Abstract
The factors that guarantee the survival of the unicompartmental prosthesis implant seems to be linked to the accurate positioning of the components. The aim of our study is to compare the standard operative technique and the assisted navigation technique to understand if the robotic technology is able to obtain more accurate implants and with a better outcome. In the period between January 2016 and February 2018, in our Clinic, were performed 94 medial unicompartmental knee implants. The implantation of the medial unicompartmental prosthesis was performed in 30 cases with the standard technique and in 29 cases with the image-free robotic technique (Navio Surgical System). The objective of our study was to evaluate the anatomical and mechanical axes, the tibial slope, the coronal inclination of the femoral tibial space, the coronal angulation of the tibial and femoral component and the height of the Joint-Line. Furthermore, to evaluate the outcome we has execute international scores (IKDC and KSS Insall mod.). The advanced navigation seems to allow the implantation of the unicompartmental prosthesis more precisely, although not always with a statistically significant difference compared to the standard technique. further clinical studies are needed to analyze the medium and long-term survival rate, as well as the patient’s subjective outcome. (www.actabiomedica.it)
Keywords: knee arthroplasty, image-free robotic technique, knee
Introduction
Unicompartmental arthritis of the knee is a disease that can be tackled with different approaches, both conservative and surgical. Among the surgical approaches, we find some that act inside the articulation and others outside of it (1). The unicompartmental knee prosthesis has undeniable advantages when the right directions are followed (2). Rapid ricovery of the function, lower hospitalization, lower perioperative comorbidities, better outcomes and, not to be underestimated, lower perioperative costs (3, 4). In fact, the unicompartmental prothesis, compared to the total one, shows better results both in terms of Forgotten Knee Score and High Flexion Knee Score (5, 6).
Unfortunately, there are also some disadvantages. The most important is the higher revision rate compared to the total knee replacements. Some 30-years projections show that the revision rate is almost double (7). The works of Murray et al. and Liddle et al show that this problem is attributable to the volume of interventions. In specialized centers where are performed a large number of unicompartmental prosthesis implants, the revision rate are comparable with those of total prostheses (8, 9)
The factors that guarantee the survival of the unicompartmental prosthesis implant seems to be linked to the accurate positioning of the components. Among all, the conservation of the normal kinematics and the optimal positioning of the tibial components are protective factors against wear and potential failure of the implant (10).
These statements can give the idea that an implant positioned as accurately as possible can guarantee a better outcome, especially in the long term.
The aim of our study is to compare the standard operative technique and the assisted navigation technique to understand if the robotic technology is able to obtain more accurate implants and with a better outcome.
Materials and Methods
In the period between January 2016 and February 2018, in our Clinic, were performed 94 medial unicompartmental knee implants. The Journey UNI (S&N) prosthesis was implanted in 59 cases. Implants with Journey UNI were performed by a single experienced surgeon. The sample of 59 patients was homogeneous by sex, age (69,2 years of average) and BMI (average of 25,7).
The implantation of the medial unicompartmental prosthesis was performed in 30 cases with the standard technique and in 29 cases with the image-free robotic technique (Navio Surgical System).
To evaluate the results, the patients made a careful clinical examination in the pre-operative and 4 months after the surgery, and they made radiographic investigations in the pre-operative and in the post-operative after 4 months, morover they compiled some international scores (IKDC and KSS Insall mod.) both in pre and post-operative period. In particular, for the clinical examination were evaluated flexion, extension and the pain. For instrumental examinations were performed x-rays in antero-posterior projection under load, lateral projection, axial projection at 45° for patella, Kneeling View and pangonogram of lower limbs.
The objective was to evaluate the anatomical and mechanical axes, the tibial slope, the coronal inclination of the femoral tibial space, the coronal angulation of the tibial and femoral component and the height of the Joint-Line. Radiographic investigations and measurements were performed by a single radiologist.
