Abstract
Study design:
Systematic review.
Objective:
In 1994, the Load Sharing Classification (LSC) was introduced to aid the choice of surgical treatment of thoracolumbar spine fractures. Since that time this classification system has been commonly used in the field of spine surgery. However, current literature varies regarding its use and predictive value in relation to implant failure and sagittal collapse. The objective of this study is to assess the predictive value of the LSC concerning the need for anterior stabilization to prevent sagittal collapse and posterior instrumentation failure.
Methods:
An electronic search of PubMed, Medline, Embase, and the Cochrane Library was performed. Inclusion criteria were (1) cohort or clinical trial (2) including patients with thoracolumbar burst fractures (3) whose severity of the fractured vertebrae was assessed by the LSC.
Results:
Five thousand eighty-two articles have been identified, of which 21 articles were included for this review. Twelve studies reported no correlation between the LSC and sagittal collapse or instrumentation failure in patients treated with short-segment posterior instrumentation (SSPI). Seven articles found no significant relation; 5 articles found no instrumentation failure at all. The remaining 9 articles experienced failure in patients with a high LSC or recommended a different surgical technique.
Conclusions:
Although the LSC was originally developed to predict the need for anterior stabilization in addition to SSPI, many studies show that SSPI only can be sufficient in treating thoracolumbar fractures regardless of the LSC. The LSC might have lost its value in predicting sagittal collapse and posterior instrumentation failure.
Keywords: spine fracture, Load Sharing Classification, instrumentation failure, short-segment pedicle screw instrumentation, systematic review
Introduction
The choice of treatment of spinal fractures is based on a thorough clinical workup and imaging. This enables a complete understanding of the morphology of the fracture and possible ligamentous injury, including a neurological examination to determine any possible presence of neurological deficit. In contrast to the clear diagnostic criteria, the optimal treatment of these injuries remains a subject of ongoing debate. Among the many available treatment options, the short-segment fixation through a posterior approach is the most performed surgical procedure in the treatment of thoracolumbar spine fractures.1 It offers little morbidity and has a straightforward approach. However, postoperative anterior collapse and posterior implant failure are reported by several authors.2,3 Some of these failures are thought to be caused by a lack of support from the anterior columns and could be prevented by providing additional anterior spinal support through a separate or combined intervention.4
To decide whether posterior fixation alone is sufficient or additional anterior stabilization is required, the Load Sharing Classification (LSC) can be used.5 This is a 3-factor point-value system, which grades vertebral comminution in 3 planes, from 1 to 3 (1 being mild, 3 being severe). The amount of vertebral involvement, the amount of apposition or displacement, and the amount of correction of kyphotic deformity are assessed.6 Six points or less on the LSC is considered to represent little comminution, whereas scores from 7 to 9 portray high to severe vertebral comminution.
High comminution (corresponding to an LSC of 7 points or more) might result in loss of anterior support. Less anterior support can lead to an increase in loading of the pedicle screws and therefore in a higher chance of instrumentation failure. According to the original study from 1994 by McCormack et al,5 fractures with an LSC score of 7 or more should therefore be supported with an anterior stabilization, in addition to a 4-screw short-segment posterior stabilization (one level above and one level below the fractured vertebra). Due to changes in technique and implants in the last decades, it remains unclear whether the LSC still has its value in predicting the need for anterior fixation.1
The current literature varies substantially regarding the predictive value of the LSC.7-10 Therefore, this study performs a systematic review of the literature to assess the predictive value of the LSC concerning sagittal collapse and posterior instrumentation failure with a specific interest for patients with thoracolumbar burst fractures with a high LSC score, treated with a posterior stabilization only.
