Abstract
Background
Increasingly, neonatal mortality is concentrated in settings of conflict and political instability. To promote evidence-based practices, an interagency collaboration developed the Newborn Health in Humanitarian Settings: Field Guide. The essential newborn care component of the Field Guide was operationalized with the use of an intervention package encompassing the training of health workers, newborn kit provisions and the installation of a newborn register.
Methods
We conducted a quasi-experimental prepost study to test the effectiveness of the intervention package on the composite outcome of essential newborn care from August 2016 to December 2018 in Bossaso, Somalia. Data from the observation of essential newborn care practices, evaluation of providers’ knowledge and skills, postnatal interviews, and qualitative information were analyzed. Differences in two-proportion z-tests were used to estimate change in essential newborn care practices. A generalized estimating equation was applied to account for clustering of practice at the health facility level.
Results
Among the 690 pregnant women in labor who sought care at the health facilities, 89.9% (n = 620) were eligible for inclusion, 84.7% (n = 525) were enrolled, and newborn outcomes were ascertained in 79.8% (n = 419). Providers’ knowledge improved from pre to posttraining, with a mean difference in score of + 11.9% (95% CI: 7.2, 16.6, p-value < 0.001) and from posttraining to 18-months after training with a mean difference of + 10.9% (95% CI: 4.7, 17.0, p-value < 0.001). The proportion of newborns who received two or more essential newborn care practices (skin-to-skin contact, early breastfeeding, and dry cord care) improved from 19.9% (95% CI: 4.9, 39.7) to 94.7% (95% CI: 87.7, 100.0). In the adjusted model that accounted for clustering at health facilities, the odds of receiving two or more essential newborn practices was 64.5 (95% CI: 15.8, 262.6, p-value < 0.001) postintervention compared to preintervention. Predischarge education offered to mothers on breastfeeding 16.5% (95% CI: 11.8, 21.1) vs 44.2% (95% CI: 38.2, 50.3) and newborn illness danger signs 9.1% (95% CI: 5.4, 12.7) vs 5.0% (95% CI: 2.4, 7.7) remained suboptimal.
Conclusions
The intervention package was feasible and effective in improving essential newborn care. Knowledge and skills gained after training were mostly retained at the 18-month follow-up.
Keywords: Essential newborn care, Humanitarian emergencies, Conflict, Clinical training, Somalia
Background
Increasingly, neonatal mortality and stillbirth are concentrated in settings of conflict and political instability [1]. Four of the five countries with the highest neonatal mortality rates in the world are in a state of chronic conflict or political instability: Somalia, South Sudan, Afghanistan and Pakistan [2]. Despite this burden, insufficient information is available on effective newborn health implementation approaches in humanitarian emergencies [3]. While there are global strategies and guidelines on newborn health for resource-poor and high mortality settings, strategies on how to scale-up evidence-based newborn interventions in the context of conflict and humanitarian emergency are lacking [3]. To promote evidence-based practices and provide guidance on neonatal care in humanitarian emergencies, an interagency working group developed the Newborn Health in Humanitarian Settings: Field Guide (Field Guide) [4]. The Field Guide, rooted in evidence-based practices recommended by the World Health Organization (WHO), comprises lists of interventions, neonatal medical supplies and drugs, and monitoring approaches at the community, primary health care, and hospital levels. In this study, we applied the essential newborn care included in the primary health facilities section of the Field Guide.
Much of the effect of conflict and disaster is experienced by communities that reside outside formal camps where access to quality health services is limited [3, 5]. In settings such as Somalia, childbirth often occurs at home or at the lowest level of the health system [6]. As neonatal mortality risk peaks at birth and during the first 24 h of life [7], it is critical to test the feasibility and to generate an evidence base for how and what can be implemented at the primary level by mid-level health workers (nurses and midwives) close to the community to improve newborn survival. Earlier studies in developing countries have shown that introducing a tailored package of essential newborn care practices might reduce stillbirth and newborn mortality [8, 9]. WHO defines essential newborn care (ENC) as a set of interventions and practices provided at childbirth and immediately after birth that includes thermal care, hygienic practices during childbirth, early breastfeeding, and newborn resuscitation [10]. As these essential newborn care practices need to be provided during labor, birth and immediately after birth, it is critical that health workers who are responsible for service provision in the labor/maternity unit have the knowledge and skills and the medical supplies necessary to provide safe and timely care.
There are two commonly used training curricula designed to build the knowledge and skills of health workers in essential newborn care: the WHO’s Essential Newborn Care Course and the American Academy of Pediatrics (AAP) Helping Babies Survive (HBS) program [11, 12]. The WHO and AAP training courses have varied levels of depth, duration, and capacity building approaches. While trainings based on the WHO and AAP training curricula have shown improvement in providers’ knowledge and skills immediately after training, their effects on changes in clinical practice, newborn mortality and stillbirth are inconsistent [13–16]. We applied the AAP HBS curriculum, since it contained substantive practical sessions for improving the skills of providers, and we supplemented the curriculum with intrapartum and maternal modules as recommended by the Field Guide.
We conducted the essential newborn care feasibility and effectiveness study in Somalia, a country that has experienced more than three decades of armed conflict [17]. At the national level, health indicators in Somalia are poor, with a maternal mortality ratio of 829 per 100,000 live births in 2017, and an estimated neonatal mortality rate of 38 deaths per 1000 live births in 2018 [2, 18]. The main causes of neonatal death in 2015 were birth asphyxia and trauma, 38.6%; prematurity, 21.1%; and infections, 28.3% [19]. The 2011 Multi Indicator Cluster Survey (MICS) in Puntland, the autonomous region of Somalia where this study was conducted, showed low antenatal coverage at 27%, low institutional delivery at 13%, and low early initiation of breastfeeding at 56% [6].
We performed a prepost intervention study to determine whether the essential newborn care practices recommended in the Field Guide were feasible to implement at the primary facility level and to measure the effect of the intervention package on increasing the correct and timely use of essential newborn care practices including: (1) thermal care, (2) breastfeeding, (3) hygienic childbirth practices, and (4) newborn resuscitation. The intervention package comprised training of health workers, provision of newborn medical supplies and drugs, and installing of newborn data collection systems. We hypothesized that the intervention package would improve essential newborn care practices by 15% from an estimated baseline (preintervention) prevalence of 30%.
Methods
Study design and timeline
This quasi-experimental prepost intervention study was conducted in Bossaso, Somalia from August 2016 through December 2018. Mixed data collection procedures included health worker knowledge and skills evaluations; observations of essential newborn care practices during labor, birth, and immediately after birth; postnatal interviews of mothers at home or via phone on the 7th -9th day after birth; and in-depth interviews and focus group discussions with health workers.
