Abstract
Background
Dead time may affect the accuracy of quantitative SPECT (QPSECT), and thus of dosimetry. The aim of this study was to quantify the effect of dead time on 177Lu-QSPECT and renal dosimetry following peptide receptor radionuclide therapy (PRRT) of neuroendocrine tumours.
Methods
QSPECT/CT was performed on days 1 and 3 during 564 personalized 177Lu-octreotate cycles in 166 patients. The dead-time data for each scanning time point was compiled. The impact of not correcting QSPECT for the dead time was assessed for the kidney dosimetry. This was also estimated for empiric PRRT by simulating in our cohort a regime of 7.4 GBq/cycle.
Results
The probability to observe a larger dead time increased with the injected activity. A dead-time loss greater than 5% affected 14.4% and 5.7% of QSPECT scans performed at days 1 and 3, respectively. This resulted in renal absorbed dose estimates that would have been underestimated by more than 5% in 5.7% of cycles if no dead-time correction was applied, with a maximum underestimation of 22.1%. In the simulated empiric regime, this potential dose underestimation would have been limited to 6.2%.
Conclusion
Dead-time correction improves the accuracy of dosimetry in 177Lu radionuclide therapy and is warranted in personalized PRRT.
Keywords: Dead time, Quantitative SPECT, Dosimetry, Radionuclide therapy, 177Lu
Background
Peptide receptor radionuclide therapy (PRRT) is an established palliative treatment for patients suffering from neuroendocrine tumours [1]. The widely adopted regime consists of four cycles of 7.4 GBq of 177Lu-octreotate. This empiric regime was designed to limit the cumulative absorbed dose to the kidney and bone marrow to 23 and 2 Gy, respectively, in the patient population [2, 3]. However, due to the very high inter-patient variability in the absorbed dose uptake per injected activity (IA) observed in the critical organs [4, 5], personalizing PRRT may be preferable in order to maximize the tumour absorbed dose while limiting that to critical organs. One way to achieve this is to personalize IA based on dosimetry to deliver a prescribed absorbed dose to a critical organ, such as 23 Gy to the kidneys over four induction cycles, which involves IA well above 7.4 GBq in some patients [5, 6]. The accuracy of dosimetry is dependent on that of quantitative imaging. We previously suggested, and recently updated, a practical method for 177Lu quantitative SPECT (QSPECT) with a dead-time correction that we implemented for routine clinical dosimetry [7, 8]. Our primary aim was to quantify, in a large cohort of patients undergoing personalized PRRT, the dead time—and the impact of not correcting for it—on the accuracy of 177Lu-QSPECT and dosimetry. Secondarily, we wanted to assess the same in the empiric regime of 7.4 GBq/cycle, by simulating the latter in our cohort.
Materials and methods
Patients and cycles
A total of 564 177Lu-octreotate cycles (median, 9.1 GBq; range, 0.7–33.7 GBq; Table 1) in 166 consecutive patients enrolled in our prospective clinical trial of personalized PRRT since April 2016 were analysed (NCT02754297) [6]. This included 32 empiric cycles (median, 7.6 GBq; range, 5.6–8.4 GBq) previously administered to 10 of these patients and 532 personalized cycles (median, 9.3 GBq; range, 0.7–33.7 GBq). The institutional Ethics Committee approved the study, and all patients provided a written consent to participate.
Table 1.