Methods
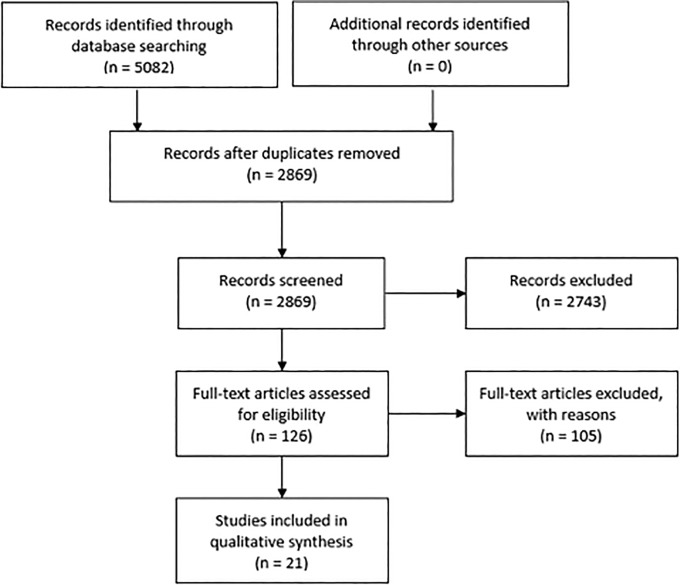
A comprehensive systematic review of the literature on the predictive value of the LSC concerning sagittal collapse and posterior instrumentation failure was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.11
Search Strategy
For this review, PubMed (from the original article of McCormack in 1994 to November 9, 2018), Medline (1994 to November 9, 2018), Embase (1994 to November 9, 2018), the Cochrane Database of Systematic Reviews (CDSR), and the Cochrane Central Register of Controlled Trials (1994 to November 9, 2018) were searched. Only articles written in the Dutch, English, and German language were reviewed. For any other language, restrictions were applied. A flow chart of the included articles is shown in Figure 1.
Figure 1.
Flowchart of selected articles according to the PRISMA statement.
Inclusion and Exclusion Criteria
The search entailed medical subject headings (Mesh terms) and also alternatives for these words. Inclusion criteria for articles were (1) cohort or clinical trial, (2) including patients with thoracolumbar burst fractures and (3) who were evaluated by the LSC for the severity of the fractured vertebrae. Exclusion criteria were fractures caused by osteoporotic or pathogenic reasons. Also, fractures in patients over 80 and under 15 years old were excluded. The search strategy can be found in Tables 1, 2, and 3.
Table 1.
Search Strategy: PubMed and Medline.
| No. | Query | Results |
|---|---|---|
| #3 | (#1 AND #2) | 2611 |
| #2 | “Classification”[Mesh] OR “classification” [Subheading] OR classif*[tiab] OR taxonom*[tiab] OR hierarch*[tiab] OR mccormack*[tiab] OR load sharing*[tiab] OR lsc[tiab] | 1 202 938 |
| #1 | “Spinal Fractures”[Mesh] OR ((“Spine”[Mesh: NoExp] OR “Lumbar Vertebrae”[Mesh] OR “Thoracic Vertebrae”[Mesh] OR spine[tiab] OR spinal*[tiab] OR lumbar vertebra*[tiab] OR thoracic vertebra*[tiab] OR thoracolumbar*[tiab]) AND (“Fractures, Bone”[Mesh: NoExp] OR “Fractures, Compression”[Mesh] OR “Fractures, Comminuted”[Mesh] OR fractur*[tiab] OR broken[tiab])) | 32 842 |
Table 2.
Search Strategy: Embase.
| No. | Query | Results |
|---|---|---|
| #4 | #3 AND ‘article’/lit | 2333 |
| #3 | #1 AND #2 | 3542 |
| #2 | ‘classification’/de OR ‘clinical classification’/exp OR ‘taxonomy’/de OR classif*: ti, ab, kw OR taxonom*: ti, ab, kw OR hierarch*: ti, ab, kw OR mccormack*: ti, ab, kw OR ‘load sharing*’: ti, ab, kw OR lsc: ti, ab, kw | 1 026 749 |
| #1 | ‘spine fracture’/exp OR ((‘lumbar spine’/exp OR ‘lumbosacral spine’/exp OR ‘thoracic spine’/exp OR ‘thoracolumbar spine’/exp OR ‘spinous process’/exp OR ‘spine’/de OR spine: ti, ab, kw OR spinal*: ti, ab, kw OR ‘lumbar vertebra*’: ti, ab, kw OR ‘thoracic vertebra*’: ti, ab, kw OR thoracolumbar*: ti, ab, kw) AND (‘fracture’/de OR ‘comminuted fracture’/exp OR ‘compression fracture’/exp OR fractur*: ti, ab, kw OR broken: ti, ab, kw)) | 52 041 |
Table 3.