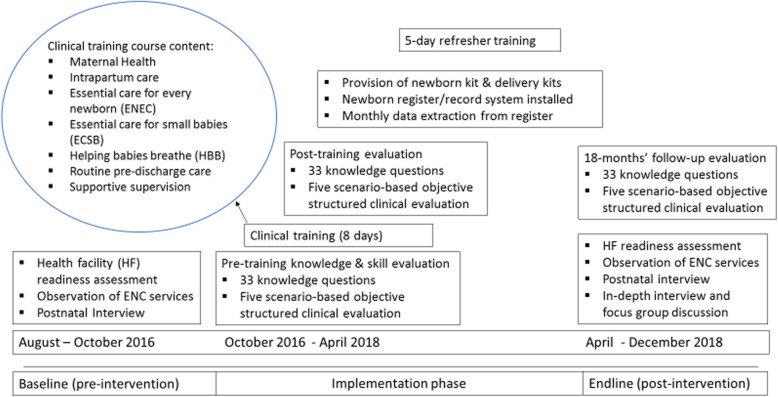
Preintervention baseline measurements were recorded from August to October 2016. An intervention package consisting of the clinical training for health workers, provision of newborn medical kits, and installation of a newborn health record system was implemented from October 2016 to April 2018. The postintervention endline measurements were taken from April to December 2018 (Fig. 1).
Fig. 1.
Schematic overview of essential newborn care Package implementation
Study settings & study participants
In Somalia, the health system has four levels: hospitals, referral health centers, health centers, and health posts [20]. Health centers are also known as maternal and child health centers. In Bossaso city, six health centers and one public hospital provide maternal and child services to internally displaced persons (IDPs) and to the host community. In consultation with the Ministry of Health, we selected four of the six health centers serving IDPs based on predefined selection criteria: the health facilities were open 24 h a day, 7 days a week and had an average of at least 40 deliveries per month. The total catchment population of the four health facilities was estimated at 134,735 persons, including both the IDPs and the host community.
Pregnant women 15–49 years of age who sought childbirth care at one of the study facilities during the study period were eligible and approached for consent and enrollment in the study. Women who were immediately referred to a hospital prior to childbirth were excluded. Women who had a stillbirth or early newborn death defined as death from 0 to 7 days of life were excluded from the postnatal interview out of respect for the family. Health workers who were responsible for service provision in the labor/maternity unit and the in-charges at the four health facilities were approached for consent and included in the study.
Implementation of newborn intervention package
The successful translation of the Field Guide to Practice necessitates the training of health workers in essential newborn care practices, the provision of newborn medical supplies and drugs, and the installation of data collection systems. The curriculum for the training of health workers was based on the AAP HBS program and comprised the Helping Babies Breathe (HBB), Essential Care for Every Baby (ECEB), and Essential Care for Small Babies (ECSB) [12]. Supplemental modules on maternal health, intrapartum care, identification and management of maternal complications, and supportive supervision were also included in the 8-day course. The training was taught by two experienced clinicians from Kenya with expertise in the subject area and experience as educators. The 8-day essential newborn care course was taught through various teaching methods: didactic lectures, videos developed for educational purposes, small group discussions, and skills practice with NeoNatalie, MamaBreast simulator, and a partograph [21–24]. Skills practices were performed in pairs and covered the assessment of a newborn, immediate newborn care, newborn resuscitation, and completion of a partograph on simulated case stories. The trainees were midwives, registered nurses, and in-charges at the four health centers. A 5-day refresher training was conducted 6 months after the initial course focusing on review of the topics covered during the initial training. Knowledge and skills evaluations were conducted pretraining, immediately after training (posttraining), and at an 18-month follow-up.
Twelve health workers (three per health center) were trained, representing 43–46% of all registered nurses and midwives in the four health facilities. Overall, there were 26 registered nurses or midwives working at the four health facilities at baseline, and 28 registered nurses or midwives at endline. We were unable to train all the health workers due to funding limitations and the requirement for some providers to remain on duty.
Newborn kits and delivery kits containing the medical supplies and drugs recommended by the Field Guide for the primary health facility level were distributed to the four health centers. The kits included the supplies and medicines necessary to monitor labor, attend childbirth, perform newborn examinations, perform newborn resuscitation, provide routine predischarge care, antibiotics, and medications for maternal health (Supplement 1: List of medical supplies and drugs).
As the existing labor and delivery registers lacked key information on the newborns, a supplemental newborn register was installed. The newborn register included information on gestational age, date and time of birth, birth weight, and any newborn complications observed (Supplement 2: Newborn register book). The newborn register was created in English and translated into Somali. The Somali version of the register was printed and distributed to the health facilities; health workers were trained and received orientation on how to complete the register book and extract data monthly.
Study outcomes and data collection
The primary outcome was a composite indicator of the essential newborn care practices and services provided to newborns at birth and immediately after birth and was measured via direct observation of clinical practices using an observation checklist. The observation checklist was adapted from the WHO’s Managing Complications in Pregnancy and Childbirth Guide [25], which has been validated in African and conflict settings [26, 27]. The observers were female from the community and with a health background (midwifery and nursing students). All observers received didactic and video-based simulation training that demonstrated the recommended essential newborn care practices. The observation tool was piloted for 2 days during the preintervention baseline assessment by pairing observers. Interobserver agreement was 94.6%.1 The primary outcome, essential newborn care, was defined as the proportion of newborns that were observed to receive at least two essential newborn care interventions. Additional variables measured were care received during pregnancy (history), predischarge education given to the mother, and maternal and newborn outcomes. Postnatal interviews with mothers were conducted either by phone or in person on the 7th to 9th day after birth. The postnatal interviews captured the status of the newborn, the mother’s knowledge of danger signs and newborn care practices, and the mother’s level of satisfaction with the care received at the health facility.
Scores of the health worker knowledge test and skills evaluation were collected for all training participants. Twelve health workers participated in the training and were evaluated at pretraining, posttraining, and at the 18-month follow-up. The knowledge and skill evaluation tools, the multiple-choice questionnaire (MCQ) and scenario-based Objective Structured Clinical Examinations (OSCE), were adapted from the AAP course. The lifesaving skills emergency obstetric training case studies on partograph use were applied to evaluate skills in the accurate completion and use of the partograph [24].
Qualitative assessment was performed at the endline. Three Focus Group Discussions (FGDs) were held with 30 health workers at the four health centers (one with providers who received the training, two with providers who had not), and in-depth interviews (IDIs) were conducted with four in-charges. The qualitative assessment aimed to examine whether and how the 8-day course and refresher training were shared among health workers who had not participated in the training; to gather information from those who attended the training on what had changed in their clinical practice after course completion; to gain insight into the perspectives of the health workers (trained and untrained) on the utility of the newborn commodities and medical supplies; and to collect their feedback on the installed newborn record/register system. The FGDs and IDIs were either conducted in English with a Somali interpreter or in Somali and audio recorded then translated and transcribed into English.
