Abstract
During the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak in Wuhan, China, we experienced a case of SARS-CoV-2 infection with atypical presentations in a patient with acute obstructive suppurative cholangitis (AOSC), who was initially admitted with jaundice and fever. The patient had no other typical symptoms of COVID-19 such as cough, dyspnea, nausea, vomiting, abdominal pain and diarrhea except for fever, but her epidemiological history was clear. COVID-19 was finally confirmed by repeated viral nucleic acid testing, but her repetitive lungs CT imaging findings had been atypical. After endoscopic-related operations and antiviral treatment, the patient was subsequently recovered and discharged. This particular case is being reported to provide a reference and guidance for the diagnosis and management of COVID-19 in AOSC.
Keywords: COVID-19, SARS-CoV-2, Acute obstructive suppurative cholangitis, AOSC
Introduction
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, which seriously threatens human health. Since the disease was first discovered from Wuhan, Hubei province, China in December 2019, the epidemic has rapidly spread to many countries around the world [1], [2]. As of May 1, 2020, a total of 3,175,207 COVID-19 cases were confirmed globally, including 224,172 deaths [2]. Compared with SARS-CoV and MERS-CoV, SARS-CoV-2 has a lower fatality rate but is more contagious [3], [4]. After being exposed to the virus, patients infected with SARS-CoV-2 usually present with fever, respiratory symptoms, gastrointestinal symptoms, fatigue, or myalgia within 14-day incubation period [5], [6], [7], [8], [9]. Typical pulmonary CT imaging features of COVID-19 patients are patchy shadows, ground-glass opacities, or consolidation [6], [7], [8]. The confirmation of SARS-CoV-2 infection depends on viral nucleic acid detection.
Acute obstructive suppurative cholangitis (AOSC) is a severe infectious disease caused by bile duct obstruction, which is the leading cause of death in biliary benign diseases. The disease has the characteristics of acute onset, rapid progression, severe and complicated clinical conditions, multiple complications, and high mortality. The typical clinical manifestations of AOSC are abdominal pain, jaundice, chills, fever, shock, and central nervous system depression. The common bile duct stones are the most common cause of the disease. Other causes include biliary ascariasis, benign biliary stenosis, anastomotic stenosis, and tumor. Treatments for this disease include open surgery, laparoscopic surgery, endoscopy, endoscopic retrograde cholangiopancreatography (ERCP), endoscopic sphincterotomy (EST), and endoscopic nose biliary drainage (ENBD).
The pathophysiological changes of AOSC can lead to decreased immune function and multiple organ dysfunction, making those with AOSC more susceptible to SARS-CoV-2 than the general population. During the SARS-CoV-2 outbreak in Wuhan, China, we experienced a case of COVID-19 with nontypical presentations in a patient with AOSC. Herein, we presented the clinical and imaging features of COVID-19 in an AOSC patient, and retrospected our diagnosis and management for this case, as well as the control measures to reduce spread of SARS-CoV-2 to other inpatients and health workers. These exceptions of this case are extremely important in the diagnosis and management of SARS-CoV-2-infected AOSC patients and to control the potential spread of SARS-CoV-2 in the hospital.