Search Strategy: Wiley/Cochrane Librarya.
| No. | Query | Results |
|---|---|---|
| #3 | #1 and #2 | 138 |
| #2 | (classif* or taxonom* or hierarch* or mccormack* or “load sharing*” or lsc): ti, ab, kw | 32 365 |
| #1 | ((spine or spinal* or “lumbar vertebra*” or “thoracic vertebra*” or thoracolumbar*) and (fractur* or broken)): ti, ab, kw | 3241 |
a Results: CDSR, 2; CENTRAL, 136.
Screening
After removal of the duplicates in EndNote, 2 authors (WT, MJ) independently determined the relevance of each article to this review based on the abstracts and titles. A second selection was made based on the full text, where after the final articles were included.
Data Collection
Extracted data from the included articles was (1) the study design, (2) patients demographics, (3) received surgical method, (4) LSC scores, and (5) outcomes after follow-up, in particularly related to complications as loss of correction, instrumentation failure, and/or sagittal collapse. Furthermore, the level of evidence (Centre of Evidence Base Medicine, University of Oxford) was determined.
Results
Five thousand eighty-two articles were identified through the databases. After removal of the duplicates, 2869 articles were screened. A total of 2743 articles were excluded based on title and abstract. Of the remaining 126 articles, 105 did not meet the inclusion criteria based on the full text. The remaining 21 articles met the inclusion criteria. All 21 articles reviewed reported the surgical technique, the severity of the fracture evaluated by the LSC, and occurrence of instrumentation failure. In 12 of the 21 articles (57%), no effect of the LSC was found on the outcome. The remaining 9 studies found a relation between a high LSC and instrumentation failure or loss of correction or already chose the surgical approach based on the LSC score. A comprehensive summary of the results is presented in Table 4.
Table 4.
Summary Results of the Included Studies.
| Level of Evidence | Author (Year) | Population | Study Type | Surgical Technique | Results |
|---|---|---|---|---|---|
| 4 | Aligizakis et al (2003)29 | 30 patients, 73% male, mean age 37.2 years, 21 patients (SSPI) LSC 4/5/6, 3 patients (anterior reconstruction) LSC 7/8/9, 6 patients (SSPI + anterior strut graft) LSC 7/8/9 | Prospective cohort | 21 patients treated with SSPI, 3 patients treated via anterior, 6 patients treated with SSPI + anterior strut graft | No instrumentation failure occurred in any of the groups |
| 4 | Altay et al (2007)22 | 32 patients, 59% male, mean age 42.6 years, 19 LSC of 6, 9 LSC of 7, 4 LSC of 8. Thirty-one patients treated with LSPI. Thirteen LSC of 6, 12 LSC of 7, 6 LSC of 8 | Retrospective cohort | Group 1: SSPI (4-screw construct), group 2: LSPI (2 above and below) | Patients with LSC ≥ 7 recommended to use LSPI instead of SSPI |
| 4 | Aono et al (2016)15 | 27 patients, 70% male, mean age 43 years, 2 LSC of 5, 6 LSC of 6, 8 LSC of 7, 8 LSC of 8, 3 patients LSC of 9 | Prospective cohort | SSPI (4-screw construct) | No significant relation between LSC and failure or loss of correction |
| 4 | Avanzi et al (2010)13 | 22 patients, 59% male, mean LSC of 6.5 | Retrospective cohort | Two or 3 above and 1 or 2 below; LSPI | No relation found between implant failure and LSC |
| 4 | Chokshi et al (2019)30 | 50 patients, mean age 33.4 years. All LSC ≤7 | Prospective cohort | SSPI (6-screw construct) | One implant failure observed |
| 4 | Defino et al (2007)24 | 18 patients, 80% male, mean age 36.6 years, 2 LSC of 4, 5 LSC of 5, 2 LSC of 6, 5 LSC of 7, 2 LSC of 8, 2 LSC of 9 | Prospective cohort | SSPI (4-screw construct) | Correlation between LSC and loss of correction, although loss of correction not inherent to a high LSC |
