Highlights
-
•
People with mental health conditions engage with health coaching phone services.
-
•
The prevalence and extent of some health risk behaviours is higher in this group.
-
•
Confidence in ability to change health risk behaviours is lower in this group.
Keywords: Preventive health services, Mental health, Chronic disease, Exercise, Diet, Health care quality, Access, Evaluation
Abstract
The NSW Get Healthy Service® (GHS) is a free telephone-based coaching service in NSW, Australia, which supports behaviour change around healthy eating and physical activity. The aims of this study were to 1) assess the proportion of coaching participants within GHS who report having had a mental health condition, and 2) describe and compare the health risk profiles and confidence for behaviour change of coaching participants with and without a mental health condition. Secondary data analysis was conducted on information collected via participant self-report as a part of the coaching process for 11,925 participants who enrolled in a GHS coaching program for the first time between January 2015 and December 2017. Twenty six percent (n = 3106) of participants reported having had a significant mental health condition that required treatment from a health professional. Participants who reported a mental health condition were significantly less likely (54%) to be meeting guidelines for physical activity than participants without a mental health condition (64%); more likely to be overweight/obese (89%) compared to those without (81%); and reported lower confidence for changing exercise, nutrition and weight. There were no significant differences in proportions meeting fruit or vegetable intake recommendations. People with a mental health condition represent approximately a quarter of GHS participants. This group of participants presented higher levels of health risks and expressed lower confidence in behaviour change than program participants without such a condition. Future service planning and development may consider this variation in participant profiles.
1. Introduction
A recent review suggests that globally 17.6% of the adult population experience a mental health condition during a 12 month period (Steel et al., 2014), and 18–36% do so at some point across their lifetime (Steel et al., 2014, Kessler et al., 2009), with similar rates suggested for Australia (Slade et al., 2009). Previous research undertaken with individuals diagnosed with a mental health condition suggests this population are likely to experience a significant reduction in life expectancy (Laursen et al., 2016, Druss et al., 2011, Walker et al., 2015, Lawrence et al., 2013). For example, in a Danish population-based cohort, individuals diagnosed with depression experienced up to 14 years reduced life expectancy (Laursen et al., 2016). A review of mortality among people with mental disorders found a reduction in life expectancy of up to 32 years, with 10 being the median years of life lost (Walker et al., 2015). In Australia, life expectancy differences have been estimated at a reduction of up to 16 years, with a large proportion (77%) of excess mortality attributed to chronic physical health conditions such as cardiovascular disease, diabetes and cancers (Lawrence et al., 2013).
A significant proportion of chronic disease burden can be attributed to health risk behaviours such as smoking, physical inactivity, poor nutrition and harmful alcohol consumption; contributing to half of the global disability adjusted life years in 2016 (GBD, 2016). These health risk behaviours are more prevalent among people with a mental health condition; and some sub-groups of the population are reported to experience a higher prevalence of both these health risk behaviours and mental health concerns. In Australia, such sub-groups include people of lower socioeconomic status, those living in rural and remote areas, Aboriginal and Torres Strait Islander people, and those from culturally and linguistically diverse backgrounds (Australian Institute of Health and Welfare, 2018). While global rates of smoking have declined in the last 20 years (World Health Organisation, 2015), this trend has not extended to people with a mental health condition, where smoking rates remain more than double that of the general population (Smith et al., 2014, Morris et al., 2014, Dierker and Donny, 2008, Lê Cook et al., 2014, Szatkowski and McNeill, 2014). A higher prevalence of physical inactivity was found in a sample of adults diagnosed with a mental health condition who had used community mental health services in the U.S. when compared to the general population (25.7% and 17.5% respectively, p < 0.01) (Daumit et al., 2005). Australian research from the National Health Survey similarly indicated a higher prevalence of physical inactivity among people with a mental health condition, as well as higher prevalence of harmful alcohol consumption (Harris et al., 2018).
The provision of health coaching is well established as being effective in supporting health behaviour change (Sforzo et al., 2017). The delivery of health coaching via telephone services represent a means to provide professionally-delivered and widely accessible behaviour change support (Zhu et al., 2002, Hollis et al., 2007, O’Hara et al., 2011). Quitlines for example provide personalised smoking cessation support at a population-level, and have been noted as being globally affordable (West et al., 2015) and effective (Hollis et al., 2007). In the U.S. (Vickerman et al., 2015) and Australia (Railton, 2015), studies suggest one half and one third of Quitline callers respectively, report a mental health condition, and that these individuals experience higher levels of nicotine dependence. Further, Quitlines are effective in facilitating cessation for smokers with a mental health condition, though sustained abstinence rates are somewhat lower when compared to Quitline participants without such a condition (Vickerman et al., 2015, Railton, 2015). An awareness of how service users with a mental health condition differ to those without highlights the potential for Quitlines, and other telephone delivered health coaching services, to develop tailored or more intensive treatments to achieve equivalent behaviour change outcomes (Vickerman et al., 2015, Tedeschi et al., 2016).
