at the beginning and toward the end). The performance scores, comorbidities, and organ system failure variables chosen for this example are those that are the quickest to assess. Performance scores: The premorbid baseline condition can be assessed using the Eastern Cooperative Oncology Group Performance Score, the Clinical Frailty Score, the Karnofsky Performance Scale, or other functional impairment tool the user is accustomed. Comorbidities can be assessed using the ASA score, number, or severity of comorbidities. Organ system failures can be assessed using the number of organ system failures or Sequential Organ Failure Assessment. Reevaluations for admitted and refused patients should be performed ideally every 24 hr. At reassessment of patients at days 10–14 or if significant deterioration or lack of improvement in the patient’s condition occurs decreasing the patient’s predicted survival to below the current priority group receiving critical care, reallocation of ventilator/ICU bed (following review by triage committee) should be considered. Status/post (S/P) cardiac arrest refers to patients with a recent cardiac arrest or one leading to significant anoxic brain damage.