Case presentation
On February 2, 2020, a 71-year-old woman was admitted to the Renmin Hospital of Wuhan University because of a 1-week history of yellow skin. One day earlier, she developed fever with a temperature of 39.0 degree centigrade, and no chills, respiratory symptoms, gastrointestinal symptoms, fatigue or myalgia. She has a history of diabetes and had acute cholecystitis 1 year ago. On physical examination, her vital signs were poor, body temperature was 39.0 degree centigrade, pulse rate was 98 beats/minute, blood pressure was 99/40 mmHg, and respiratory rate was 20 breaths/minute. She presented with poor consciousness, lethargy, thin body, and serious yellow of the skin and sclera. Abdominal physical examination revealed tenderness in the upper abdomen, but no rebound pain or muscle tension. Laboratory tests showed a white blood cell count of 22.59 × 109/L (reference interval, 3.5–9.5 × 109/L), neutrophil ratio of 93.70% (reference interval, 40.0–75.0%), neutrophil count of 21.16 × 109/L (reference interval, 1.8–6.3 × 109/L), hemoglobin level of 87 g/L (reference interval, 115–150 g/L), red blood cell count of 2.78 × 1012/L (reference interval, 3.80–5.10 × 1012/L), hematocrit of 0.24 (reference interval, 0.350–0.450), alanine aminotransferase level of 34 U/L (reference interval, 7–40 U/L), aspartate aminotransferase level of 34 U/L (reference interval, 13–35 U/L), gamma-glutamyl transferase level of 754 U/L (reference interval, 7–45 U/L), alkaline phosphatase level of 481 U/L (reference interval, 50–135 U/L), albumin level of 19.8 g/L (reference interval, 40.0–55.0 g/L), total bilirubin level of 345.02 umol/L (reference interval, 0–23 umol/L), direct bilirubin level of 248.70 umol/L (reference interval, 0–8 umol/L), and procalcitonin level of 28.000 ng/mL (reference interval, < 0.1 ng/mL). Plain computed tomography (CT) of the abdomen revealed intra- and extra-hepatic bile duct dilatation, pancreatic duct dilatation, pancreatic atrophy, gallbladder stones, increased gallbladder volume, and slightly thickened gallbladder walls (Fig. 1 ). Considering that SARS-CoV-2 was raging in Wuhan, China at the time, and the patient had been living in Wuhan, chest CT plain scan and viral nucleic acid test were thus performed for the patient to exclude COVID-19. Chest CT revealed that high-density strip shadows in the lungs (Fig. 2 ). Samples were obtained from nasopharyngeal swabs for the detection of viral nucleic acid. The testing of 2019-nCoV ribonucleic acid (RNA) showed that the nucleocapsid protein (2019-nCoV-NP) gene and open reading frame lab (2019-nCoV-ORF-lab) were negative. Therefore, the diagnosis of AOSC, cholecystolithiasis, chronic cholecystitis, pneumonia, moderate anemia, hypoproteinemia, and diabetes was initially considered in accordance with the patient's symptoms, signs, and auxiliary examination.
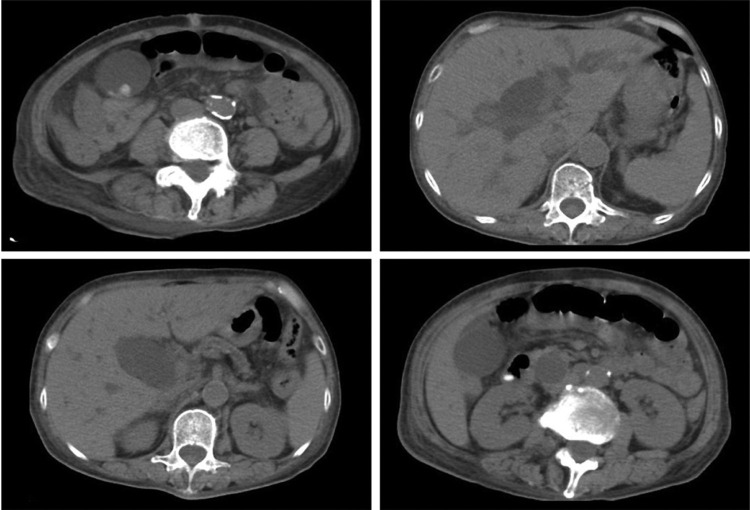
Figure 1.
Plain abdominal CT (computed tomography), February 2, 2020 (Illness Day 7). Intra- and extra-hepatic bile duct dilatation, pancreatic duct dilatation, pancreatic atrophy, gallbladder stones, increased gallbladder volume, and slightly thickened gallbladder walls were visible.
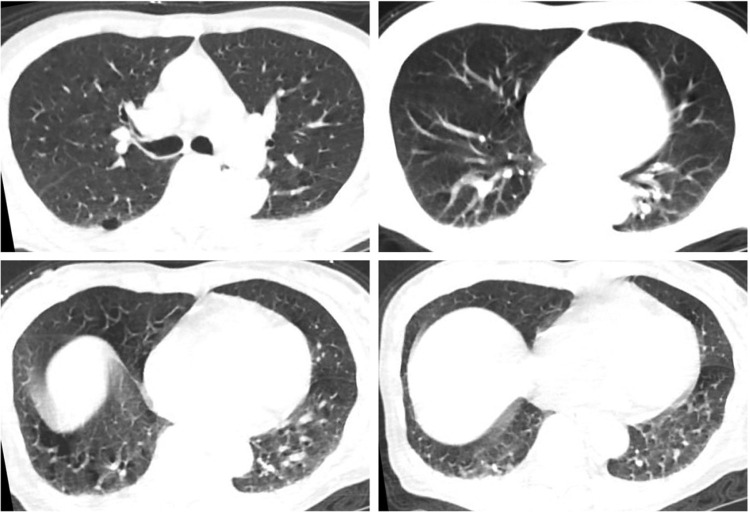
Figure 2.