Research has indicated that telephone coaching support can also be effective for behaviours other than smoking, such as physical activity and nutrition (Goode et al., 2012), yet compared to smoking behaviours, there is currently limited population-level research that has explored the impact of telephone support services for these behaviours. In New South Wales (NSW), Australia, the Get Healthy Information and Coaching Service® (NSW Get Healthy Service®), is a free telephone coaching service providing support for healthy eating, physical activity, maintaining/achieving healthy weight and reducing alcohol consumption. Participants may be referred to this service by a health professional, or may self-refer either online or by phone. The NSW Get Healthy Service® engaged with approximately 5000 participants as a part of their coaching program in 2017, with enrolment rates increasing annually since service inception in 2009. A pre-post evaluation found that participants completing a 6 month coaching program improved their weight and waist circumference and increased vegetable consumption at 12 months following program completion, suggesting the service can be effective for the general population (O’Hara et al., 2013).
For people with a mental health condition, previous research indicates that telephone support for nutrition (Baker et al., 2014), physical activity (Baker et al., 2014, Lee et al., 2014) and weight (Temmingh et al., 2013) is feasible and acceptable. However, use of a population level service such as the NSW Get Healthy Service® has not been examined for this subgroup. Further, a comparison of characteristics of service users with and without a mental health conditions may usefully inform service planning and development.
The aim of the current study is therefore to assess the proportion of coaching participants undertaking the NSW Get Healthy Service® who report having had a mental health condition, and to describe and compare the health risk profiles, goals and confidence in behaviour change of coaching participants with and without a mental health condition.
2. Methods
2.1. Setting & design
Individuals over the age of 16 residing in the states of NSW or Queensland, or over 18 in South Australia, who are interested in eating a healthier diet, getting active, achieving or maintain a healthy weight, or reducing their alcohol consumption can self-refer to the NSW Get Healthy Service® via telephone or through the service’s website. Referrals are also received from a range of health professionals within and outside the public health system. Participants may choose to receive a single call and resources from the service (Information Only), or may opt to enrol in a coaching program. Participants who choose to enrol in a coaching program receive a minimum of 4 and up to 13 calls over a 6 month period, during which they are provided with behaviour change advice and support, most often from the same individual coach throughout. The average length of a coaching call is 15–20 min. Calls are delivered by university qualified health coaches (dietitians, exercise physiologists, nurses). Coaches receive training in motivational interviewing, focusing on working effectively with patients to promote: health literacy; shared and fully-informed decision-making; and evidence-based, goal-oriented treatment, self-management and health behaviours (Health Change Australia, 2020). During their first call with a coach, participants complete a health assessment with information collected around their current health behaviours, their health-related goals, as well as whether they have experienced a mental health condition. Participants are allocated to a module based on responses to the health assessment. A module is a series of up to 13 telephone calls, supporting health behaviour change in areas relevant to a participant’s goals through goal setting, identifying barriers and enablers, and problem solving from each participant’s perspective. They include support to eat healthily, increase physical activity, and/or achieve or maintain a healthy weight (Standard Get Healthy module, commenced February 2009), and may also have a focus on particular health concerns (Alcohol Reduction, commenced October 2015; Type 2 Diabetes Prevention module, commenced July 2013) or have been tailored for a portion of the population (Aboriginal and Torres Strait Islander module, commenced November 2012). The Get Healthy in Pregnancy module (commenced July 2015) focuses on gaining a healthy amount of weight during pregnancy as per Institute of Medicine guidelines (National Research Council, 2010).
A secondary data analysis was conducted on a de-identified, cross-sectional sample of data routinely collected as a part of registering with the service. Ethical approval was obtained from the University of Newcastle Human Research Ethics Committee, reference no: H-2016-0270.
2.2. Participants
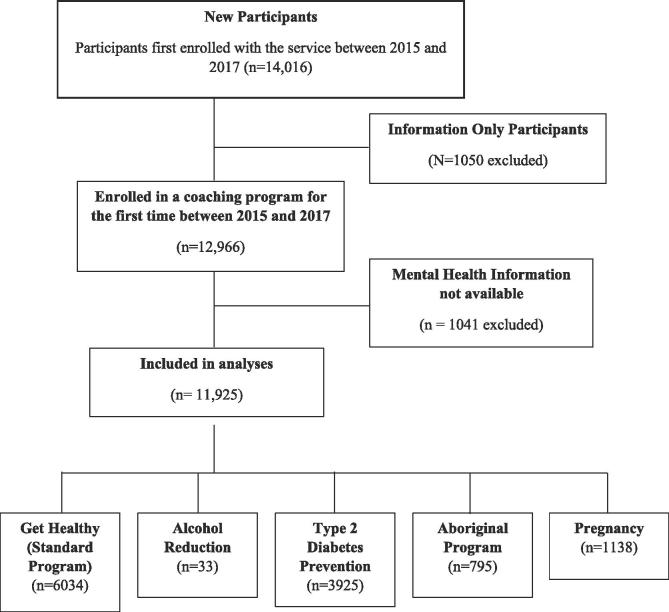
Data were obtained for all participants who made contact with the NSW Get Healthy Service® between January 2015 and December 2017 (n = 14,016) (Fig. 1). Of this, 1050 participants only ever enrolled in the Information Only module and were subsequently excluded. Of the potential 12,966 remaining participants for whom data was available for their first coaching experience within the study period, 1041 were removed due to information on mental health status not being provided, resulting in 11,925 participants with available data for analysis.