Sample size
We assumed a baseline prevalence of the provision of essential newborn care of 30%, a power of 80%, a 5% probability of a Type I error, and a nonresponse rate of 20%. To detect an absolute difference in the primary outcome, provision of essential newborn care, of at least 15%, the number of mother-newborn pairs needed was 203 at both pre and postintervention. The sample size for each facility was allocated using a proportional to estimated size where the size measure was based on historic data on number of childbirths per health facility [28].
Statistical analysis
Descriptive statistics were used to summarize the data. Proportions with 95% CI, mean (standard deviation), and median (interquartile range) were generated to characterize the study population. Missing and “don’t know” responses were analyzed as missing and excluded from the analysis. To estimate the effect of the training on the trainees’ knowledge and skills, paired Student’s t-tests were used. Differences in two proportion z-tests were used to test for differences in proportions in maternal and newborn characteristics and essential newborn care practices pre and postintervention. To accommodate for possible correlations of changes in score with health facility, i.e., single level of clustering at the health facility level, we ran a generalized estimating equation (GEE) with robust option. The GEE utilized health facility as the cluster, the indicators of interest as an outcome, and the preintervention versus postintervention indicator as predictor to estimate the adjusted odds ratio, F-statistic and p-value. We applied logistic regression to estimate the risk ratio, an approximation of the odds ratio for rare events, of early neonatal mortality and stillbirth. Statistical significance was considered at a p-value < 0.05. STATA (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP) was used for the quantitative analysis. For the qualitative analysis, audio recordings from the IDIs and FGDs were transcribed into English and imported into MAXQDA Analytics Pro (VERBI Software, 2017) for coding and analysis. Researchers engaged in content analysis applying an initial coding list based on the interview and focus group discussion guides. New codes were added as they emerged during the analysis. Once the coding framework was finalized, a subset of transcripts was coded by a primary and a secondary analyst to determine the intercoder reliability. The themes that emerged were consolidated into four subthemes.
Ethical compliance
Approval for the study was sought from the Puntland Ministry of Health, Save the Children and the Centers for Disease Control and Prevention (CDC). Approval was obtained from the Puntland Ministry of Health, the Save the Children ethics review committee, and a nonresearch determination approved by the CDC. Consent information was read to the women in the local language, and verbal consent was sought at each point of contact. Those who consented were included in the study. Personal identifiers collected to facilitate postnatal follow-up visits were destroyed immediately after completion of the data collection process. Verbal consent was obtained from health workers and the in-charges who were responsible for service provision at the four health facilities.
Results
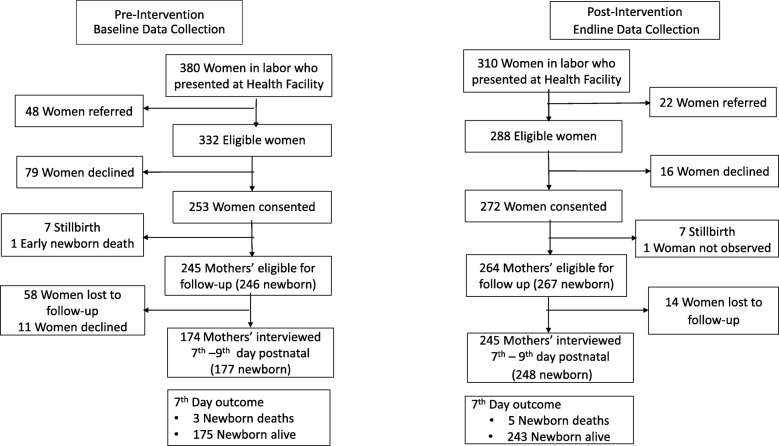
Overall, 690 pregnant women in labor sought care at the four health centers; 89.9% (n = 620) were eligible, 84.7% (n = 525) consented and were enrolled in the study, and outcomes were ascertained in a postnatal follow-up assessment in 79.8% (n = 419) of enrolled women (Fig. 2).
Fig. 2.
Study flow chart
On average, there were 1 to 2 births per day per health facility, and the highest proportion of births occurring at health center 2 at both baseline and endline. Birth attendants at the health facilities were either community midwives, auxiliary nurses, registered nurses or midwives. A minimum of three registered nurses and three midwives were available per facility at baseline; no registered nurses and 3 midwives were available at endline. At study baseline and endline, the proportion of births attended by a midwife was 90.5% [95% CI: 86.2, 93.8] and 89.3% [95% CI: 85.0, 92.7], respectively. The pre and postintervention obstetric history of the women who presented in labor with regard to median maternal age [interquartile range] (25 yrs. [21, 29] vs 26 yrs. [22, 29]), primigravida (19.8% [95% CI: 15.0, 25.2] vs 14.4% [95% CI: 10.4, 19.1]), and at least one antenatal care visit (85.3% [95% CI: 75.3, 95.7] vs 88.2% [95% CI: 78.3, 98.4]) were comparable (Table 1). The proportion of newborns born preterm were comparable at pre and postintervention. There was variation in the proportion of newborns born with low birth weight with an increase at postintervention measurement (2.5% [95% CI: 0.7, 5.3] vs 7.9% [95% CI: 4.2, 10.7]) (Table 2).
Table 1.