| 2b | De Iure et al (2018)25 | 121 patients, 65% male, mean age group impending or true failure 41.5 years, mean age group without failure 51.2 years, mean LSC of 6 | Single center, retrospective cohort | SSPI (4-screw construct) (supplementary anterior fixation in case of failure), 2 above, 1 below (LSPI) | Additional anterior fixation in 34 patients due to awaiting or true instrumentation failure, 82.4% with LSC ≥ 6 points, no anterior fixation needed ≤5 points |
| 4 | Gelb et al (2010)14 | 27 patients, 85% male, mean age 34.9 years, 3 LSC of 3, 2 LSC of 4, 6 LSC of 5, 7 LSC of 6, 5 LSC of 7, 2 LSC of 8, 2 LSC of 9 | Retrospective review/cohort | SSPI (4-screw construct) | No significant difference in loss of correction between LSC ≤ 6 and LSC ≥ 7 |
| 2b | Jang et al (2018)17 | 208 patients, 50% male, mean age 45.9, mean LSC 5.7, 52 cases >7 | Retrospective cohort | SSPI: 126 patients, LSPI: 82 patients, screws at fracture level: 133 | 31 patients with re-collapse, 4 instrumentation failures, LSC: no statistically significant risk factor for re-collapse |
| 4 | Kanna et al (2015)21 | 32 patients, all LSC ≥ 7 (23 LSC of 7, 8 LSC of 8, 1 LSC of 9) | Retrospective review of case records | SSPI (6-screw construct) | No instrumentation failure observed and no anterior reconstruction needed |
| 4 | Kose et al (2014)18 | 39 patients, 67% male, mean age 35.1 years, 18 LSC of 7, 21 LSC of 6 | Retrospective cohort | SSPI (6-screw construct) | No revision needed for instrumentation failure or loss of correction |
| 4 | Liao et al (2017)26 | 56 patients, 68% male, mean age 43.4 years, 2 groups Group 1: 27 patients (2 LSC of 4, 2 LSC of 5, 12 LSC of 6, 11 LSC of 7, 1 LSC of 8) Group 2: 29 patients (2 LSC of 4, 4 LSC of 5, 7 LSC of 6, 11 LSC of 7, 3 LSC of 8, 1 LSC of 9) |
Retrospective cohort | SSPI Group 1: all pedicle screw method (6-screw construct) Group 2: Fracture augmentation (4-screw construct) |
Three out of 27 failure in group 1, all with LSC of 7 (11.1%), 8 out of 29 in group 2 (27.6%) One LSC of 6, 4 LSC of 7, 2 LSC of 8, 2 LSC of 9 Statistically significant relation between LSC and failure rate |
| 4 | Liu et al (2009)27 | 18 patients, 89% male, mean age 38.2 years, 5 LSC of 5, 4 LSC of 6, 7 LSC of 7, 2 LSC of 8 | Prospective cohort | MSPI (4-screw construct) | One patient with LSC of 8 had screw dislodgement |
| 4 | McCormack et al (1994)5 | 28 patients, 61% male, mean age 47 years; 1 LSC of 3, 2 LSC of 4, 2 LSC of 5, 4 LSC of 6, 5 LSC of 7, 7 LSC of 8, 7 LSC of 9 | Prospective cohort | SSPI (4-screw construct) | Ten of 28 patients showed screw breakage, all patients had LSC ≥ 7 points |
| 4 | Park et al (2016)23 | 45 patients, 36% male, mean age group 1: 50.5 years, mean age group 2: 49.0 years Group 1: 17 patients LSC of 7, 11 LSC of 8 Group 2: 12 patients LSC of 7, 5 LSC of 8 |
Retrospective cohort | 28 patients 2-level posterior fixation, 17 patients 3-level posterior fixation | Two cases of screw breakage, but solid union occurred. Posterior only fixation successful in patients with LSC 7 and 8 |
| 4 | Parker et al (2000)6 | 46 patients, 59% male, mean age 32.7 years, 29 SSPI, 16 via anterior, 9 LSC of 3, 5 LSC of 4, 4 LSC of 5, 6 LSC of 6, 9 LSC of 7, 7 LSC of 8, 5 LSC of 9 | Retrospective review/cohort | SSPI (4-screw construct) | 29 patients in the posterior only group, no implant failure occurred (LSC 3-6) |
| 4 | Pellisé et al (2015)16 | 72 patients, 74% male, mean age 35.6 years, mean LSC 6.3, 70.9% LSC ≥ 7 points | Single center case series | SSPI (6-screw construct) | Regional kyphosis correction loss significantly greater in LSC ≥ 7, one failure in LSC of 7 |