Plain chest CT, February 2, 2020 (Illness Day 7). High-density strip shadows in the lungs were visible.
On February 3, 2020, ERCP, EST, and ENBD were performed to resolve the patient's bile duct obstruction. Brown, silt-like bile was seen, and the bile duct was dilated with a maximum diameter of 2.5 cm during the operation (Fig. 3 ). The operation was successfully completed. On the 9th day after the operation, the patient complained of a fever of 37.8 degree centigrade, and then the testing for 2019-nCoV RNA showed that 2019-nCoV-NP was suspicious, and 2019-nCoV-ORF-lab was negative. On the 11th day after the operation, the detection of 2019-nCoV RNA was performed again. The results showed that 2019-nCoV-NP was positive and 2019-nCoV-ORF-lab was negative. Chest CT still revealed strip shadows in the lungs (Fig. 4 ). Eventually, the patient was identified as COVID-19 and was immediately transferred to the Infectious Department. After 10 days of antiviral treatment, the patient's fever subsided, and her temperature was normal for three consecutive days. The results of two viral nucleic acid tests with a 1-day interval were negative. Chest CT showed that strip shadows still existed in the lungs, but which were significantly less than before (Fig. 5 ). Since the patient was identified as a suspected case of COVID-19, we have taken corresponding protective measures and implemented quarantine management for the patient. All medical staff took strict protective measures when contacting the patient, including wearing personal protective equipment (PPE), isolation gowns, N95 respirators, surgical masks, operating caps, goggles, and medical gloves. In addition, mobile medical devices were used to minimize the number of times that patients left the ward, thereby reducing the widespread spread of the virus. As of now, health workers associated with this patient have not been infected.
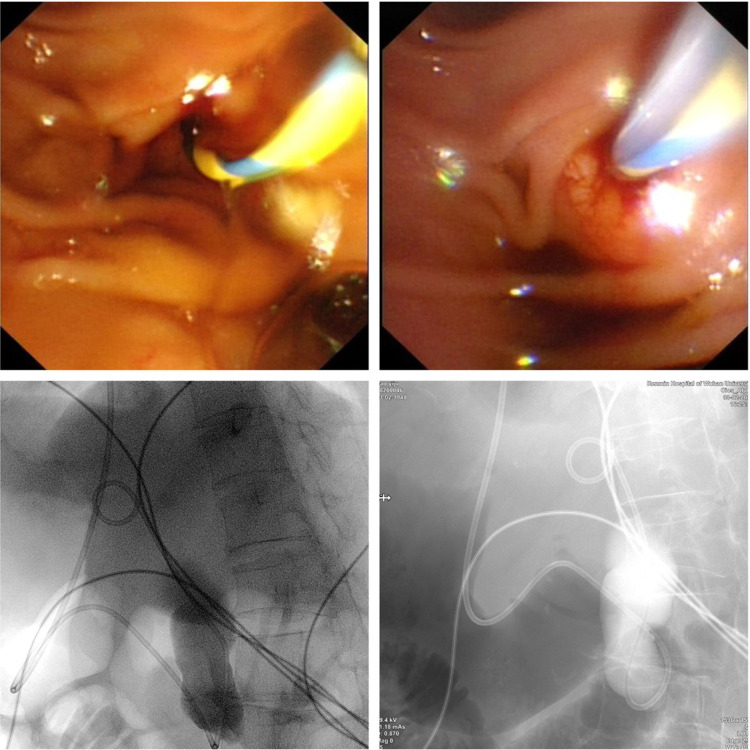
Figure 3.
Endoscopic retrograde cholangiopancreatography (ERCP), Endoscopic sphincterotomy (EST), and Endoscopic nose biliary drainage (ENBD), February 3, 2020 (Illness Day 8, Hospital Day 1). Brown silt-like bile, and dilated bile duct were visible.