Results
The results of the post-operative assessment showed a good recovery of flexion and extension in both groups of patients: in the group subjected to intervention with the standard technique there was a deficit of extension always <5° and an average flexion of 118°. In the Navio group, the results were similar: the extension was always excellent (deficit always <5°) and an average flexion of 127°, slightly better than the standard technique.
Also the evaluation of pain is comparable in the two groups: according to the NRS scale, the average pain recorded in the Standard group is 2,3, while in the Navio group is 1,9. The results of the scores given to the patients show good results. In the Standard group, IKDC before and after surgery were respectively 74,7 and 87,0, while in the Navio group they were 74,3 and 89,9 respectively. We have to say that the best result of the Navio group (+2,9) isn’t statistically significant. Concerning the KSS score, the trend was similar: in the Standard group the pre- and post-operative evaluation gave respectively 58,9 and 81,1, while for the Navio group respectively 58,6 and 83,2. Also for the KSS there was a better result in the Navio group (+2,1), that is still not statistically significant.
In the pre- and post-operative pangonogram was evaluated the possible variation of the anatomical axis: in both groups there was never a variation greater than 5°. In the Standard group the variance from the anatomical axis recorded in the pre-operative was ±2.1°. In the Navio group the variance recorded was lower, ±1.3°. These results have no statistical value. Also the radiographic evaluation of the tibial slope and the height of the Joint Line showed similar results: the variance recorded from the pre to post-operative for the tibial slope is ± 3.1° in the Standard group and ±1,7° in the Navio group. Concerning the Joint Line, was found a variance with the pre-operative in the Standard group of ±1,7 mm and in the Navio group of ±1.1 mm. The values also have no statistical significance.
Discussion
In literature there is a lot of interest about this topic: in fact, there are numerous studies that analyze the advantages of robotic surgery in orthopedics. In a review by Lonner et al are analyzed some of the most widespread robotic technologies for orthopedic (11). However, there are few studies concerning advanced image-free navigation and for the most they concern studies on dead bodies (12) and synthetic bone (13). Only a few studies analyze retrospectively clinical data and the results show always greater accuracy in the positioning of prosthetic components: for example, in the work by Harry et al, the height of the Joint Line is taken into consideration as a parameter (14).
Ours is certainly a preliminary work and the results presented must by analyzed in a more detailed way. But it’s based on clinical results and on measurements taken without the aid of the navigation system itself, and therefore independently performed. That allows us to evaluate the result and the accuracy of the system in guiding us in the positioning that we have previously planned. The overall results obtained by adding the two groups allow us to affirm that in both cases the implantation of the unicompartmental prothesis is effective in terms of subjective and radiographic outcomes. The results are therefore aligned with the literature and allow patients to improve their initial conditions (6).
However, it must be emphasized that the study has important critical points. First of all, the number of the sample is very limited, mainly due to two reasons: in addition to the small number of patients enrolled, the volume of interventions and the possibility of access to this technology were certainly a problem. Currently, the accessibility to this technology is easier, so our work will continue and will probably have greater scientific weight. Also, in all the assessments made there is a minimal superiority of the results obtained with the computer-assisted procedure Navio Surgical System, although never statistically significant: that agrees with numerous articles in literature (13-16).
Our technology is image-free and therefore doesn’t require the pre-operative processing of data from CT radiographic investigations, such as some system on the market. That can certainly be considered an advantage as there is less exposure to ionizing radiation from the patient. The image-free system don’t have the risk of working on wrong or modified data, because they are recorded at the same time as the surgery. On the other hand, with systems that require CT investigations, there is a risk that the information collected with the radiological investigation has changed at the time of the surgery, if there is a significant period of time between the two moments.
Another advantage of the Navio advanced navigation system is that it allows the surgeon to assess and quantify the tension of the soft tissues in real time, by simulating different scenarios, depending on the virtual positioning of the prosthetic components (12). Before making the cuts with the aid of the robotic cutter, it’s possible to verify, thanks to previously collected data, the real dimensions of the implant and its dynamic behavior, the articular kinematics as well as the variation of the contact points of the components, depending on the degree of flexion.