Injected activity, dead time and dosimetry data for personalized and simulated empiric PRRT cycles (n = 564)
| Minimum | 1st decile | Median | 9th decile | Maximum | |
|---|---|---|---|---|---|
| Personalized PRRT (actual) | |||||
| Injected activity (GBq) | 0.67 | 5.39 | 9.14 | 17.35 | 33.67 |
| Dead time | |||||
| Day 1 QSPECT (%) | 0.44 | 1.36 | 2.39 | 6.17 | 23.08 |
| Day 3 QSPECT (%) | 0.28 | 0.73 | 1.36 | 3.83 | 22.14 |
| Renal dosimetry | |||||
| Absorbed dose (Gy) | 0.93 | 3.58 | 6.07 | 8.42 | 25.89 |
| Absorbed dose per injected activity (Gy/GBq) | 0.14 | 0.34 | 0.63 | 1.11 | 4.93 |
| Deviation without dead-time correction (%) | 2.82 | − 0.58 | − 1.39 | − 3.84 | − 22.14 |
| Empiric PRRT (simulated, 7.4 GBq/cycle) | |||||
| Dead time | |||||
| Day 1 QSPECT (%) | 0.55 | 1.06 | 1.96 | 4.78 | 9.82 |
| Day 3 QSPECT (%) | 0.28 | 0.55 | 1.15 | 3.08 | 7.21 |
| Renal dosimetry | |||||
| Absorbed dose (Gy) | 1.07 | 2.53 | 4.64 | 8.23 | 36.46 |
| Deviation without dead-time correction (%) | 1.90 | − 0.54 | − 1.04 | − 2.60 | − 6.65 |
QSPECT and dosimetry
177Lu-QSPECT/CT was acquired and reconstructed as previously described using a Symbia T6 system (Siemens Healthineers, Erlangen, Germany), with the only modulated parameter being the time per projection (15 s for acquisitions the same day and the day following the injection, and 20 s for following days) [8]. Since photons of any energy can cause dead time, the dead-time correction factor was deduced from the average acquisition wide-spectrum (18–680 keV) counting rate using a lookup table [7, 8]. The dead time corresponds to one minus the inverse of the dead-time correction factor. We used the dead-time constant and calibration factor that were recently obtained (0.55 μs and 9.4 cps/MBq, respectively [8]), which were smaller than those initially estimated (0.78 μs and 10.8 cps/MBq, respectively [7]). Of note, when multiple bed positions were acquired, we considered the dead time of that encompassing the kidney, which was typically the greatest.
Our initial dosimetry protocol was based on a 3-time point QSPECT, at day 0 (~ 4 h), 1 (~ 24 h) and 3 (~72 h) post-injection. Since the day 0 scan contributes little to the accuracy of renal dosimetry, we stopped performing it [9]. Accordingly, dosimetry was computed using only day 1 and 3 scans in the present analysis. Like others, we sampled the activity concentration in tissues using 2-cm spherical volumes of interest [10]. Renal dosimetry was computed by fitting a monoexponential curve, multiplying the area under the time-activity concentration curve by an activity concentration dose factor of 87 mGy g/MBq/h and averaging the absorbed dose of both kidneys [5, 6, 9]. This factor was determined by multiplying the self-absorbed S value for the kidney (0.29 Gy/GBq h; OLINDA, Vanderbilt University, Nashville, TN, USA) with the mean kidney volume (300 ml, assuming 1 g = 1 ml). The dead-time loss observed for day 1 and 3 QSPECT, the absorbed dose to the kidney and its deviation without dead-time correction were plotted against the IA. Histograms of the proportion of scans and renal dose estimates that would have deviated by more than 5% or 10% in the absence of dead-time correction were drawn. Graphs and statistics were generated with R (v.1.2.1335; RStudio, Inc., Boston, MA, USA).
Simulation of empiric PRRT
To estimate the incidence and the impact of dead time in the context of the widely practised fixed-IA 177Lu-octreotate PRRT, we simulated an IA of 7.4 GBq for every cycle. The dead-time-corrected kidney activity concentration per IA was multiplied by 7.4 GBq for each imaging time point. We then multiplied the expected wide-spectrum count rate per IA by 7.4 GBq and retrieved the simulated dead-time correction factor from the lookup table. The same analyses described above were then conducted.