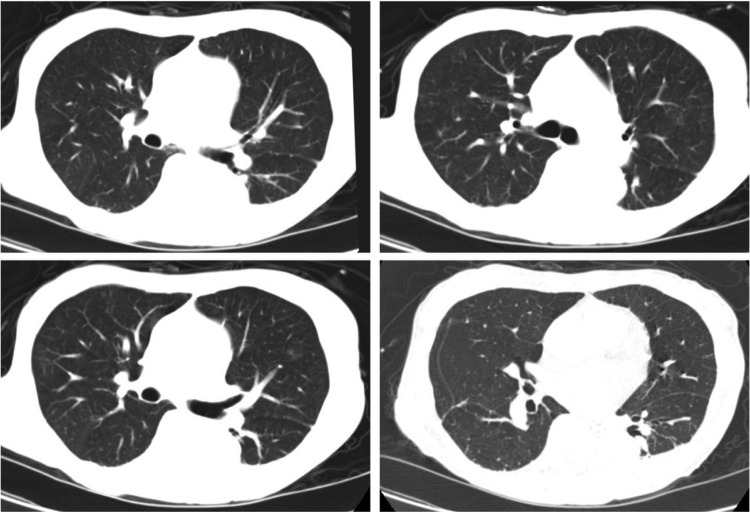
Figure 4.
Plain chest CT, February 14, 2020 (Illness Day 19, Hospital Day 12, Postoperation Day 11). Strip shadows in the lungs were still visible.
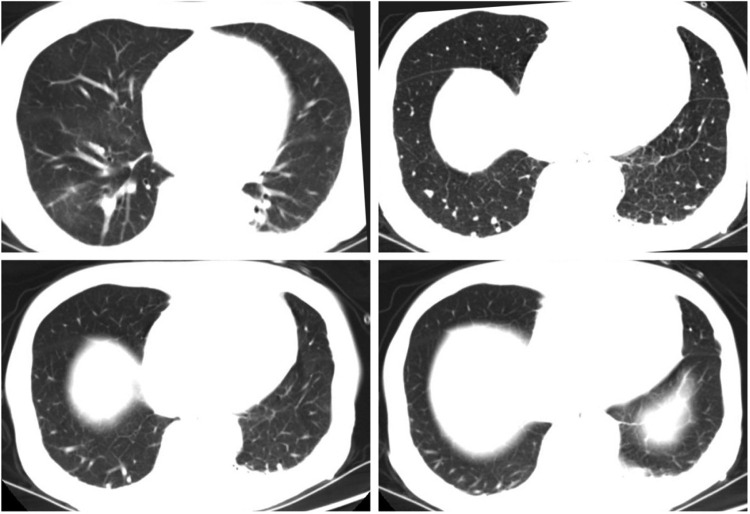
Figure 5.
Plain chest CT, February 24, 2020 (Illness Day 29, Hospital Day 22, Postoperation Day 21, Confirmation and Antiviral Therapy Day 10). Strip shadows in the lungs were visible, but which were significantly less than before.
Discussion
In this report, we presented the clinical course of a COVID-19 case in an AOSC patient. She had no other typical symptoms of COVID-19 such as cough, dyspnea, nausea, vomiting, abdominal pain and diarrhea except for fever, but her epidemiological history was clear. Under protection and isolation measures, after treatment with ERCP, EST and ENBD, jaundice caused by AOSC was relieved, but the patient had a fever again. SARS-CoV-2 viral nucleic acid testing and lungs CT scanning were performed repeatedly, and COVID-19 was eventually confirmed by the viral nucleic acid testing results, but the pulmonary CT imaging patterns had been atypical. After the patient was transferred to the Infection Department for antiviral treatment, her condition improved significantly without fever.
Although the patient had no other typical symptoms of COVID-19 except for fever when she came to the hospital, SARS-CoV-2 was spreading widely in Wuhan, China at that time, and the patient had been living in Wuhan. Accordingly, Pulmonary CT scanning and SARS-CoV-2 nucleic acid testing were performed to exclude COVID-19. The first lungs CT revealed high-density strip shadows in both lower lung, which were not typical CT patterns of COVID-19 pneumonia. The first viral nucleic acid testing result was also negative. However, the pathophysiological changes of AOSC can cause impaired immune function. In addition, the patient is older and has underlying health conditions. These adverse factors make this patient is more vulnerable to SARS-CoV-2 than the general population. Therefore, the patient could not be completely excluded as COVID-19, and was safely and prudently classified as a suspicious case. Isolation and protection measures were immediately taken to avoid nosocomial infections. Because the patient was critically ill, emergency endoscopy-related procedures were performed to relieve biliary obstruction. After the operation, the viral nucleic acid testing and chest CT scanning were repeated due to the recurrence of fever. It was not positive until the third viral nucleic acid testing, and the patient was finally confirmed as COVID-19. However, repeated chest CT had consistently shown no typical imaging patterns. This case gives clinicians a hint that patients’ epidemiological history should be highly valued, especially in patients with serious underlying diseases that may be more susceptible to SARS-CoV-2 infection.