These advantages and the absolutely preliminary results allow us to affirm that, despite the limited number of our sample and the short-term follow-up, the Navio system has shown a greater accuracy in the positioning of the prosthetic components (13, 15, 16).
Figure 1.
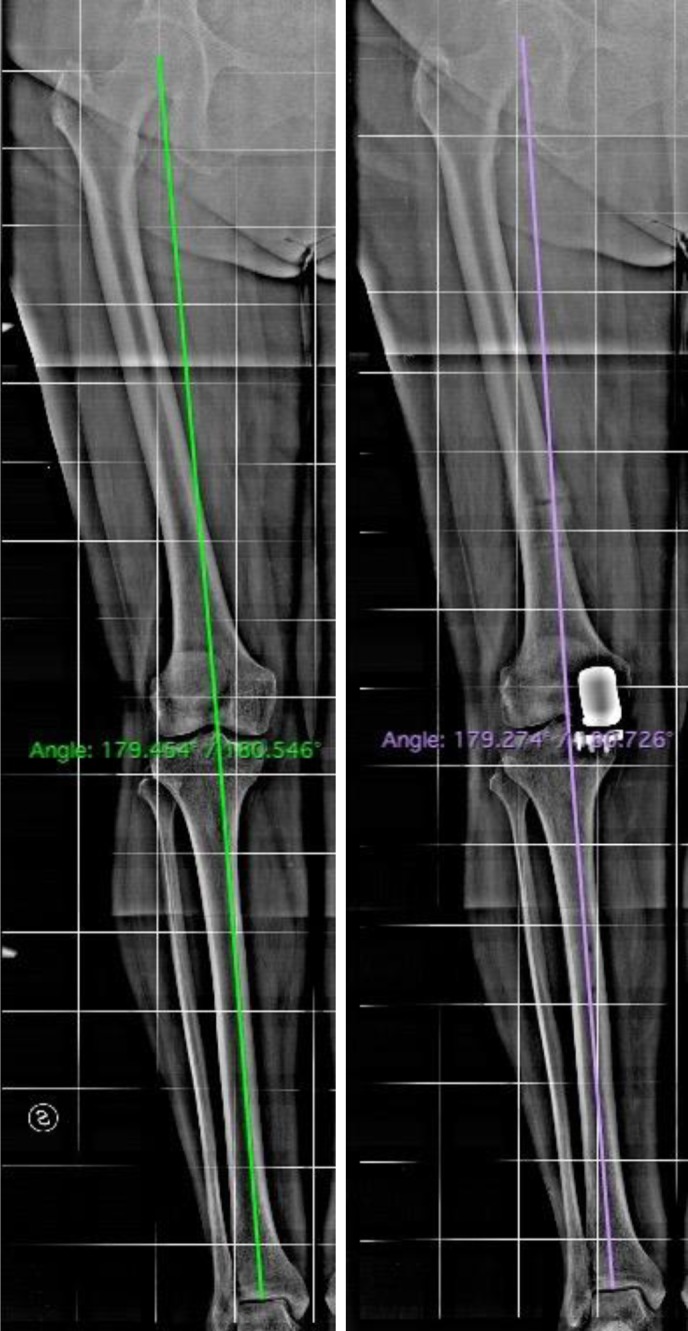
Pangonogram pre- and post-operative
Conclusions
The advanced navigation or image-free robotic technique seems to allow the implantation of the unicompartmental prosthesis more precisely, although not always with a statistically significant difference compared to the standard technique. Surely, this is a safe procedure for the patient and is simple for the surgeon. However, further clinical studies are needed to analyze the medium and long-term survival rate, as well as the patient’s subjective outcome.