Results
Dead time and QSPECT
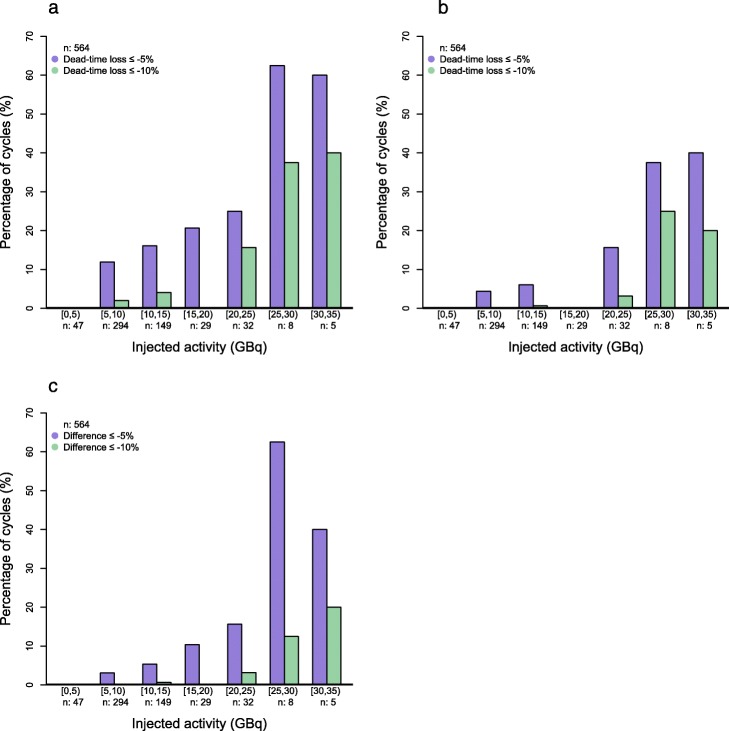
The median dead time was 2.4% and 1.4% for day 1 and day 3 QSPECT, respectively (Table 1). As expected, the dead time tended to increase with IA and reached up to 23.1% and 22.1%, respectively (Fig. 1a, b). We observed that 14.4% of the day 1 scans (in 23.5% of patients) were affected by a dead-time loss of 5% or more, while at day 3, this figure was 5.7% (in 7.2% of patients). More than 60% of day 1 scans suffered a dead time of at least 5% when the IA was 25 GBq or more (Fig. 2a, b).
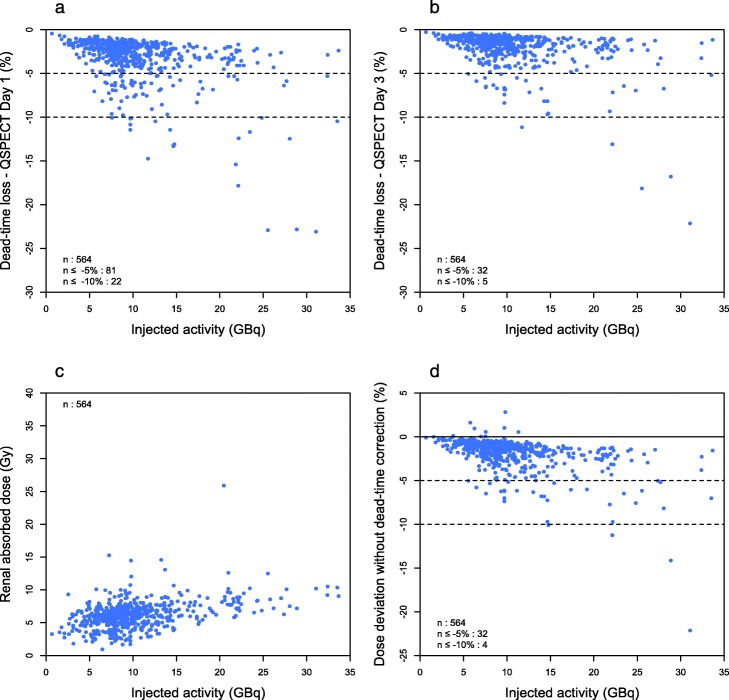
Fig. 1.
Dead time and renal dosimetry in personalized PRRT. The dead-time count loss affecting day 1 (a) and day 3 (b) QSPECT scans, the renal absorbed dose (c) and its deviation without dead-time correction (d) are plotted against the injected activity
Fig. 2.
Percentage histograms of cycles per injected activity strata during which the dead time affected day 1 (a) or day 3 (b) QSPECT, or during which the renal absorbed dose would have been underestimated without dead-time correction (c) by at least 5% (purple) or 10% (green)
Dead time and dosimetry
Since our personalized PRRT protocol aims at standardizing the kidney absorbed dose, the latter showed little dependence to IA (Fig. 1c), reflecting the high inter-patient variability in the absorbed dose per IA (Table 1). Not correcting for a dead time would have resulted in a median deviation of the renal absorbed dose by − 1.4%, and the underestimation could get as important as − 22.1% (Table 1). It exceeded − 5% in 5.7% of cycles in 10.2% of patients (Fig. 1d). The probability of a significant impact of dead-time correction on dosimetry increased with IA (Fig. 2c). In 54% of cases involving an IA of 25 GBq or more, dead-time correction avoided an underestimation greater than − 5% to occur. An example of such a case is presented (Fig. 3).
