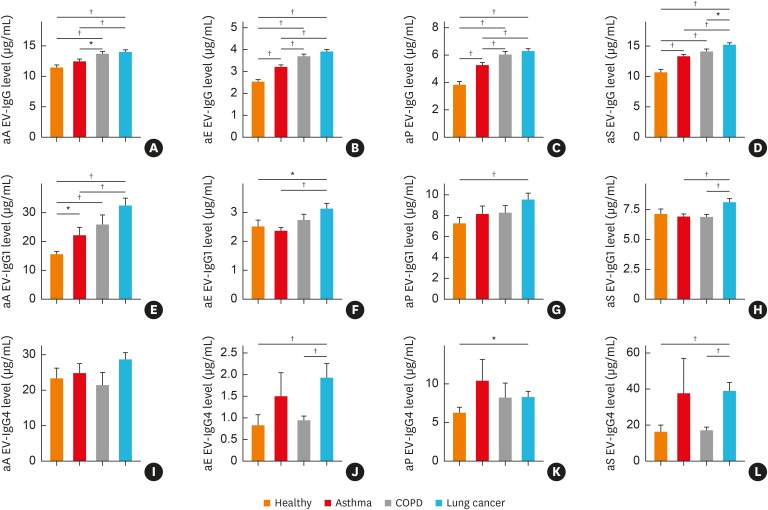
Fig. 3. Differences in IgG, IgG1 and IgG4 sensitization to microbial EVs, such as Acinetobacter baumannii, Enterobacter cloacae, Pseudomonas aeruginosa and Staphylococcus aureus among healthy subjects and patients with asthma, COPD or lung cancer. (A) IgG sensitization to A. baumannii EVs, (B) IgG sensitization to E. cloacae EVs, (C) IgG sensitization to P. aeruginosa EVs, (D) IgG sensitization to S. aureus EVs, (E) IgG1 sensitization to A. baumannii EVs, (F) IgG1 sensitization to E. cloacae EVs, (G) IgG1 sensitization to P. aeruginosa EVs, (H) IgG1 sensitization to S. aureus EVs, (I) IgG4 sensitization to A. baumannii EVs, (J) IgG4 sensitization to E. cloacae EVs, (K) IgG4 sensitization to P. aeruginosa EVs, (L) IgG4 sensitization to S. aureus EVs.
IgG, immunoglobulin G; EV, extracellular vesicle; COPD, chronic obstructive pulmonary disease; aE, anti-E. cloacae; aP, anti-P. aeruginosa; aS, anti-S. aureus; aA, anti-A. baumannii.
*P < 0.05, †P < 0.01.