The simplicity of the procedure may suggest that it’s also suitable for young orthopedic surgeons, but probably is not so (17). This technology certainly has the capacity to be didactic, but it must be used by those who completely dominate the standard technique. The possible switch to the traditional technique may be necessary to take on with some intraoperative complications or even with the instrumentation itself.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Pogliacomi F, Defilippo M, Guardoli A, Scaravella E. High tibial osteotomy: our experience with hemicallotasis method. Acta Biomed. 2014;85(Suppl 2):85–90. [PubMed] [Google Scholar]
- 2.Vaienti E, Scita G, Ceccarelli F, Pogliacomi F. Understanding the human knee and its relationship to total knee replacement. Acta Biomed. 2017;88(2S):6–16. doi: 10.23750/abm.v88i2-S.6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lum ZC, Lombardi AV, Hurst JM, Morris MJ, Adams JB, Berend KR. Early outcomes of twin-peg mobile-bearing unicompartmental knee arthroplasty compared with primary total knee arthroplasty. The bone & joint journal. 2016;98-B(10 Supple B):28–33. doi: 10.1302/0301-620X.98B10.BJJ-2016-0414.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shankar S, Tetreault MW, Jegier BJ, Andersson GB, Della Valle CJ. A cost comparison of unicompartmental and total knee arthroplasty. Knee. 2016;23(6):1016–1019. doi: 10.1016/j.knee.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Kim MS, Koh IJ, Choi YJ, Lee JY, In Y. Differences in Patient-Reported Outcomes Between Unicompartmental and Total Knee Arthroplasties: A Propensity Score-Matched Analysis. J Arthroplasty. 2017;32(5):1453–1459. doi: 10.1016/j.arth.2016.11.034. [DOI] [PubMed] [Google Scholar]
- 6.Zuiderbaan HA, van der List JP, Khamaisy S, Nawabi DH, Thein R, Ishmael C, et al. Unicompartmental knee arthroplasty versus total knee arthroplasty: Which type of artificial joint do patients forget. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):681–686. doi: 10.1007/s00167-015-3868-1. [DOI] [PubMed] [Google Scholar]
- 7.Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis. Knee. 2017;24(2):179–190. doi: 10.1016/j.knee.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Liddle AD, Pandit H, Judge A, Murray DW. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. The bone & joint journal. 2015;97-B(11):1506–1511. doi: 10.1302/0301-620X.97B11.35551. [DOI] [PubMed] [Google Scholar]
- 9.Murray DW, Liddle AD, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty. The bone & joint journal. 2015;97-B(10 Suppl A):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J, et al. Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival. Orthop Traumatol Surg Res. 2013;99(4 Suppl):S219–225. doi: 10.1016/j.otsr.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Lonner JH, Klement MR. Robotic-assisted Medial Unicompartmental Knee Arthroplasty: Options and Outcomes. J Am Acad Orthop Surg. 2018 doi: 10.5435/JAAOS-D-17-00710. [DOI] [PubMed] [Google Scholar]
- 12.Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res. 2015;473(1):206–212. doi: 10.1007/s11999-014-3764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith JR, Riches PE, Rowe PJ. Accuracy of a freehand sculpting tool for unicondylar knee replacement. Int J Med Robot. 2014;10(2):162–169. doi: 10.1002/rcs.1522. [DOI] [PubMed] [Google Scholar]
- 14.Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop. 2017;41(11):2265–2271. doi: 10.1007/s00264-017-3633-9. [DOI] [PubMed] [Google Scholar]
- 15.Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88(2):188–197. doi: 10.1302/0301-620X.88B2.17220. [DOI] [PubMed] [Google Scholar]
- 16.Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty. 2012;27(5):803–808. doi: 10.1016/j.arth.2011.09.021. e801. [DOI] [PubMed] [Google Scholar]
- 17.Karia M, Masjedi M, Andrews B, Jaffry Z, Cobb J. Robotic assistance enables inexperienced surgeons to perform unicompartmental knee arthroplasties on dry bone models with accuracy superior to conventional methods. Adv Orthop. 2013;2013:481039. doi: 10.1155/2013/481039. [DOI] [PMC free article] [PubMed] [Google Scholar]


