Description of the Problem
The first clinical case of coronavirus disease 2019 (COVID-19) was reported in Wuhan in China in December 2019 [1]. Since then, there have been more than 1,171,000 confirmed cases and 68,000 deaths in the United States as of May 5, 2020 [2]. To mitigate the spread of the disease, the Governor of the Commonwealth of Massachusetts issued a “social distancing” order on March 23, 2020 [3], and the Massachusetts Department of Public Health issued a “stay-at-home” advisory on March 24, 2020 [4]. In this context, hospital networks implemented significant changes in practice and workflow, particularly among procedure-based specialties, to facilitate the anticipated surge in COVID-19-related hospital admissions. This report describes the changes in workflow, caseload, procedure prioritization, and staff deployment in a tertiary medical center during the COVID-19 pandemic.
What Was Done
Hospital Level
Elective surgeries and procedures have been postponed since March 16, 2020, to free up operation rooms and associated staff for intensive care unit (ICU) bed conversion and to enable possible future redeployment, respectively [5].
Interventional Radiology Division Level
To prepare for the anticipated COVID-19 surge, the interventional radiology (IR) administration evaluated all procedures scheduled after March 16, 2020, and categorized each procedure as “emergent or urgent,” “case by case,” or “elective,” with nearly all elective procedures postponed (Table 1 ). In addition, every procedure request was first evaluated for outpatient IR suite eligibility to decrease patients’ risks of hospital exposure.
Table 1.
Triage of IR procedures urgency during COVID-19 pandemic
| Category | Definitions |
|---|---|
| Emergent or urgent | All trauma cases Acute bleeding Hemodialysis access thrombectomy Urgent IVC filter placement Sepsis-related interventions (drainage, symptomatic effusions) Foreign body retrievals Peripheral arterial disease with rest pain (critical limb ischemia) |
| Case by case | Interventional oncology related treatment (ablation, SIRT, TACE), ports, catheters, prostate fiducials or SpaceOARs, fiducials for radiation therapy, biopsy for initial diagnosis and staging of cancer) Venous access for specific indications (stem cell therapy, intravenous antibiotics, chemotherapy) Feeding tubes for sustainment Dialysis-related interventions Painful bone compression requiring therapy (kyphoplasty) |
| Elective | Routine drain or line changes Vein sampling (adrenal or petrosal, etc) UFE, gonadal vein embolization IVC filter retrievals, chronic venous recanalization, EVLT, VenaSeal, sclerotherapy Arteriovenous or venous malformations Routine PAD Research biopsies Biopsies for mutation analysis (if not affecting cancer therapy) Thyroid biopsies |
All emergent or urgent cases were performed and elective cases were deferred. The remaining cases were assessed on an individual basis. COVID19 = coronavirus disease 2019; EVLT = endovascular laser therapy; IR = interventional radiology; IVC = inferior vena cava; PAD = peripheral arterial disease; SIRT = selective internal radiation therapy; TACE = transarterial chemoembolization; SpaceOAR = Space Organs at Risk (Augmenix, Waltham MA, USA), UFE = uterine fibroid embolization; VenaSeal (Medtronic, Minneapolis MN, USA).
IR attending physicians were assigned to a new ICU-based team to provide bedside venous access options for COVID-19 patients, and a more formalized ambulatory team of an IR trainee and attending physician was created to perform routine bedside procedures including ultrasound (US)-guided paracentesis, thoracentesis, or drainages in suitable COVID-19-positive and -negative patients to minimize patient transfer to reduce the risks of transmission during transportation. IR nursing and technologist staffing levels during this period were reviewed to ensure compatibility with staffing requirements elsewhere in the hospital.
Outcomes
All IR procedures performed in our division during the first 4 weeks of the COVID-19 pandemic (March 16, 2020, to April 17, 2020) were identified and analyzed before being compared with a similar 4-week period in 2019 (March 18, 2019, to April 19, 2019).
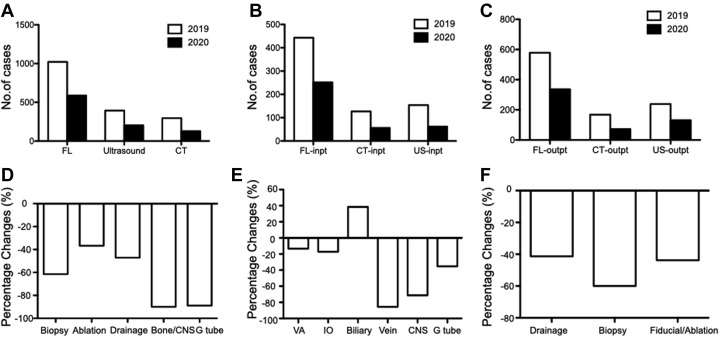
Changes of Total Case Volume
The number of IR procedures performed during the COVID-19 pandemic decreased from 1,710 to 919, constituting a 46% reduction when compared to the comparable period in 2019. Fluoroscopy (FL) was the most common modality used in both periods, accounting for approximately 60% of all procedures. The number of procedures decreased across all three modalities: the number of FL-guided procedures decreased from 1,022 to 588, US-guided procedures decreased from 393 to 203, and CT-guided procedures decreased from 295 to 128 (Fig. 1 A). The reduction in CT-guided procedure caseload (56.6%) was the largest during the COVID-19 pandemic when compared with FL-guided (42.5%) and US-guided (48.4%) procedures.
