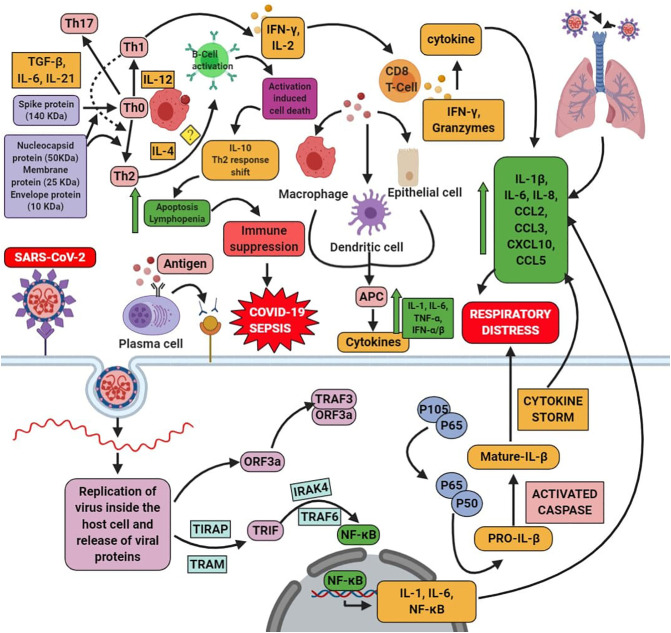
Fig. 2.
SARS-CoV-2 enters into the host cell via binding with the cellular receptor ACE-2. It undergoes the fusion with the joining of the plasma membrane and the virus. Then it undergoes the process of the proteolytic cleavage; further, it will undergo replication and lead to the formation of the proteins. This process activates the signaling pathway, such as the NF-kB pathway, via TRIF. The interaction between the cells and the virus activates many cytokine storms. On the other hand, once the virus enters into the cell, the antigen present in that would undergo the antigen presentation cells (APC); further, this stimulates the humoral and cellular immunity. COVID-19 infects the macrophage cells, which presents to the T cell, further, which leads to the activation, differentiation of T-cells, along with the production of cytokines. This shows the negative action on the activation of CD8 T cells. Thus the mediator produced by the CD8+ T cells clears the infection of SARS-CoV. Upon COVID-19 infection, there is a reduced CD4+ and CD8+ cell level, further increasing the cytokine level in the cells, which triggers the inflammation. This mediates the production of the cytokine storm via secreting chemokine and cytokines such as IL-1β, IL-6, TNF-α, IL-8, IL-21, CCL2, CCL3, CCL5, CXCL10, TNF-β, and MCP-1 and triggers the tissue injury. On the other hand, based on the weight of the protein of SARS-CoV2, there is an activation of Th1/Th17 (boosts immune system) when the spike protein is >70 kDa. In case of the Th2 (anti-inflammatory) is activated by the majority of the protein with <70 kDa, then the activation of the B-cell receptor, which causes activation-induced cell death such as apoptosis and lymphopenia which is by releasing IL-10, shifting of Th1 to Th2 immune response, suppression of the immune system and further leads to the COVID-19 sepsis. The role of IL-4 has not been elucidated yet. It remains unanswerable upon COVID-19 condition with the mechanism of Th2 and Th1/Th17.