Health facility and study participant characteristics
| Pre-intervention | Post-intervention | P-value | |||||
|---|---|---|---|---|---|---|---|
| n/N | % | 95% CI | n/N | % | 95% CI | ||
| Facility characteristics | |||||||
| Maternity/labor room functional 24/7 | 4/4 | 100 | 4/4 | 100 | - | - | |
| Electricity functional | 3/4 | 75 | 2/4 | 50 | 0.57 | ||
| Water availability | 4/4 | 100 | 3/4 | 75 | 0.29 | ||
| Health worker | |||||||
| Mean skilled birth attendants per facility (registered nurse) | 3.8 |
Range (3–6) |
2.8 |
Range (0–4) |
|||
| Mean skilled birth attendants per facility (midwife) | 3.5 |
Range (3–4) |
3.5 |
Range (3–5) |
|||
| Location of birth | |||||||
| Health center 1 | 55/253 | 21.7 | 16.8–27.3 | 75/271 | 27.7 | 22.4–33.4 | 0.44 |
| Health center 2 | 95/253 | 37.5 | 31.6–43.8 | 93/271 | 34.3 | 28.7–40.3 | 0.64 |
| Health center 3 | 58/253 | 22.9 | 17.9–28.6 | 60/271 | 22.1 | 17.3–27.5 | 0.92 |
| Health center 4 | 45/253 | 17.8 | 13.3–23.1 | 43/271 | 15.9 | 11.7–20.8 | 0.81 |
| Length of stay from birth to discharge at HF among livebirths | |||||||
| ≤ 6:00 h | 161/242 | 66.5 | 60.6–72.4 | 174/257 | 67.7 | 62.0–73.4 | – |
| 6:00–12:00 h | 61/242 | 25.2 | 19.7–30.7 | 67/257 | 26.1 | 20.7–31.5 | – |
| ≥ 12:01 h | 20/242 | 8.3 | 4.8–11.7 | 16/257 | 6.2 | 3.3–9.2 | – |
| Birth attendant | |||||||
| Midwife | 229/253 | 90.5 | 86.2–93.8 | 242/271 | 89.3 | 85.0–92.7 | 0.66 |
| Registered nurse | 13/253 | 5.1 | 2.8–8.6 | 3/271 | 1.1 | 0.2–3.2 | 0.58 |
| Auxiliary nurse | 9/253 | 3.6 | 1.6–6.6 | 23/271 | 8.5 | 5.4–12.5 | 0.62 |
| Community midwife | 2/253 | 0.8 | 0.1–2.8 | 3/271 | 1.1 | 0.2–3.2 | 0.97 |
| Maternal age | |||||||
| 15–18 years | 23/253 | 9.1 | 5.9–13.3 | 16/271 | 5.9 | 3.4–9.4 | 0.20 |
| 19–24 years | 78/253 | 30.8 | 25.2–36.9 | 88/271 | 32.5 | 26.9–38.4 | 0.77 |
| ≥ 25 years | 152/253 | 60.1 | 53.8–66.2 | 167/271 | 61.6 | 55.5–67.4 | 0.86 |
| Gravidity | |||||||
| Primigravida | 50/253 | 19.8 | 15.0–25.2 | 39/271 | 14.4 | 10.4–19.1 | 0.17 |
| Two or more pregnancies | 203/253 | 80.2 | 74.8–85.0 | 232/271 | 85.6 | 80.9–89.6 | 0.62 |
| Antenatal care during this pregnancy | |||||||
| None | 31/253 | 12.2 | 8.5–16.9 | 32/271 | 11.8 | 8.2–16.2 | 0.96 |
| One to three ANC visits | 181/253 | 71.5 | 65.5–77.0 | 196/271 | 72.3 | 66.6–77.6 | 0.87 |
| Four or more ANC visits | 35/253 | 13.8 | 9.8–18.7 | 43/271 | 15.9 | 11.7–20.8 | 0.80 |
| Missing values | 6/253 | – | 0/271 | – | – | ||
Table 2.
Maternal and newborn birth outcomes and complications
| Variable | Pre-intervention | Post-intervention | P-value | ||||
|---|---|---|---|---|---|---|---|
| n/N | % | 95% CI | n/N | % | 95% CI | ||
| Birth and newborn outcome | |||||||
| Live birth (Singleton) | 245/253 | 96.8 | 93.9–98.6 | 261/271 | 96.3 | 93.3–98.2 | 0.96 |
| Live birth (Twins) | 1 /253 | 0.4 | 0.01–2.2 | 3 /271 | 1.1 | 0.2–3.2 | 0.34 |
| Estimated gestational age | |||||||
| < 37 Weeks | 6/247 | 2.4 | 0.9–5.1 | 4/267 | 1.5 | 0.4–3.7 | 0.45 |
| ≥ 37 Weeks | 240/247 | 97.2 | 94.4–98.9 | 263/267 | 98.5 | 96.3–99.6 | 0.91 |
| Missing values | 1/247 | – | – | – | |||
| Birthweight | |||||||
| < 2500 g | 6/247 | 2.5 | 0.7–5.3 | 21/267 | 7.9 | 4.2–10.7 | 0.002 |
| ≥ 2500 g | 216/247 | 87.4 | 94.7–99.3 | 245/267 | 91.8 | 89.3–95.8 | 0.71 |
| Missing values | 25/247 | 10.1 | 6.7–14.6 | 1 | 0.4 | 0.0–2.1 | < 0.001 |
| Newborn complications | |||||||
| Severe infection | 5 /247 | 2.0 | 0.7–4.7 | 7 /267 | 2.6 | 1.1–5.3 | 0.66 |
| Isolated fast breathing | 4 /247 | 1.6 | 0.4–4.1 | 1 /267 | 0.4 | 0.0–2.1 | 0.15 |
| Birth asphyxia | 11 /247 | 4.5 | 2.2–7.8 | 13 /267 | 4.9 | 2.6–8.2 | 0.83 |
| Congenital abnormality | 0 /247 | 0.0 | 1 /267 | 0.4 | 0.0–2.1 | 0.34 | |
| Other | 2 /247 | 0.8 | 0.1–2.9 | 1 /267 | 0.4 | 0.0–2.1 | 0.52 |
| Maternal complicationsa | |||||||
| Bleeding | 16 /253 | 6.3 | 3.7–10.1 | 7 /271 | 2.6 | 1.0–5.2 | 0.05 |
| Obstructed/prolonged labor | 17 /253 | 6.7 | 4.0–10.5 | 3 /271 | 1.1 | 0.2–3.2 | 0.001 |
| Pre-eclampsia/eclampsia | 4 /253 | 1.6 | 0.4–4.0 | 0 /271 | 0.0 | 0.04 | |
| Severe infection | 12 /253 | 4.7 | 2.5–8.1 | 12/271 | 4.4 | 2.3–7.6 | 0.87 |
| Other | 3 /253 | 1.2 | 0.2–3.4 | 0 /271 | 0.0 | 0.07 | |
azero maternal death was reported at pre- and post-intervention measurement
Health worker knowledge and skills
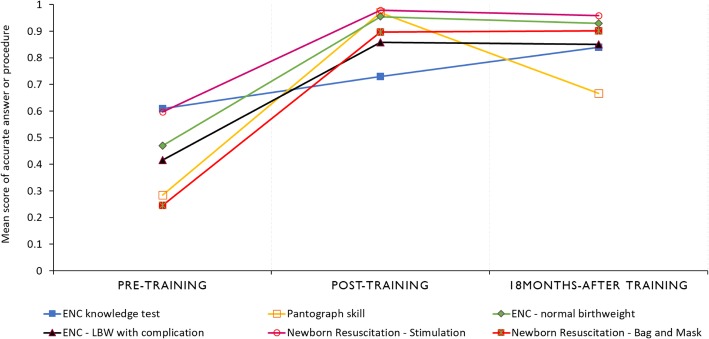
All 12 registered nurses and midwives who attended the training completed the multiple-choice knowledge test questionnaire and the scenario-based objective structured clinical skill evaluation at three time points. Their knowledge scores improved from pre to posttraining and at the 18-month follow-up. The mean difference in score from posttraining to pretraining was + 11.9% [95% CI: 7.2, 16.6; p-value < 0.001] and from 18-months after training to posttraining was + 10.9% [95% CI: 4.7, 17.0; p-value < 0.001] (Fig. 3). The score on the accurate completion of a partograph at baseline was 28.5% (95% CI: 11.7, 45.3), which improved at posttraining with a mean difference in score of + 68.5% (95% CI: 52.7, 84.3; p-value < 0.001) and declined at the 18 month follow-up from posttraining with a mean difference in score of − 30.3% (95% CI: − 13.5, − 47.1; p-value = 0.002). Skills in newborn resuscitation with bag and mask improved from pretraining to posttraining with a mean difference in score of + 65.1% (95% CI: 53.4, 76.7; p-value < 0.001), and the skill was retained at the 18-month follow-up from the posttraining score with a mean score difference of + 0.4 (95% CI: − 6.6, 7.4; p-value = 0.903) (Fig. 3).