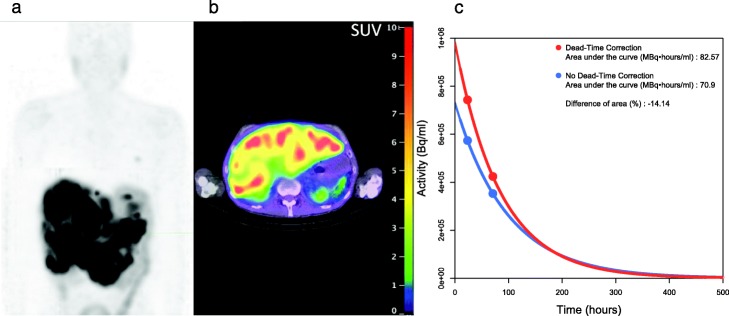
Fig. 3.
Day3 QSPECT maximum intensity projection (a), fused QSPECT/CT slice (b) and renal time-activity concentration curve (c) of a patient with extensive liver metastases who received 28.9 GBq 177Lu-octreotate at his second cycle. The dead time was 22.8% and 16.8% on day 1 and day 3 QSPECT, respectively. The area under the curve–and consequently, the renal absorbed dose – would have been underestimated by 14.1% without dead-time correction
Simulated empiric PRRT
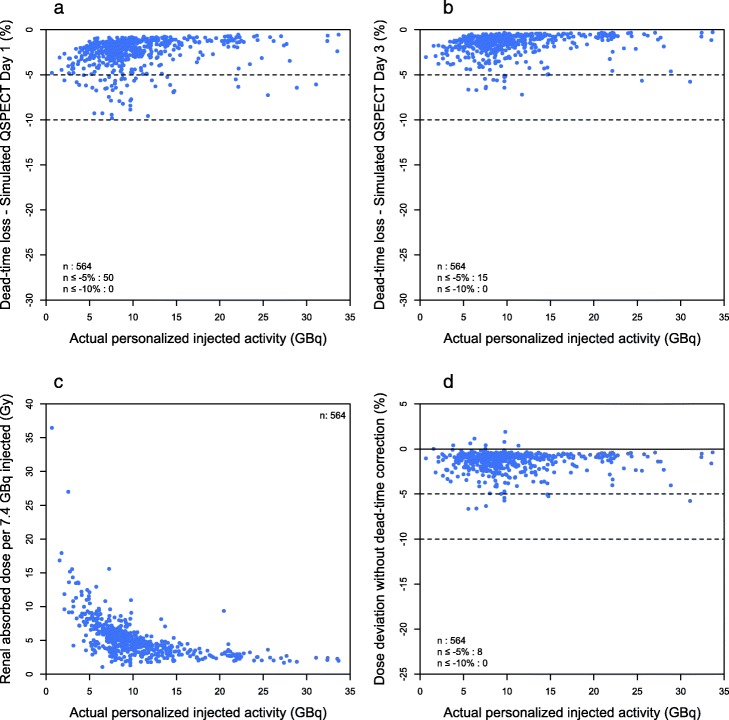
If all patients had received 7.4 GBq/cycle, the dead-time loss would not have exceeded 10% at both QSPECT time points (Table 1, Fig. 4a, b). The dead time was at least 5% in 8.9% and 2.7% for day 1 and day 3 scans, respectively (in 13.9% and 4.2% of patients, respectively). Not correcting for dead time would have resulted in an underestimation of kidney absorbed dose of at least − 5% in 1.4% of cycles. Of note, the absorbed dose to the kidney could have gotten as high as 36 Gy/cycle (4.9 Gy/GBq) if PRRT had not been personalized in our cohort (Fig. 4c). The maximum underestimation of renal absorbed dose when not correcting for dead time was − 6.15% (Fig. 4d).