| 4 | Sodhi et al (2017)28 | 91 patients, 55% male, mean age 33.5 years | Retrospective cohort | SSPI (4-screw construct) | No short-segment instrumentation alone in patients with LSC ≥ 7 points preoperatively. Six out of 40 failures in LSC ≤6, 20 out of 51 failures in LSC ≥ 7 |
| 4 | Spiegl et al (2016)12 | 59 patients, 61% male, mean age 51 years, 2 LSC of 3, 11 LSC of 5, 16 LSC of 6, 22 LSC of 7, 8 LSC of 8 | Retrospective cohort | SSPI (4-screw and 6-screw construct) | No significant relation between LSC and reduction loss |
| 4 | Rojas-Tomba et al (2017)19 | 40 patients, 70% male, mean age 40.6 years, 60% LSC ≥ 7 points, 40% LSC <7 points | Retrospective review/cohort | SSPI (6-screw construct) | No implant failure with Universal Spinal System (titanium screws and rods) |
| 4 | Yang et al (2014)20 | 22 patients, 59% male, mean age 38 years, 16 patients LSC ≤ 6 points | Retrospective cohort | SSPI (6-screw), for highly comminuted 8-screw construct | No implant failure such as screw breakage |
Abbreviations: LSC, Load Sharing Classification; LSPI, long-segment posterior instrumentation; MSPI, mono-segmental posterior instrumentation; SSPI, short-segment posterior instrumentation; 4-screw construct: without intermediate screw; 6-screw construct: with intermediate screw.
No Relation Between LSC and Instrumentation Failure
Of the 12 articles that found no effect of the LSC on loss of correction or implant failure, 6 reported no significant relation between the LSC and instrumentation failure.12-17 Four did not find instrumentation failure at all.18-21 One reported no instrumentation failure but recommended to use long-segment posterior instrumentation (LSPI) instead of short-segment posterior instrumentation (SSPI) for patients with a high LSC score.22 The last one reported instrumentation failure, but stated that SSPI only can be used successful in patients with a high LSC.23 Of the 656 patients that were described in these 12 studies, 317 had a high LSC score and 317 had a low LSC score. Of the remaining patients the score was not specified. One patient in the high score group experienced instrumentation failure; none experienced failure in the low score group. This, however, was not reported in every study. Within this group, it was stated that anterior reconstruction is not necessary in most fractures and that a 2-level (6-screw construct) posterior fixation can be used successfully in patients with a high LSC score.15,16 Pellisé et al16 found a statistically significant relation between LSC scores ≥7 and loss of correction. However, no correlation was found between the LSC score and instrumentation failure. In addition to that, the loss of correction observed was not associated with significant differences in clinical outcomes and further surgery due to correction loss was not required in any case.
Relation Between LSC and Instrumentation Failure
Six studies reported a relation between a high score and instrumentation failure.5,24-28 Of the 332 patients that were described in these 6 studies, 112 had a high LSC score and 99 a low LSC score. In the remaining patients the score was not specified. Of these patients 63 in the high score group and 13 in the low score group experienced failure. This, however, was not reported in every study. Liao et al26 concluded that a high LSC causes higher failure rates. Liu et al27 used mono-segmental posterior instrumentation and conclude that an LSC of 8 correlated with a high incidence of loss of reduction or implant failure.