Fig. 3.
Mean score of knowledge and skills evaluation: answers and procedures performed accurately by health providers. ENC knowledge score was based on a 33-item multiple-choice questionnaire
Essential newborn care practices
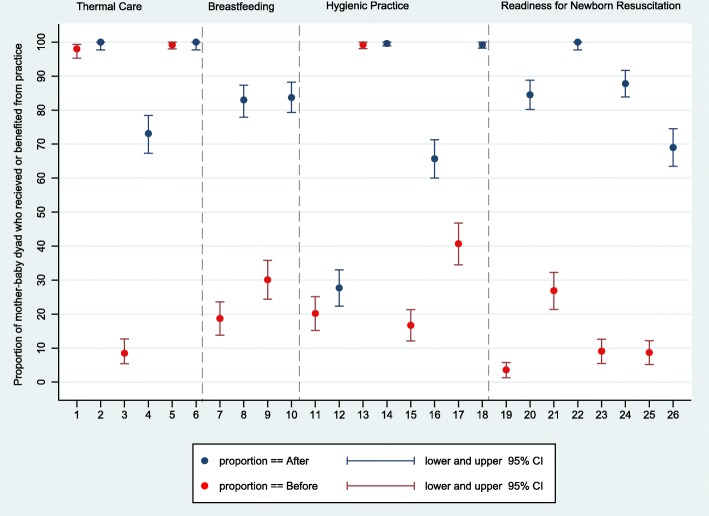
The primary composite outcome, proportion of newborns who received two or more essential newborn care practices (skin-to-skin contact, early breastfeeding, and dry cord care), improved from 19.9% (95% CI: 4.9, 39.7) at baseline to 94.7% (95% CI: 87.7, 100.0) at endline with a difference in proportion of + 74.8% (95% CI: 69.1, 80.5; p-value < 0.001). In the adjusted model, the odds of receiving two or three newborn practices at endline versus baseline was 64.5 (95% CI: 15.8, 262.6, p-value < 0.001). The proportion of newborns who received three newborn care practices improved from 0.8% (95% CI: 0.0, 1.7) at baseline to 61.4% (95% CI: 37.8, 77.0) at endline, with a difference in proportion of + 60.6% (95% CI: 54.6, 66.5; p-value < 0.001) (Table 3). All newborns who had birth asphyxia were successfully resuscitated both pre and postintervention. The difference in the proportion of newborns who received skin-to-skin contact was + 64.6% (95% CI: 58.2, 71.0, p-value < 0.001) from a baseline of 8.5% (95% CI: 5.4, 12.7) and in early breastfeeding was + 53.6% (95% CI: 46.4, 60.9, p-value< 0.001) from a baseline of 30.1% (95% CI: 24.4, 35.8) (Fig. 4).
Table 3.
Observed essential newborn care practices adjusted for health facility
| Pre-Intervention | Post-Intervention | Difference | Adjusted Odds Ratio (GEE) | p-value (GEE) | |||
|---|---|---|---|---|---|---|---|
| n/N | % (95% CI) | n/N | % (95% CI) | % (95% CI) | % (95% CI) | ||
| Early initiation of breastfeeding | 74/246 | 30.1(8.8, 61.4) | 221/264 | 83.7(59.4, 98.6) | 53.6(46.4, 60.9) | 10.6 (1.6, 69.8) | 0.014 |
| Thermal carea | 21/246 | 8.5 (0.0, 21.3) | 190/264 | 72.0 (59.4, 86.1) | 63.4 (57.0, 69.9) | 28.4 (8.0, 100.9) | < 0.001 |
| Clean childbirth practices b | 6/246 | 2.4 (0.0, 21.3) | 70/264 | 26.5 (7.9, 46.9) | 24.1 (18.4, 29.7) | 11.1 (2.6, 46.6) | 0.001 |
| Newborns received at least two ENC practices c | 49/246 | 19.9 (4.9, 39.7) | 250/264 | 94.7 (87.7, 100) | 74.8 (69.1, 80.5) | 64.5 (15.8, 262.6) | < 0.001 |
| Newborns received three ENC practices d | 2/246 | 0.8 (0.0, 1.7) | 162/264 | 61.4 (37.8, 77.0) | 60.6 (54.6, 66.5) | 220.0 (33.7, 1443.0) | < 0.001 |
| Newborn that needed resuscitation | 34/246 | 13.8 (8.3, 22.0) | 16/264 | 6.1 (4.4, 8.3) | −7.8(−13.3, −2.3) | 0.4 (0.2, 1.0) | 0.057 |
| Newborns who started breathing after stimulation | 23/23 | 100% | 0 | 0 | – | – | |
| Newborns who started breathing after bag & mask resuscitation | 11/11 | 100% | 16/16 | 100% | – | – | |
a Newborn received all three thermal care practices: immediate drying, skin-to-skin contact, delayed bathing while in the facility
b Hygienic childbirth practices all five adhered: visibly clean delivery bed, handwashing of attendant, gloves wore by attendant, use of sterile delivery kit, and dry cord care
c Newborn received two out of these three practices: skin-to-skin contact, early initiation of breastfeeding, dry cord care
d Newborn received all three practices: skin-to-skin contact, early initiation of breastfeeding, dry cord care
Fig. 4.