Fig. 4.
Dead time and dosimetry in simulated empiric PRRT (7.4 GBq/cycle). The dead-time count loss affecting day 1 (a) and day 3 (b) QSPECT scans, the renal absorbed dose (c) and its deviation without dead-time correction (d) are plotted against the actual personalized injected activity
Discussion
With its low-yield medium-energy gamma emission (208 keV, 11%), 177Lu is a therapeutic radionuclide with favourable imaging characteristics. However, our results confirm that dead time, if not accounted for, affects the accuracy of 177Lu-QPSECT and consequent dosimetry estimates. The probability of significant dead time increases with the IA, but the level of dead time remains poorly predictable at any IA owing the very high inter-patient variability in 177Lu-octreotate retention, which in turn depends on individual factors such as tumour burden and renal function.
As others have found, the impact of dead time is limited when IA does not exceed the widely adopted empiric IA of 7.4 GBq [11, 12]. Nevertheless, simple dead-time correction methods can be easily implemented to maximize the accuracy of QSPECT and remove a layer of uncertainty which would otherwise sum up with many others when performing internal dosimetry [8, 12–14].
The proportion of patients whose dosimetry would be significantly impacted by the lack of dead-time correction is larger in personalized PRRT, which aims to optimize the treatment for each individual. In this regard, a personalized medicine approach is particularly concerned with outlier patients, even if they represent a minority of the population. In PRRT, outliers include patients with a very high tumour burden and consequent retention of 177Lu-octreotate combined with a fast activity clearance from the kidneys and other healthy tissues. While these patients are in great need for therapeutic effect, they are undertreated with empiric PRRT. Our personalized PRRT protocol aims to optimize the irradiation of their tumour by personalizing the IA to deliver a standardized renal absorbed dose. The latter would inevitably be exceeded if QSPECT was not dead-time corrected, exposing them to a higher risk of toxicity than intended. Furthermore, at the population level, risk assessment based on non-dead-time-corrected dosimetry data could result in underestimated safety thresholds, or overestimated risk for a given absorbed dose value.
Our results obtained using a SPECT/CT system equipped with NaI crystals are likely valid for other systems having a similar design. However, dead time is expected to be substantially lesser, if not negligible, using a system with pixelized CZT solid-state detectors in the same clinical setting [15].
Conclusion
For NaI crystal cameras, dead-time correction improves the accuracy of QSPECT and dosimetry in 177Lu radionuclide therapy. While dead-time correction is recommended for empiric PRRT, it becomes mandatory in personalized PRRT protocols involving custom IA per cycle. This will likely also apply to other 177Lu radionuclide therapies such as the rapidly emerging prostate-specific membrane antigen radioligand therapy.
Acknowledgements
We are grateful to our team of nuclear medicine physicians and technologists contributing to the care of the patients, in particular, to our technologist Nancy Lafrenière who performed most of the of original dosimetry analyses.
Abbreviations
- CZT
Cadmium zinc telluride
- IA
Injected activity
- PRRT
Peptide receptor radionuclide therapy
- QSPECT
Quantitative single-photon emission computed tomography
Authors’ contributions
AD participated in the design of the study, collected and analysed the data and drafted the manuscript. GB helped with data collection and analysis. GB, PD and AF revised the manuscript. JMB designed the study, supervised the project, contributed to the data analysis and edited the manuscript. All authors read and approved the final manuscript.
Funding
AD is the recipient of a Bourse interfacultaire from Cancer Research Centre, Université Laval. JMB is supported by a Clinical Research Scholarship from the Fonds de recherche du Québec – Santé. This work was funded by the Canadian Institutes of Health Research (CIHR) operating grant MOP-142233 to JMB.
Availability of data and materials
Please contact the corresponding author for the data used in this manuscript.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All patients enrolled in our P-PRRT trial (NCT02754297) and gave a written consent to participate. The institutional Ethics Committee (Comité d’éthique de la recherche CHU de Québec – Université Laval) approved the study.