Use of LSC Score to Decide Surgical Technique
Two articles already based their surgical approach on the LSC score6,29 and one study only included low LSC scores in order to prevent the need for anterior reconstruction.30 Of the 126 patients described in these 3 studies, 30 had a high score and 96 a low score. One failure occurred in the group with a low score; no failure occurred in the group with a high score. Aligizakis et al29 stated that the LSC is a helpful adjunctive tool that can complement but not replace other forms of classification.
Discussion
When treating thoracolumbar fractures, there is no universal agreement on the best type of surgical treatment to achieve and maintain stabilization. The 21 studies reviewed used the classification system since the introduction of the LSC in 1994 and additionally looked at complications such as instrumentation failure. Of these 21 studies, 6 studies actually report a relation between the LSC and failure. Those 6 studies, including the study of McCormack et al,5 reported instrumentation failure in patients who had an LSC of 7 or more. The remaining 15 studies showed that there was no significant correlation between instrumentation failure and the number of points scored on the LSC. Two studies only showed an association between loss of correction and the LSC,16,24 although this did not appear to be entirely inherent to a high score.24
The classification system of McCormack et al5 has been used intensively over the past 20 years. However, their article has some limitations. In their retrospective study only 28 patients were included, treated with an older generation screws and rods. The conclusions drawn by the authors can be debated nowadays and these thoughts are not new. Several studies already reported the questionable value of the LSC regarding instability and instrumentation failure.13,21,25,31 Jang et al17 discussed that another critical limitation of the original article is that no patient-related parameters were considered. In their study, age (>43 years old) and gender were related to re-collapse and not the LSC score. Pishnamaz et al32 compared different spine fracture classification systems and concluded that other systems have a higher reliability. Therefore, the role of the LSC in clinical practice is arguable.
In the past decades, new insights and numerous improvements have modified the approach on spinal trauma care. McCormack et al5 stated that with a high LSC score anterior stabilization is necessary in order to prevent failure. However, anterior stabilization is less desirable due to the potentially increased morbidity and the desired preservation of spinal motion, especially in younger patients.19,21 Therefore, the wish to obtain sufficient stabilization via a posterior only approach is present.
Main differences seen in the reviewed articles in comparison with the article of McCormack et al5 are concerning the surgical technique. In the article of McCormack et al,5 an SSPI with 4 screws was used. Most spinal surgeons did not use this technique and are using various modifications to improve the stiffness of the posterior construct. The modifications used are extending the SSPI, using cement augmentation at fracture level or, in most cases, the use of intermediate screws at the level of the fractured vertebra. Besides the changed techniques, great improvements have been made regarding the materials used. In 1994, only stainless steel screws and rods were used. Nowadays, all constructs are made of titanium, which is said to have twice the strength and elasticity of stainless steel. Therefore, it can bear more weight and is less likely to break.15 Modern surgical techniques and more sophisticated instrumentation may have contributed to the reduction in instrumentation failure.14,19,20 Few studies were comparable to the original article of McCormack et al.5 The studies that had used the same technique either did not mention the materials used or used titanium screws and rods which makes it incomparable to the stainless steel constructs used by McCormack et al.5 Due to these improvements the LSC has not managed to maintain itself in present time. Therefore, it has lost its predictive value and thus its reliability for predicting clinical outcomes.19 Wood et al33 discussed in a comprehensive view on the management of thoracolumbar spine fracture that there still remain many uncertainties regarding the best approach to the treatment of spinal fractures. Numerous classification systems have been proposed of which the AOSpine classification, as described by Reinhold et al,34 has been used widely and is thought to be most applicable in clinical practice.32 However, further research is still necessary to asses which system or which combination of systems is best in predicting instrumentation failure and the need for anterior stabilization.