Observed change in essential newborn care practice readiness and care provided to mother-baby dyad. X-axis label 1,2 = immediate drying; 3,4 = skin-to-skin contact; 5,6 = delayed bathing; 7,8 = support in initiation of breastfeeding; 9,10 = early breastfeeding; 11,12 = provider washes hands with soap & water; 13,14 = provider wears new sterile gloves; 15,16 = provider uses sterile or clean delivery kits; 17,18 = dry cord care; 19,20 = printed partograph in labor room; 21,22 = functioning fetoscope in labor room; 23,24 = resuscitation surface/table in labor room; 25,26 = bag/mask in labor room
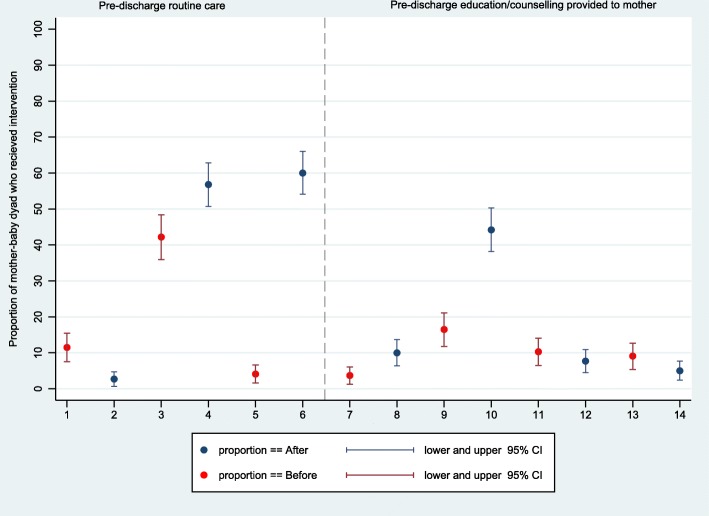
The differences in essential newborn practices was one directional (improvement) for all health facilities for most of the indicators. However, for predischarge care and education, handwashing by the attendant, and use of the sterile delivery kit, the direction of change varied by health facility. Overall, predischarge education provided to mothers related to newborn care at pre vs postintervention on the topics of skin-to-skin contact (3.7% (95% CI: 1.3, 6.1) vs 10.0% (95% CI: 6.4, 13.7)), breastfeeding (16.5% (95% CI: 11.8, 21.1) vs 44.2% (95% CI: 38.2, 50.3)), and danger signs of newborn illness (9.1% (95% CI: 5.4, 12.7) vs 5.0% (95% CI: 2.4, 7.7)) remained suboptimal (Fig. 5).
Fig. 5.
Observed change in essential newborn care practices: predischarge routine care and education provided to mother-baby dyad. X-axis label: 1,2 = examination of newborn 2 h after birth; 3,4 = eye ointment provided; 5,6 = vitamin K provided; 7,8 = education on skin-to-skin contact provided; 9,10 = education on breastfeeding provided; 11,12 = education on dry cord care provided; 13,14 = education on danger signs of newborn illness provided
This study was not powered to detect changes in mortality. From the data gathered, the proportion of stillbirth was 2.8% (95% CI: 1.1, 5.6) at baseline and 2.6% (95% CI: 1.0, 5.3) at endline, with a risk ratio of 0.9 (95% CI: 0.3, 2.6; p-value = 0.899). Early newborn mortality was 1.7% (95% CI: 0.4, 4.9) at baseline and 2.0% (95% CI: 0.7, 4.6) at endline, with a risk ratio of 1.2 (95% CI: 0.3, 4.9, p-value = 0.804).
Health workers’ perspectives on training and knowledge transfer
The themes that emerged from the FGDs and IDIs were summarized in four subthemes: knowledge and skills gained; dissemination of training; applicability of the medical supplies and kits received; and use of the newborn register. In the FGDs and IDIs, health workers reported that the training taught them new skills and improved their previously acquired skills and knowledge.
“There’s an encouragement for the staff to conduct their services. Even your mind changes – our mind has changed when we got that training and knowledge.” (In-depth interview participant)
Interventions that resulted in self-reported areas of change included Kangaroo Mother Care (KMC) and recognition of the golden minute for newborn resuscitation. Participants stated that they had been taught about the importance of skin-to-skin contact previously as an intervention for low birth weight babies, but after the study intervention period, they now used skin-to-skin contact for all babies delivered in their facilities.
Notably, changes in care resulting from the intervention were reported in the FGDs with health workers who had not attended the training as well as those who attended the training, most likely due to dissemination efforts within the facilities. All participants from the FGDs and IDIs noted that there was a diffusion of learning within their facilities following the training. Many participants shared that this diffusion of knowledge and materials was an expectation within their facilities. Information was shared through didactic presentations, dissemination of training materials, hands-on demonstrations, on-the-job training, or through a combination of these methods. In some facilities, health workers who had attended the training were paired for multiple shifts with a colleague who had not attended the training.
“You know some of our staff get trained – they share with other colleagues. That is normal.” (Focus group discussion participant)
“Every trained person was assigned to train other untrained staff during shifts, one trained and one untrained in one shift.” (Focus group discussion participant)
Participants discussed the newborn medical supplies and drugs that the health centers received as part of the study. They commented that some of the medical supplies and drugs in the kit were useful and that they would have liked to have more delivery kits, baby caps, towels, vitamin k, and antibiotics. Some supplies were not used because they either did not know how to use the medical equipment (for example, the vacuum extraction delivery kit) or the supplies were not installed (for example, the table for baby reanimation with overhead heater). The participants also discussed their preference for single use medical supplies, such as disposable newborn suction devices, as they found cleaning and sterilizing instruments challenging.
The participants discussed that the newborn register documents more information on the newborn than they had collected in the past, and since the installation of the newborn register, they have changed the way they record data. For example, newborn birth weight, previously recorded in kilograms, is now recorded in grams. The register also facilitated easier review of information. However, participants voiced challenges associated with the register, they reported that they recorded large amounts of information and that it added to their workload.
Discussion
This prepost intervention study in a humanitarian emergency demonstrates that an essential newborn care intervention package comprising health worker training, provision of newborn medical commodities, and installation of a newborn register was feasible and associated with a statistically significant improvement in observed essential newborn care practices. There was marked improvement in the proportion of newborns who received two or more essential newborn care practices. In the analysis of health worker knowledge and skills test results, the study found a statistically significant improvement in knowledge and skills immediately posttraining, and the knowledge gained was retained at the 18-month follow-up. Previous studies have shown a reduction in stillbirth after the implementation of essential newborn care training [14]. Our study was not powered to detect changes in stillbirth or early newborn mortality.
Evidence of the applicability of the AAP HBS course in humanitarian emergencies is limited [30]. Our study found that the adapted AAP HBS training curriculum was effective in increasing providers’ knowledge and skills as assessed at posttraining. Critically, our study showed that trained providers retained the knowledge gained at the 18-month follow-up, and skills such as newborn resuscitation with a bag and mask were retained. Studies in Kenya and India that evaluated the retention of knowledge after Helping Babies Breathe training found that knowledge was retained at 6-months’ follow-up; however, a decline in skills in newborn resuscitation with a bag and mask was observed at the 6-month follow-up [16]. Supportive activities, which included a refresher training at the 6th month of implementation, monitoring of the newborn register data throughout the implementation period, and training of health centers’ in-charges in supportive supervision, might have led to the knowledge and skills retention. Similar results were reported in Nepal where continued practice on manikins and coaching was associated with skill retention on newborn resuscitation at the 6-month follow-up [31].
Bundling evidence-based interventions into a service delivery model is more cost-effective than single intervention approaches [8]. In our study, the four areas of essential newborn care practices, including thermal care, early breastfeeding, hygienic birth practices, and readiness to manage birth asphyxia improved after the implementation of the intervention package, providing evidence regarding what is feasible to implement under challenging operational environments. Our study demonstrated that it is possible to train a portion of providers and have the skills transferred to untrained providers through formal and informal methods. The Lancet Neonatal Survival series recommended clinical services be universally provided by skilled health workers to every newborn around the clock [8]. Our study demonstrated that several essential newborn care practices were nearly universal for all newborns attended at endline. While there was variation in the scale of change from pre to-post-intervention, the direction of change improved for most essential newborn practices for all four health centers.
