Figure 2.
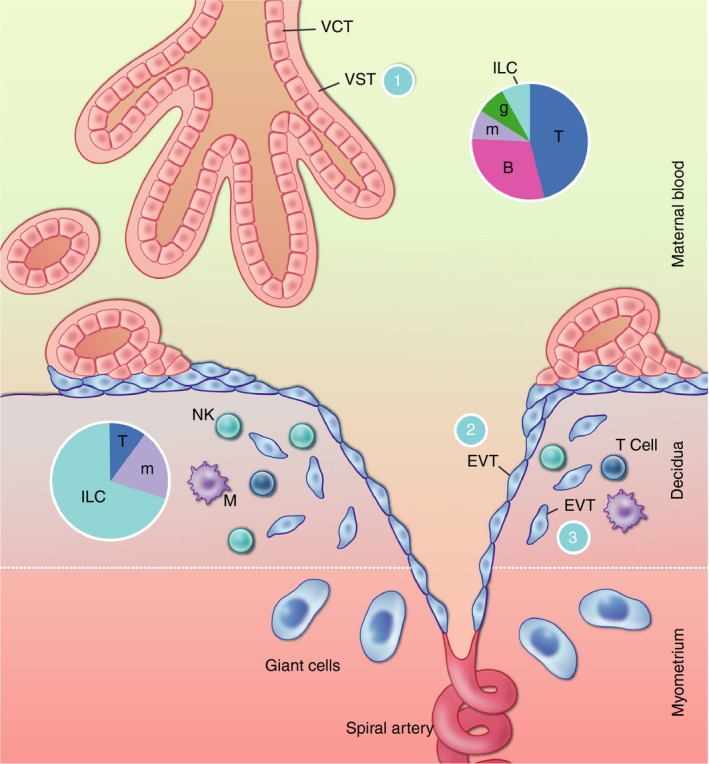
Interfaces between the placenta and the maternal immune system. The placental villi are bathed in the maternal blood. The outer layer of the villi is covered by VST with an underlying layer of mononuclear VCT. Villous trophoblast (VT) is protected from recognition by T‐cells, which are frequent in the maternal blood, by their complete lack of MHC expression (interface 1). They are further protected by immune cell recognition by their syncytial nature and thick glycocalyx. The inner layer of VCT grows out of the villi to anchor the placenta to the maternal decidua. VCT differentiates to extravillous trophoblast (EVT), some of which migrates down the spiral arteries, replacing the endothelial cells as far as the inner third of the myometrium. This process aids in the transformation of the spiral arteries, allowing blood to flow to the placenta at low pressure. These cells are in contact with the maternal blood (interface 2). Some EVT cells are also present in the decidua, where they interface with the unique immune cells present in this microenvironment (interface 3). EVT is largely protected from T‐cell recognition because they do not express the major TCR ligands HLA‐A and ‐B, but they do express the natural killer (NK) cell ligands HLA‐C, ‐E and G. At interface 2, this may protect EVT from recognition by blood NK cells. At interface 3, the expression of HLA‐C is likely to allow recognition by decidual NK cells, which are not cytotoxic but rather seem to have a role in tissue remodelling. Pie charts indicate the composition of maternal immune cells in the blood and decidua. VCT, villous cytotrophoblast; VST, villous syncytiotrophoblast; EVT, extravillous trophoblast; T, T‐cells; B, B‐cells; m, monocytes/macrophages; g, granulocytes; ILC, innate lymphoid cells.