Limitations
A limitation of this review is that in case of instrumentation failure, only the number of points on the LSC was considered and no other possible contributors. McCormack et al5 reported that the stability of the vertebral body and the clinical outcome is not only dependent on the degree of comminution, but is largely determined by ligamentary damage.26,29 Because ligamentary damage plays a major role in the indication for surgery, no surgical decision can be made based on the LSC only. Other causes that contribute to instrumentation failure may, among other things, include age, gender, lifestyle, muscle strength, and previous fractures or surgery. These were not considered in this review. Another limitation is that the results of the studies reviewed may be difficult to compare due to the fact that the studies have small populations, the fracture types can be different, and a variety of techniques is used. There is a possibility that the LSC has more influence on one technique than the other. In addition, some studies showed a relation between instrumentation failure and the LSC, thus not significant. This occurred in studies with a small sample size.12,14,15,24 Due to differences in study design and various cutoff values for a high LSC score it was impossible to perform a meta-analysis.
Conclusions
Although McCormack et al5 describe that anterior stabilization in addition to SSPI is necessary in patients with a high LSC score, many studies show that SSPI only can be sufficient and safe enough in treating thoracolumbar fractures regardless of the LSC. Therefore, the LSC might be losing its predictive value concerning sagittal collapse and posterior instrumentation failure.
Acknowledgment
The authors thank Mr J. C. F. Ket from the Medical Library of the VU University of Amsterdam for performing the database searches.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Wessel T. Stam, BSc  https://orcid.org/0000-0002-2282-3783
https://orcid.org/0000-0002-2282-3783
References
- 1. Alanay A, Acaroglu E, Yazici M, Oznur A, Surat A. Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine (Phila Pa 1976). 2001;26:213–217. [DOI] [PubMed] [Google Scholar]
- 2. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993;75:162–167. [DOI] [PubMed] [Google Scholar]
- 3. Reinhold M, Knop C, Beisse R, et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J. 2010;19:1657–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang J, Liu P. Analysis of surgical approaches for unstable thoracolumbar burst fracture: minimum of five year follow-up. J Pak Med Assoc. 2015;65:201–205. [PubMed] [Google Scholar]
- 5. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741–1744. [DOI] [PubMed] [Google Scholar]
- 6. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000;25:1157–1170. [DOI] [PubMed] [Google Scholar]
- 7. Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79:69–83. [DOI] [PubMed] [Google Scholar]
- 8. Katonis PG, Kontakis GM, Loupasis GA, Aligizakis AC, Christoforakis JI, Velivassakis EG. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976). 1999;24:2352–2357. [DOI] [PubMed] [Google Scholar]
- 9. Li KC, Hsieh CH, Lee CY, Chen TH. Transpedicle body augmenter: a further step in treating burst fractures. Clin Orthop Relat Res. 2005;(436):119–125. [PubMed] [Google Scholar]
- 10. Muller U, Berlemann U, Sledge J, Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J. 1999;8:284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Spiegl UJ, Jarvers JS, Heyde CE, Glasmacher S, Von der Höh N, Josten C. Delayed indications for additive ventral treatment of thoracolumbar burst fractures: what correction loss is to be expected [in German]. Unfallchirurg. 2016;119:664–672. [DOI] [PubMed] [Google Scholar]
- 13. Avanzi O, Landim E, Meves R, Caffaro MF, de Albuquerque Araujo Luyten F, Faria AA. Thoracolumbar burst fracture: load sharing classification and posterior instrumentation failure. Rev Bras Ortop. 2010;45:236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gelb D, Ludwig S, Karp JE, et al. Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech. 2010;23:293–301. [DOI] [PubMed] [Google Scholar]