However, care practices such as attendant handwashing with soap and water, though improved from preintervention, remained suboptimal (27.7%), and the direction of change varied by health facility, with a decline in one health center at the postintervention measurement. Similarly, the use of a sterilized delivery kit at endline, though improved from preintervention, was not universal for all babies born (65.7%). Challenges in sterilization of reusable medical equipment and running out of stock of clean delivery kits might have contributed to this outcome. Previous studies on essential newborn care practices have also shown varied levels of success. In the India BetterBirth Program, adherence to hand hygiene by the birth attendant was the lowest of the practices they measured and declined at the 12 -month follow-up in the intervention arm [32].
Predischarge care, including newborn assessment at 2 h postbirth, was not common practice and did not improve. Length of stay following childbirth is a critical time to monitor for danger signs and to educate the mother/caretakers on newborn care, danger signs of newborn illness, and breastfeeding. The limited space or capacity to admit at the health facilities, the desire by families to go home, and lack of prioritization might have contributed to the short length of stay and the suboptimal predischarge care and education provided to mothers. Future trainings might benefit from sessions that focus on the health workers’ skills in educating and counseling mothers and caretakers, checklists to ensure that routine interventions are provided, and readiness for discharge assessment of newborns.
Overall, essential newborn care practices at baseline were much lower than reported in other African countries [33]. One of the consequences of protracted conflict is the limited opportunity for continued education and skill-based trainings [30, 34]. Care practices that were not targeted or emphasized by the intervention package, including quality of antenatal care, did not improve from baseline. Acquisition of essential knowledge and skills for newborn care is critical to improving the care of newborns; however, to effect change on newborn survival, capacity-building approaches in humanitarian settings need to include the pregnancy continuum, maternal care, and care for small and sick newborns. Humanitarian settings, such as Somalia, often depend on prepackaged supplies or kits in the absence of a functioning national medical supply chain system [20]. In our study, medical supplies that needed sterilization were not preferred by providers, and supplies that need installation were not installed, limiting their applicability. Future medical kit provisions should include installation or training on installation and should be appropriate for the context.
The newborn register enabled health workers to record newborn data, promoted evidence-based practices such as recording birth weight in grams, and the use of data for programming. However, careful consideration should be given to avoid overwhelming health workers with multiple record systems and reports and duplicating efforts. The results of this study suggest that the Field Guide recommended essential newborn care practices, newborn kits, and the data system are feasible and have the potential to improve essential newborn care practices in the context of protracted humanitarian crises.
Strengths and limitations
Interrupted time-series study design is increasingly used for the evaluation of public health interventions, and it is particularly well suited to interventions introduced over a clearly defined time-period. Our study had a clearly defined time for pre and postintervention measurements, and the interventions were introduced after the preintervention measurement was completed, decreasing the likelihood that concurrent changes in practice influenced the outcome. The 18-month follow-up enabled us to assess the retention of knowledge and skills. The use of observation rather than self-reported or register-based information was a strength of this study. However, the study had several limitations. First, we were unable to quantify individual (provider) levels of change in practice. Second, our estimates had wide confidence intervals overall, reflecting the small number of clusters in the study, leading to corrections widening the confidence intervals. This wide confidence interval is much more visible in the GEE model, where there were also small numbers present in the comparison groups. Third, we were unable to train all of the health workers at the four health centers. Fourth, we lost some mothers to follow-up at the postnatal visit, which might have affected the outcome. There is also the possibility of the Hawthorne effect, where providers might have performed differently under observation than in routine practice [35]. Fifth, the study was performed at four health facilities, and the implementation package and findings of this study might not be generalizable to national or large-scale initiatives. Finally, temporal changes in context or policy during the implementation period could have influenced the results.
Conclusion
We found that the intervention package, which included training of providers, provision of newborn medical commodities, and the installation of a newborn register, was feasible and effective in improving essential newborn care practices at the primary health facility level. There were areas of essential newborn care such as handwashing and predischarge education that did not improve and that will require a different approach and/or more intensive training and supervision. Sustained knowledge and skill retention at the 18-month follow-up is a promising result for program sustainability. The results of this study could provide a foundation for policies such as the national Every Newborn Action Plan that is under development and the scale-up of essential newborn care programs in Somalia.
Supplementary information
Acknowledgements
We would like to acknowledge the Ministry of Health in Bossaso, Somalia and the in-charges of the four health facilities for providing organizational support for the study and access to the health facilities. We extend special acknowledgements to the health workers, observers, data clerks, and interviewers for the substantial amount of time they invested in the successful completion of this study. The authors would also like to thank the women who participated in the study for their invaluable support.
Ethical approval and consent to participate
The health workers and women in labor provided verbal consent for birth observation. Women who were under the age of 18 years provided consent, and their parents or husbands provided verbal consent. Women provided verbal consent for home follow-up and the postnatal interviews. The study protocol was submitted to the Ministry of Health, the Save the Children Ethics Review Committee and the CDC. Approval was obtained from the Puntland Ministry of Health and the Save the Children Ethics Review Committee, and a nonresearch determination was approved by the CDC.
Declarations
The findings and conclusions in this report are those of the authors and do not represent the official position of the Centers for Disease Control and Prevention (CDC).
Abbreviations
- CDC
U.S. Centers for Disease Control and Prevention
- IDPs
Internally Displaced Persons
- WHO
World Health Organization
Authors’ contributions
RA contributed substantially to the conception, design, analysis, interpretation of the results, and the drafting of this article. CM contributed substantially to the design, implementation, and interpretation of the results. MH and KM contributed substantially to the design, analysis, and interpretation of the results presented in this article. AC contributed to the analysis and interpretation of the results. HH, JS, BG, SA, SB, and AM contributed to the design, data collection and interpretation of the results. All of the authors have read and approved the final version of this manuscript.
Funding
Funding was provided through a cooperative agreement with the Centers for Disease Control and Prevention. CDC staff contributed to the study design, analysis and interpretation of results, and review and approval of the manuscript.
Availability of data and materials
All relevant data used and/or analyzed for the study are available in anonymized form from the corresponding author upon reasonable request.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Exact count agreement divided by total count. 3600/3807
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12887-020-02120-x.
References
- 1.Wise PH, Darmstadt GL. Confronting stillbirths and newborn deaths in areas of conflict and political instability: a neglected global imperative. Pediatr Child Health. 2015;35(3):220–226. doi: 10.1179/2046905515y.0000000027. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Children’s Fund (UNICEF), WHO, World Bank Group, United Nations. Levels & trends in child mortality: report 2019. Estimates developed by the UN interagency group for child mortality estimation. New York, USA. Accessed 8 Oct 2019.