Fig 1.
A marked reduction in overall interventional radiology case volume was noticed during the coronavirus disease 2019 pandemic (March 16, 2020, to April 17, 2020) compared with the same time period in 2019, affecting all imaging modalities (A), as well as procedures performed in both inpatient (inpt) (B) and outpatient (outpt) (C) settings. The largest percentage decrease in CT-guided procedure volume was seen among bone and central nervous system (CNS) cases (D). Among fluoroscopy (FL)-guided procedures, biliary cases demonstrated a small percentage increase in number between 2019 and 2020, and venous access (VA) and interventional oncology (IO) procedures demonstrated the smallest percentage decrease (E). Among ultrasound (US)-guided procedures, biopsies decreased by the largest percentage (F). G tube = gastrostomy or jejunostomy tube placement.
Changes of Inpatient and Outpatient Settings
In 2019, inpatient procedures accounted for 42.3% of all IR procedures, compared with 41.3% during the COVID-19 pandemic. Among all inpatient procedures, CT-guided procedures experienced the greatest reduction (127 versus 56, 56%), followed by US-guided (154 versus 72, 53%) and FL-guided (442 versus 252, 43%) procedures (Fig. 1B). The overall number of outpatient procedures decreased by 45% (986 versus 539) during the COVID-19 pandemic compared with 2019. Similar to inpatient procedures, the number of CT-guided outpatient procedures demonstrated the greatest decrease among all modalities (168 versus 72, 57%), followed by US-guided (239 versus 131, 45%) and FL-guided (579 versus 336, 42%) procedures (Fig. 1C). There was an average of 30 venous catheters placed daily at beside in the ICUs during the COVID pandemic by the newly created ICU-based venous access team. Excluding venous access placement and removal, 27 bedside procedures were performed in the first 4 weeks of the COVID-19 pandemic, compared with 40 cases in the comparison period in 2019.
Changes of Case Type
Among CT-guided procedures, there was a 90% reduction in bone and central nervous system–related procedures (10 versus 1). The number of gastrostomy or jejunostomy tube placements decreased by 89% (9 versus 1). This compared with a 61.5% decrease in the number of biopsies (161 versus 62) and a 47% decrease in catheter drainages (85 versus 45), whereas the total volume of ablations only decreased by 36.7% (30 versus 19; Fig. 1D).
The number of FL-guided venograms (55 versus 8) and central nervous system–related procedures (164 versus 47) decreased the most (85% and 71%, respectively) in 2020. The number of FL-guided gastrostomy and jejunostomy placements decreased by 35% (85 versus 55). However, the number of FL-guided venous access and interventional oncology procedures only decreased by 13% (278 versus 241) and 17% (35 versus 29), respectively. In contrast, FL-guided biliary procedures increased by 38% during the COVID-19 pandemic (13 versus 18) (Fig. 1E).
Similar to CT-guided procedures, the number of US-guided procedures decreased significantly; biopsies decreased by 60% (145 versus 58), and ablations and fiducial placements and drainages and aspirations fell by 43.8% (16 versus 9) and 41.3% (230 versus 135), respectively (Fig. 1F).
Changes of Procedure Location and Staffing
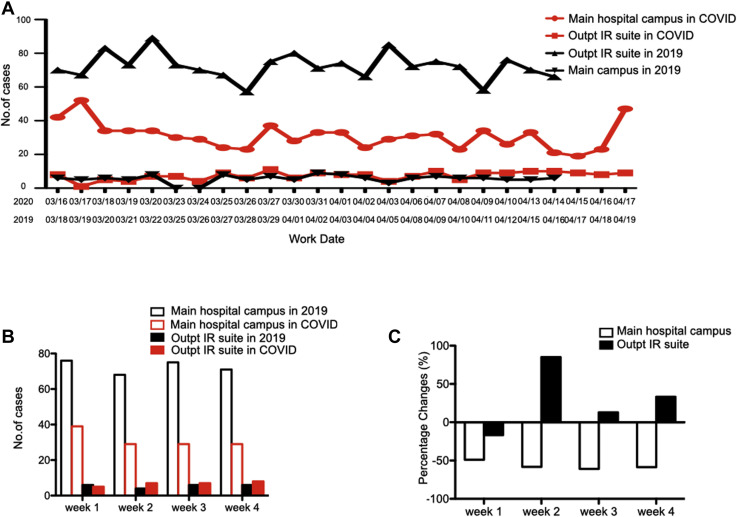
The number of cases performed on the main campus and outpatient IR suites were analyzed and compared (Fig. 2 A). Only cases performed on weekdays were included to allow a more accurate comparison because the outpatient IR suite did not operate on weekends. On the main hospital campus, the average number of IR procedures performed per weekday decreased by 56.7% during the first 4 weeks of the COVID-19 pandemic (72.7 versus 31.6). In comparison, average procedures performed at the outpatient IR suite per weekday increased by 23.4% during the pandemic (5.6 versus 6.9; Fig. 2B, 2C).
