Figure 4.
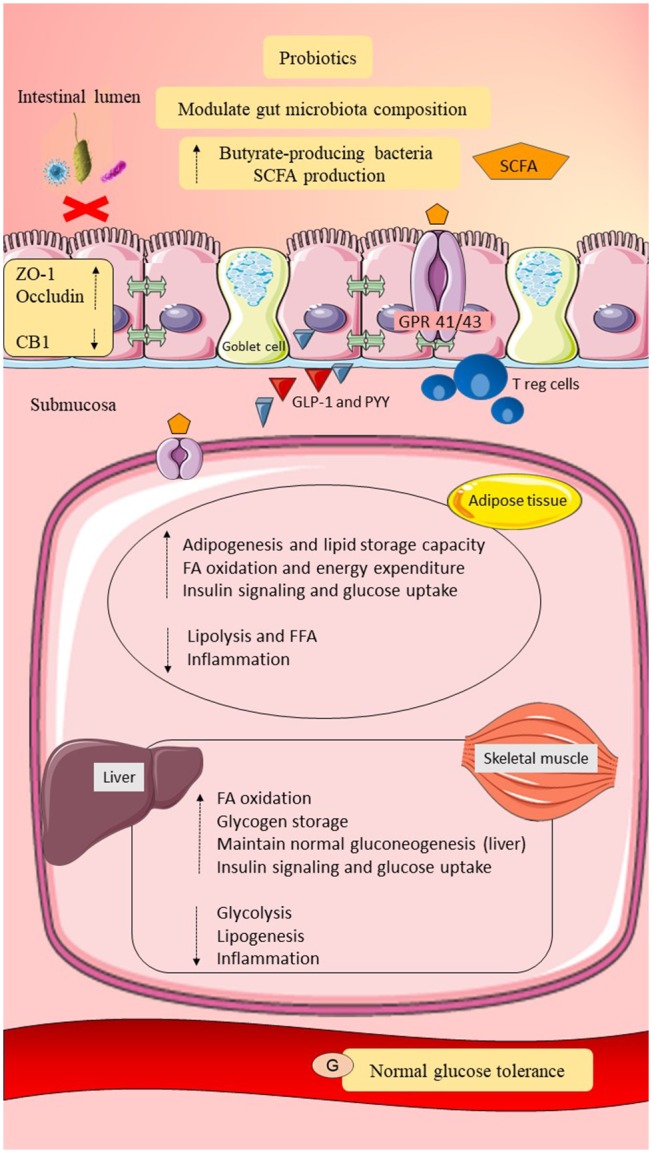
Possible roles of probiotics in post-GDM women. Probiotics may modulate gut microbiota composition by increasing the butyrate-producing gut microbiota and reducing the adherence of pathobionts to the gut epithelial mucosa. Elevation of butyrate-producing bacteria may improve dietary fermentation and promote SCFAs production. Probiotics may improve gut epithelial permeability by upregulating the expression of tight junction proteins (ZO-1 and occludin) and may downregulate CB1. Intact gut epithelial integrity with adequate mucosal layer and tight junctions may reduce pathobionts and LPS translocation and prevent metabolic endotoxemia. Probiotics may upregulate Treg cells and downregulate CD8+ T cells. Probiotics may also promote GLP-1 and PYY release. Moreover, probiotics may regulate lipid metabolism by maintaining adipogenesis, fatty acid oxidation, and suppression of lipolysis. Therefore, suppression of metabolic endotoxemia and adiposity, as well as elevation of GLP-1 and PYY, may increase insulin signaling and glucose uptake. Probiotics in an adequate amount may also regulate glucose metabolism by maintaining gluconeogenesis and promoting glycogen storage. In conclusion, probiotics may reduce systemic inflammation and improve lipid and glucose homeostasis in post-GDM women. SCFA, short-chain fatty acid; GPR 41/43, G-protein-linked receptor 41/43; CB1/2, cannabinoid receptor 1/2; ZO-1, zona occludens 1; Treg cells, regulatory T cells; GLP-1, glucagon like peptide-1; PYY, peptide YY; IL-1β, interleukin-1β; IL-6, interleukin-6; TNF-α, tumor necrosis factor-α; IR, insulin receptor; FFA, free fatty acid; G, glucose. Dashed lines indicate the possible effects of probiotics.