- 3.Salama P, Spiegel P, Talley L, Waldman R. Lessons learned from complex emergencies over past decade. Lancet. 2004;364:1801–1813. doi: 10.1016/S0140-6736(04)17405-9. [DOI] [PubMed] [Google Scholar]
- 4.UNICEF. Save the Children . Newborn health in humanitarian settings: field guide interim version 2016. New York: UNICEF; 2016. [Google Scholar]
- 5.Spiegel P, Checchi F, Colombo S, Paik E. Health-care needs of people affected by conflict: future trends and changing frameworks. Lancet. 2010;375:341–345. doi: 10.1016/S0140-6736(09)61873-0. [DOI] [PubMed] [Google Scholar]
- 6.UNICEF and Ministry of Planning and International Cooperation. Northeast zone multiple indicator cluster survey 2011. Nairobi, Kenya. http://microdata.worldbank.org/index.php/catalog/2551/datafile/F24/V3110 Accessed on 24 Jan 2019.
- 7.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 8.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 9.Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics. 2005;115:519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Essential newborn care course: clinical practice book. Geneva: World Health Organization; 2010. [Google Scholar]
- 11.World Health Organization . Essential newborn care course, trainer’s guide. Geneva: World Health Organization; 2010. [Google Scholar]
- 12.American Academy of pediatrics helping babies survive program. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/helping-babies-survive/Pages/Facilitator%20Tools.aspx Accessed 28 Jun 2019.
- 13.Thukral A, Lockyer J, Bucher SL, Berkelhamer S, Bose C, Deorari A, et al. Evaluation of an educational program for essential newborn care in resource-limited settings: essential care for every baby. BMC Pediatr. 2015;15:71. doi: 10.1186/s12887-015-0382-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362(7):614–623. doi: 10.1056/NEJMsa0806033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McClure EM, Carlo WA, Wright LL, Chomba E, Uxa F, Lincetto O, Bann C. Evaluation of the educational impact of the WHO essential newborn care course in Zambia. Acta Paediatr. 2007;96(8):1135–1138. doi: 10.1111/j.1651-2227.2007.00392.x. [DOI] [PubMed] [Google Scholar]
- 16.Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping babies breathe (HBB) training: what happens to knowledge and skills over time? BMC Pregnancy Childbirth. 2016;16(1):364. doi: 10.1186/s12884-016-1141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Internal Displacement Monitoring Center (IDMC): Somalia country information http://www.internal-displacement.org/countries/somalia/ Accessed on 24 Jan 2018.
- 18.Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Accessed 8 Oct 2019.
- 19.UNICEF country profiles (2016). Maternal and newborn health disparities in Somalia https://data.unicef.org/resources/maternal-newborn-health-disparities-country-profiles/. Accessed 3 Apr 2020.
- 20.World Health Organization . Strategic review of the Somali health sector: challenges and prioritized actions. 2015. [Google Scholar]
- 21.Global Health Media Project. Global health media. https://globalhealthmedia.org/ Accessed 23 Apr 2019.
- 22.Laerdal Medical. MamaBreast. https://laerdalglobalhealth.com/products/mamabreast/ Accessed 23 Apr 2019.
- 23.Laerdal Medical. NeoNatalie. https://laerdalglobalhealth.com/products/neonatalie/ Accessed 23 Apr 2019.
- 24.van den Broek N. Life saving skills manual essential obstetrics and newborn care. 2nd edition. London: Royal College of Obstetricians and Gynecologists Press; 2007 World Health Organization. Pregnancy, Childbirth, postpartum and newborn care: a guide for essential practice. 2nd ed. Geneva: World Health Organization; 2006. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/924159084X/en/. Accessed 23 Apr 2019.
- 25.WHO. UNFPA. UNICEF . Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice (3rd edition) (PCPNC) Geneva: World Health Organization; 2015. [PubMed] [Google Scholar]
- 26.Sami S, Kerber K, Kenyi S, Amsalu R, Tomczyk B, Jackson D, et al. State of newborn care in South Sudan's displacement camps: a descriptive study of facility-based deliveries. Reprod Health. 2017;14(1):161. doi: 10.1186/s12978-017-0417-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Graft-Johnson J, Vesel L, Rosen HE, Rawlins B, Abwao S, Mazia G, et al. Cross-sectional observational assessment of quality of newborn care immediately after birth in health facilities across six sub-Saharan African countries. BMJ Open. 2017;7(3):e014680. doi: 10.1136/bmjopen-2016-014680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diggle, Liang, Zeger . Analysis of longitudinal data. Oxford: Clarendon Press; 1994. [Google Scholar]
- 29.Arlington L, Kairuki AK, Isangula KG, Meda RA, Thomas E, Temu A, et al. Implementation of “helping babies breathe”: a 3-year experience in Tanzania. Pediatrics. 2017;139(5). 10.1542/peds.2016-2132. [DOI] [PubMed]
- 30.Sami S, Kerber K, Tomczyk B, Amsalu R, Jackson D, Scudder E, Dimiti A, Meyers J, Kenneth K, Kenyi S, Kennedy CE, Ackom K, Mullany LC. “you have to take action”: changing knowledge and attitudes towards newborn care practices during crisis in South Sudan. Reprod Health Matters. 2017;25(51):124–139. doi: 10.1080/09688080.2017.1405677. [DOI] [PubMed] [Google Scholar]
- 31.Kc A, Wrammert J, Nelin V, Clark RB, Ewald U, Peterson S, Malqvist M. Evaluation of helping babies breathe quality improvement cycle (HBB-QIC) on retention of neonatal resuscitation skills six months after training in Nepal. BMC Pediatr. 2017;17(1):103. doi: 10.1186/s12887-017-0853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Semrau KEA, Hirschhorn LR, Marx Delaney M, Singh VP, Saurastri R, Sharma N, et al. Outcomes of a coaching-based WHO Safe Childbirth Checklist program in India. N Engl J Med. 2017;377(24):2313–2324. doi: 10.1056/NEJMoa1701075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amsalu R, Morris CN, Chukwumalu K, Hynes M, Janjua S, Couture A, Summers A, Cannon A, Hulland EN, Baunach S. Essential newborn care practice at four primary health facilities in conflict affected areas of Bossaso, Somalia: a cross-sectional study. Confl Heal. 2019;13:27. doi: 10.1186/s13031-019-0202-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yalahow A, Hassan M, Foster AM. Training reproductive health professionals in a postconflict environment: exploring medical, nursing, and midwifery education in Mogadishu, Somalia. Reprod Health Matters. 2017;25(51):114–123. doi: 10.1080/09688080.2017.1405676. [DOI] [PubMed] [Google Scholar]
- 35.McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data used and/or analyzed for the study are available in anonymized form from the corresponding author upon reasonable request.