Fig 2.
There was a substantial reduction in daily caseload at the main hospital campus during the coronavirus disease 2019 (COVID-19) pandemic compared with 2019, and outpatient interventional radiology (IR) suite caseload remained stable (A). The reduction of caseload at the main hospital campus during the COVID-19 pandemic was observed in all 4 weeks, and weekly procedure numbers started to increase at the outpatient (Outpt) IR suite at the beginning of week 2 (B). The number of cases performed at the main hospital campus each week was consistently reduced by 50% during the COVID-19 pandemic, and the numbers of cases performed at the outpatient IR suite increased in 3 of the 4 weeks under review (C).
The IR division adjusted nursing and technologist staffing levels based on IR caseload and hospital redeployment requirements. On the main hospital campus, the number of technologists and registered nurses assigned to IR each day decreased by 47.6% (21 versus 11) and 56% (25 versus 11), respectively, during the first 4 weeks of the COVID-19 pandemic. IR nursing staff, all of whom are trained in critical care, were redeployed to staff newly created ICUs within the hospital. IR technologists were reassigned to meet the increased demand for portable chest radiographs, both on inpatient floors and newly created ambulatory respiratory assessment clinics. By contrast, in the outpatient IR suite, the number of assigned registered nurses remained the same, and the number of technologists increased by 50% (2 versus 3).
This study has some limitations. First, this study did not report patients’ COVID-19 status. All nonurgent or nonemergent interventional cases in COVID-19-positive patients were deferred or performed at the bedside per hospital policy to decrease the risks of transportation and staff exposures. Only one COVID-19-positive patient had a catheter exchange procedure performed during the first 4 weeks of the COVID-19 pandemic. However, the authors intend to follow up this study with more focus on the COVID-19 cohort as the pandemic evolves. Second, bedside venous access placement in the ICU by IR physicians during 2019 was not reported. Traditionally, the vast majority of temporary venous access placements in the ICU is performed by ICU physicians, and IR is only responsible for tunneled catheter placements in the IR suites. During the COVID-19 pandemic, the newly created ICU-based venous access team placed all temporary catheters in the ICU. Therefore, this new bedside ICU venous access service did not greatly impact the number of venous access procedures performed by IR during the period under review.
This report details the impact of COVID-19 on an IR division in a tertiary academic medical center during the COVID-19 pandemic, which may provide insights and information to other centers located in COVID-19 epicenters. The fall in cases within IR likely mirrors the significant changes in work patterns and caseloads across multiple specialties, something that has already been reflected in preliminary studies published elsewhere [6]. As the pandemic continues, we plan to continue to follow this early signal and re-allocate our resources to areas that require most urgent support. It is particularly crucial to meet patients’ needs given the decreased IR resources during the COVID-19 pandemic.
Footnotes
Dr Cahalane and Dr Cui contributed equally to this study and are co–first authors.
The authors state that they have no conflict of interest related to the material discussed in this article. Dr Cahalane is a fellow in Interventional Radiology, in an academic institution, non-partnership track. Dr Thabet, Dr Hirsch, Dr Cui, Dr Sutphin, Dr Kalva, and Dr Palmer are attending physicians in an academic institution and partners. Mr Sheridan is an employee in an academic institution, nonpartner, nonpartnership track.
References
- 1.Wu Y., Ho W., Huang Y. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395:949–950. doi: 10.1016/S0140-6736(20)30557-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus disease 2019 (COVID-19) cases in the U.S. National Center for Immunization and Respiratory Diseases (NCIRD) Division of Viral Diseases, ed. Centers for Disease Control and Prevention, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed May 6, 2020.
- 3.Baker CD, Polito K. Order assuring continued operation of essential services in the commonwealth, closing certain workplaces, and prohibiting gatherings of more than 10 people. In: Office of the Governor Commonwealth of Massachusetts, 2020. Available at: https://www.mass.gov/doc/march-23-2020-essential-services-and-revised-gatherings-order/download. Accessed May 6, 2020.
- 4.Safer-at-Home Advisory. Department of Public Health Advisory ed. Massachusetts Department of Public Health, 2020. Available at: https://www.mass.gov/news/safer-at-home-advisory. Accessed May 6, 2020.
- 5.Lancaster E.M., Sosa J.A., Sammann A. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064–1073. doi: 10.1016/j.jamcollsurg.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]