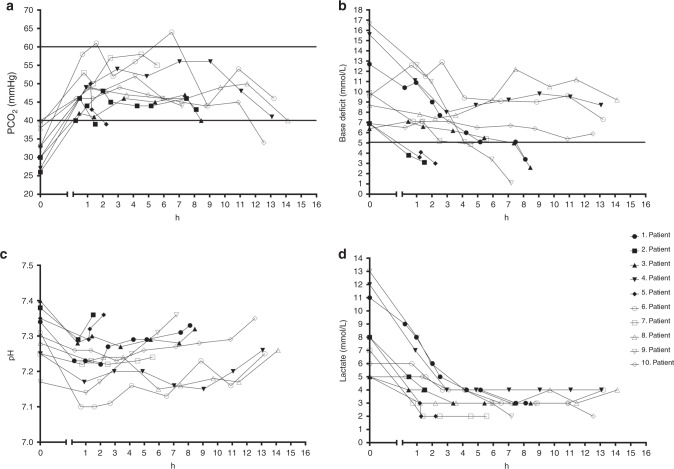
Fig. 1. The trends of temperature-corrected arterial blood gas values (PCO2, base deficit, pH) and lactate during CO2 administration.
Each symbol represents one patient. Baseline values (0-point) correspond to the last measured value prior to the start of CO2 inhalation. The last data point on the graphs correspond to values measured after the offset of CO2 administration. The x-axis displays the time in hours since the start of CO2 inhalation. a PCO2 trends for each patient during the study. Patients spent 95.1% of time (range: 44.6–98.5%) in the desired PCO2 range (40–60 mm Hg) during the 5% CO2 administration, calculated by linear interpolation between the blood gas measurements. All PCO2 values were >40 mm Hg, the lower value of the target range. b pH trends for each patient during the study. A repeated-measures linear mixed-effect model predicted that pH remained stable over time during the CO2 administration. Baseline value, time in hours since the beginning of inhalation, and Thompson encephalopathy score were considered to have fixed effects. c Base deficit trends for each patient during the study. The same model predicted that base deficit decreased by 0.61 mmol/L per hour throughout the CO2 inhalation period. d Lactate trends for each patient during the study. The same model predicted that lactate levels decreased by 0.55 mmol/L per hour throughout the CO2 inhalation period.