- 15. Aono H, Tobimatsu H, Ariga K, et al. Surgical outcomes of temporary short-segment instrumentation without augmentation for thoracolumbar burst fractures. Injury. 2016;47:1337–1344. [DOI] [PubMed] [Google Scholar]
- 16. Pellisé F, Barastegui D, Hernandez-Fernandez A, et al. Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures. Spine J. 2015;15:1796–1803. [DOI] [PubMed] [Google Scholar]
- 17. Jang HD, Bang C, Lee JC, et al. Risk factor analysis for predicting vertebral body re-collapse after posterior instrumented fusion in thoracolumbar burst fracture. Spine J. 2018;18:285–293. [DOI] [PubMed] [Google Scholar]
- 18. Kose KC, Inanmaz ME, Isik C, Basar H, Caliskan I, Bal E. Short segment pedicle screw instrumentation with an index level screw and cantilevered hyperlordotic reduction in the treatment of type—a fractures of the thoracolumbar spine. Bone Joint J. 2014;96-B:541–547. [DOI] [PubMed] [Google Scholar]
- 19. Rojas-Tomba F, Hernández-Ruiz Á, Menéndez-Quintanilla I, García de Quevedo-Puerta D, Moriel-Durán J, Villanueva-Pareja F. Radiologic and functional outcomes in unstable thoracolumbar fractures treated with short-segment pedicle instrumentation. Clin Spine Surg. 2017;30:459–465. [DOI] [PubMed] [Google Scholar]
- 20. Yang M, Ding GZ, Xu ZJ. Surgical outcome in thoracolumbar fractures managed by short-segment pedicle instrumentation. Ann Acad Med Singapore. 2014;43:24–32. [PubMed] [Google Scholar]
- 21. Kanna RM, Shetty AP, Rajasekaran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J. 2015;15:256–264. [DOI] [PubMed] [Google Scholar]
- 22. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in Magerl type A fractures. Eur Spine J. 2007;16:1145–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Park SR, Na HY, Kim JM, Eun DC, Son EY. More than 5-year follow-up results of two-level and three-level posterior fixations of thoracolumbar burst fractures with load-sharing scores of seven and eight points. Clin Orthop Surg. 2016;8:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Defino HL, Canto FR. Low thoracic and lumbar burst fractures: radiographic and functional outcomes. Eur Spine J. 2007;16:1934–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. De Iure F, Lofrese G, De Bonis P, Cultrera F, Cappuccio M, Battisti S. Vertebral body spread in thoracolumbar burst fractures can predict posterior construct failure. Spine J. 2018;18:1005–1013. [DOI] [PubMed] [Google Scholar]
- 26. Liao JC, Fan KF. Posterior short-segment fixation in thoracolumbar unstable burst fractures—transpedicular grafting or six-screw construct? Clin Neurol Neurosurg. 2017;153:56–63. [DOI] [PubMed] [Google Scholar]
- 27. Liu S, Li H, Liang C, et al. Monosegmental transpedicular fixation for selected patients with thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22:38–44. [DOI] [PubMed] [Google Scholar]
- 28. Sodhi HBS, Savardekar AR, Chauhan RB, Patra DP, Singla N, Salunke P. Factors predicting long-term outcome after short-segment posterior fixation for traumatic thoracolumbar fractures. Surg Neurol Int. 2017;8:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aligizakis AC, Katonis PG, Sapkas G, Papagelopoulos PJ, Galanakis I, Hadjipavlou A. Gertzbein and load sharing classifications for unstable thoracolumbar fractures. Clin Orthop Relat Res. 2003;(411):77–85. [DOI] [PubMed] [Google Scholar]
- 30. Chokshi JJ, Shah M. Outcomes of including fracture level in short-segment fixation for thoracolumbar fracture dislocation. Asian Spine J. 2019;13:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Du JP, Fan Y, Liu JJ, et al. Decompression for traumatic thoracic/thoracolumbar incomplete spinal cord injury: application of AO Spine Injury Classification System to identify the timing of operation. World Neurosurg. 2018;116:e867–e873. [DOI] [PubMed] [Google Scholar]
- 32. Pishnamaz M, Balosu S, Curfs I, et al. Reliability and agreement of different spine fracture classification systems: an independent intraobserver and interobserver study. World Neurosurg. 2018;115:e695–e702. [DOI] [PubMed] [Google Scholar]
- 33. Wood KB, Li W, Lebl DR, Ploumis A. Management of thoracolumbar spine fractures. Spine J. 2014;14:145–164. [DOI] [PubMed] [Google Scholar]
- 34. Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013;22:2184–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]