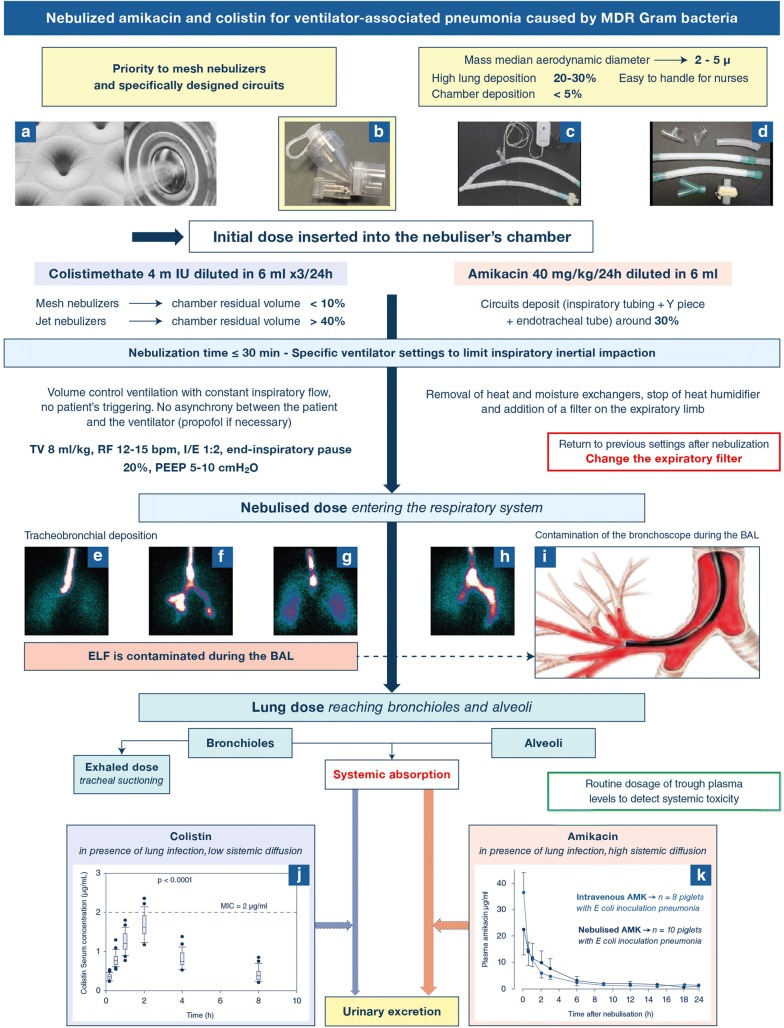
Fig. 1.
Nebulization of amikacin and colistin: from the nebulizer’s chamber to lung deposition and urinary excretion. a–c Mesh nebulizers positioned 15 cm from the Y piece, and made of a domed aperture plate with 1000 precision-formed holes which vibrates at 100 kHz. The vibration-induced micro-pumping effect produces a fine particle, low velocity aerosol. The mass median aerodynamic diameter depends and the holes’ diameter; d specific respirator tubings with smooth angle and inner surface; e–i illustrations of tracheobronchial deposition of aerosol particles. Scintigraphic images representing airways and lung deposition of an aerosol of diethylenetriaminepentaacetic acid labeled with technetium-99 m are shown in e–h. Images were obtained in four postoperative neurosurgery patients without pulmonary disease ventilated either in volume-controlled ventilation (n = 2, e and f) or in pressure support ventilation (n = 2, g and h). A part of the aerosol reached the lung periphery, but the majority impacted proximally in the trachea and large bronchi. Lung deposition was significantly greater in patients on volume-controlled mechanical ventilation; whereas, extrapulmonary deposition was significantly lower. i Illustrates the contamination of the bronchoscope during the BAL procedure (the red color indicates high aerosol bronchial concentration). Reproduced from Dugernier et al. [14] and Rouby et al. [5] with the permission of the publishers. j, k Illustrate the systemic diffusion of nebulized colistin (j) and aminoglycosides (k) in patients with ventilator-associated tracheobronchitis and in piglets with inoculation pneumonia. Amikacin plasma concentrations after intravenous administration are represented in blue and in black following nebulization. The nebulized dose was equal to the intravenous dose plus extrapulmonary deposition, so that equivalent amount entered the respiratory system either by the trachea (nebulization) or by the pulmonary artery (intravenous administration). Reproduced from Athanassia et al. [8] and Rouby et al. [1] with the permission of the publishers. TV tidal volume, RF respiratory frequency, bpm breaths per minute, I/E inspiratory:expiratory ratio; PEEP positive end-expiratory pressure, BAL bronchoalveolar lavage; m IU million International Units