Consent for publication
All authors read the manuscript and consented for its publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–135. doi: 10.1056/NEJMoa1607427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, et al. Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol. 2005;23(12):2754–2762. doi: 10.1200/JCO.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 3.Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26(13):2124–2130. doi: 10.1200/JCO.2007.15.2553. [DOI] [PubMed] [Google Scholar]
- 4.Sandström M, Garske-Román U, Granberg D, Johansson S, Widström C, Eriksson B, et al. Individualized dosimetry of kidney and bone marrow in patients undergoing 177Lu-DOTA-octreotate treatment. J Nucl Med. 2013;54(1):33–41. doi: 10.2967/jnumed.112.107524. [DOI] [PubMed] [Google Scholar]
- 5.Del Prete M, Buteau F-A, Beauregard J-M. Personalized 177Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: a simulation study. Eur J Nucl Med Mol Imaging. 2017;44(9):1490–1500. doi: 10.1007/s00259-017-3688-2. [DOI] [PubMed] [Google Scholar]
- 6.Del Prete M, Buteau F-A, Arsenault F, Saighi N, Bouchard L-O, Beaulieu A, et al. Personalized 177Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: initial results from the P-PRRT trial. Eur J Nucl Med Mol Imaging. 2019;46(3):728–742. doi: 10.1007/s00259-018-4209-7. [DOI] [PubMed] [Google Scholar]
- 7.Beauregard J-M, Hofman MS, Pereira JM, Eu P, Hicks RJ. Quantitative 177Lu SPECT (QSPECT) imaging using a commercially available SPECT/CT system. Cancer Imaging. 2011;11:56–66. doi: 10.1102/1470-7330.2011.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frezza A, Desport C, Uribe C, Zhao W, Celler A, Després P, et al. Comprehensive SPECT/CT system characterization and calibration for 177Lu quantitative SPECT (QSPECT) with dead-time correction. EJNMMI Phys. 2020;7(1):10. doi: 10.1186/s40658-020-0275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Del Prete M, Arsenault F, Saighi N, Zhao W, Buteau F-A, Celler A, et al. Accuracy and reproducibility of simplified QSPECT dosimetry for personalized 177Lu-octreotate PRRT. EJNMMI Phys. 2018;5(1):25. doi: 10.1186/s40658-018-0224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandström M, Garske U, Granberg D, Sundin A, Lundqvist H. Individualized dosimetry in patients undergoing therapy with 177Lu-DOTA-D-Phe1-Tyr3-octreotate. Eur J Nucl Med Mol Imaging. 2010;37(2):212–225. doi: 10.1007/s00259-009-1216-8. [DOI] [PubMed] [Google Scholar]
- 11.Marin G, Vanderlinden B, Karfis I, Guiot T, Wimana Z, Flamen P, et al. Accuracy and precision assessment for activity quantification in individualized dosimetry of 177Lu-DOTATATE therapy. EJNMMI Phys. 2017;4(1):7. doi: 10.1186/s40658-017-0174-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ljungberg M, Celler A, Konijnenberg MW, Eckerman KF, Dewaraja YK, Sjögreen-Gleisner K, et al. MIRD Pamphlet No. 26: Joint EANM/MIRD Guidelines for Quantitative 177Lu SPECT Applied for Dosimetry of Radiopharmaceutical Therapy. J Nucl Med. 2016;57(1):151–162. doi: 10.2967/jnumed.115.159012. [DOI] [PubMed] [Google Scholar]
- 13.Uribe CF, Esquinas PL, Gonzalez M, Zhao W, Tanguay J, Celler A. Deadtime effects in quantification of 177Lu activity for radionuclide therapy. EJNMMI Phys. 2018;5(1):2. doi: 10.1186/s40658-017-0202-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gear JI, Cox MG, Gustafsson J, Gleisner KS, Murray I, Glatting G, et al. EANM practical guidance on uncertainty analysis for molecular radiotherapy absorbed dose calculations. Eur J Nucl Med Mol Imaging. 2018;45(13):2456–2474. doi: 10.1007/s00259-018-4136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peterson TE, Furenlid LR. SPECT detectors: the Anger Camera and beyond. Phys Med Biol. 2011;56(17):R145–R182. doi: 10.1088/0031-9155/56/17/R01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Please contact the corresponding author for the data used in this manuscript.