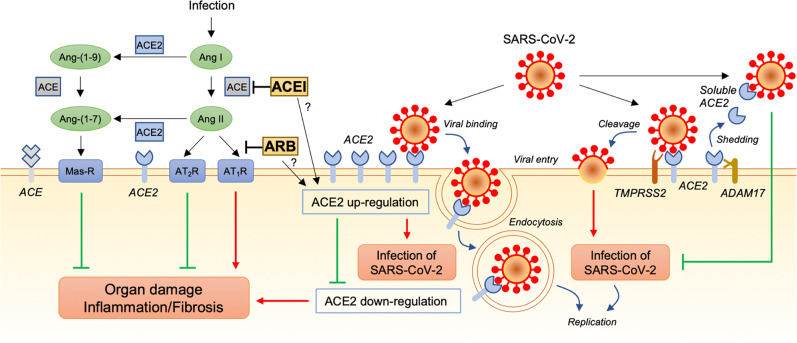
Fig. 1.
Possible associations of the renin-angiotensin system with SARS-CoV-2 infection and lung injury caused by SARS-CoV-2. Angiotensin-converting enzyme (ACE) converts angiotensin I (Ang I) to angiotensin II (Ang II). Ang II signaling leads to organ damage, such as lung injury, by promoting inflammation and fibrosis through the Ang II type 1 receptor (AT1R) and has opposing effects through the Ang II type 2 receptor (AT2R). Angiotensin-converting enzyme 2 (ACE2) converts Ang II to Ang-(1–7) and Ang I to Ang-(1–9). Ang-(1–7) signaling attenuates the effects of inflammation and fibrosis through the Mas receptor (Mas-R). It has been suggested that ACE2 is upregulated by some ACE inhibitors (ACEIs) and AT1R blockers (ARBs). ACE2 is also a receptor of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). ACE2-binding SARS-CoV-2 is internalized by endocytosis into the cell, and membrane-anchored ACE2 on the cell surface is downregulated. Downregulation of ACE2 promotes organ damage through activation of the ACE/Ang II/AT1R pathway and deactivation of the ACE2/Ang-(1–7)/Mas-R pathway. Another mechanism of SARS-CoV-2 infection is transmembrane protease serine 2 (TMPRSS2)-mediated cleavage of SARS-CoV-2 accompanied by ACE2. ACE2 is also shed from the membrane by a disintegrin and metalloproteinase 17 (ADAM17), and the soluble form of ACE2 may intercept the virus from binding to membrane-anchored ACE2 in the cell plasma membrane. Possible increases in the expression and soluble form of ACE2 induced by RAS inhibitors would have beneficial effects of protection against lung injury and other organ damage but not infection with SARS-CoV-2