The patient was admitted with jaundice and fever as the main clinical features. The fever subsided after the biliary obstruction was relieved, indicating that the patient's first fever was caused by a biliary infection. The SARS-CoV-2 nucleic acid positive result was confirmed rapidly after the recurrence of postoperative fever, and antiviral treatment was immediately given, suggesting that the patient's recurrent fever was caused by SARS-CoV-2 infection. Therefore, the absence of other typical COVID-19 symptoms in the course of the patient's disease may be due to timely antiviral treatment after the confirmation of SARS-CoV-2 infection.
SARS-CoV-2 nucleic acid detection, including real-time quantitative RT-PCR and gene sequencing, is the main means of confirming COVID-19. However, this method has a high incidence of false-negative results, usually requiring multiple sampling and repeated testing to confirm COVID-19. This is one of the reasons that the patient did not show a positive SARS-CoV-2 nucleic acid test until the third nasopharyngeal sampling. Of course, the negative results of the first two viral nucleic acid tests may also be that the patient is in the incubation period with a low SARS-CoV-2 viral RNA load.
Chest imaging, including X-ray and CT examination, is an important supplementary means to confirm COVID-19, especially for suspicious patients with negative viral nucleic acid test results. Previous studies have reported that during the progression of COVID-19, the chest CT scans of patients presented initially patchy shadows and interstitial changes, then developed into ground-glass opacities and infiltrates, and in severe cases even into pulmonary consolidation, but pleural effusion was rare [9], [10], [11], [12]. This patient has not shown the typical CT characteristics of COVID-19 pneumonia. It may be that early antiviral treatment blocked the pathological changes in the lungs. Chest CT showed high-density strip shadows of both lungs, which may be a secondary bacterial infection of lung injury caused by acute severe cholangitis.
Conclusions
In conclusion, we reported a case of COVID-19 with atypical presentations in an AOSC patient. The particularity of this COVID-19 case was the atypical clinical features and chest CT findings. Endoscopy-related procedures relieved the patient's biliary obstruction. Repeated viral nucleic acid testing confirmed SARS-CoV-2 infection. This particular case indicates that patients with COVID-19 may not exhibit typical clinical features and lung imaging findings, especially for patients receiving early antiviral therapy, and also reveals the importance of timely antiviral treatment after confirmation of SARS-CoV-2 infection.
Funding
This work was supported by the Zhejiang Provincial Natural Science Foundation of China (No. LGF19H290004).
Authors’ contributions
Lu-Lu Zhai and Feng Xiang: drafting and editing of manuscript, acquisition of data.
Wei Wang, Lun Wu, Ling Ye and Li-Chao Yao: editing of manuscript.
Zhi-Gang Tang: analysis and interpretation of data, revision of manuscript.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
We thank the patient; the nurses and clinicians who provided care for the patient; the medical staff in the Radiology, Laboratory, Pneumology, Infectious, and Prevention and Health Care Departments for their support; and all health workers in the fight against the epidemic.
References
- 1.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19):Situation Report–102. Accessed May 2, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200501-covid-19-sitrep.pdf?sfvrsn=742f4a18_2.
- 3.Centers for Disease Control and Prevention. Frequently asked questions about SARS. Accessed March 11 2020. https://www.cdc.gov/sars/about/faq.html.
- 4.World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV). Accessed March 11, 2020. https://www.who.int/emergencies/mers-cov/en
- 5.Xu X.W., Wu X.X., Jiang X.G., et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020:368. doi: 10.1136/bmj.m606. m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D., Hu B., Hu C., et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang W., Cao Q., Qin L., et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020 doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi H., Han X., Jiang N., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;24 doi: 10.1016/S1473-3099(20)3008. 6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei J., Xu H., Xiong J., et al. 2019 Novel Coronavirus (COVID-19) Pneumonia: Serial Computed Tomography Findings. Korean J Radiol. 2020 doi: 10.3348/kjr.2020.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ai T., Yang Z., Hou H., et al. Correlation of chest CT and RT-PCR testing in Coronavirus Disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]