Fig. 1.
Data inclusion and module allocation all included participants have provided consent for their data to be analysed for research purposes.
2.3. Measures
2.3.1. Mental health status
One screening question as a part of the enrolment process asked participants “Have you had a significant mental health problem that required treatment from a health professional?”(Yes/No).
2.3.2. Demographics, service details, self-rated health and health goals
As a part of routine data collection, participants were asked to report their: date of birth, gender, Aboriginality, postcode, highest education level attained and current employment status. Postcode was used to determine geographic remoteness (Department of Health and Aged Care, 2001) and socio-economic index of disadvantage (BAustralian Bureau of Statistics, 2008). Data also included the module to which participants had been allocated. Participants indicated where they heard about the service (referral source), their perceived overall health (poor, fair, good, very good, excellent) and primary health goal (Healthy eating-, exercise-, weight- or waist circumference-related).
2.3.3. Health risks and confidence in behaviour change
As a part of the health assessment, participants indicated the frequency with which they engaged in health-related behaviours. Questions included previously used and validated measures of health behaviours, including the usual number of fruit and vegetable servings consumed per day (Rutishauser et al., 2001), the number of times per week they engaged in 30 min of walking, 30 min of moderate physical activity, and 20 min of vigorous physical activity (Smith et al., 2005), frequency of smoking tobacco products (Chen et al., 2010), as well as frequency and amount of alcohol consumption as measured via AUDIT (Babor et al., 2001) Self-reported weight, height and waist circumference were also recorded.
Participants indicated their perceived confidence in achieving behaviours relating to physical activity exercise, diet and weight. On a scale of 1–10, with 1 being not at all confident and 10 being very confident, participants identified how confident they felt in their ability to: do regular, moderate physical activity (such as walking, swimming or cycling) on most days of the week; change to healthier eating; or achieve a weight-related goal.
2.4. Statistical analysis
Data were analysed using SPSS (IBM) and descriptive statistics were used to summarise the representation of those with a mental health condition among the overall sample and for each GHS module (Proportion; 95% Confidence Interval). Referral sources were categorised as either general practitioner, other health professional, or any other source.
Health risk variables were created post-data collection in accordance with current Australian guidelines. Participants were considered to be at risk for fruit consumption if they consumed less than two serves daily, and for vegetable consumption if they consumed <5 serves daily (National Health & Medical Research Council, 2003). Physical activity risk was classified as not meeting current guidelines (Department of Health, 2014) of 150 min of light (walking) to moderate activity, 75 min of vigorous activity, or a combination of the two, each week. In accordance with guidelines, smoking risk was determined as any current tobacco smoking (daily, occasionally) (Ministerial Council on Drug Strategy, 2004), and alcohol consumption risk was assigned for AUDIT scores of >8 (Babor et al., 2001). Waist circumference risk was considered >80 cm for women and >94 cm for men (World Health Organization, 2000). Body Mass Index (BMI) was calculated using reported height and weight, with a score of 25+ (overweight/obese) considered at risk (World Health Organization, 2000).
Comparison of groups was based on responses to having had a mental health condition (Yes, No). For demographics, service details, primary health goal and self-rated health variables (Table 1), chi-squared analyses were conducted to compare the groups for categorical variables and a t-test to compare mean age (p < 0.01 to allow for multiple comparisons).
Table 1.
Demographic, service details, self-rated health and health-related goals by presence of a mental health condition (MHC).
| All (N = 11,925) |
No MHC (N = 8819) |
MHC (N = 3106) |
P | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Demographics | |||||||
| Age | N = 11,920 | N = 8814 | N = 3106 | ||||
| Under 18 | 27 | 0.2 | 21 | 0.2 | 6 | 0.2 | 0.000 |
| 18–39 | 4229 | 35.5 | 3210 | 36.4 | 1019 | 32.8 | |
| 40–59 | 4707 | 39.5 | 3312 | 37.6 | 1395 | 44.9 | |
| 60+ | 2957 | 24.8 | 2271 | 25.8 | 686 | 22.1 | |
| Mean age (SD) | 47.9 (15.8) | 47.9 (16.0) | 47.6 (14.8) | 0.405 | |||
| Gender | N = 11,924 | N = 8818 | N = 3106 | ||||
| Male | 2721 | 22.8 | 2057 | 23.3 | 664 | 21.4 | 0.028 |
| Female | 9203 | 77.2 | 6761 | 76.7 | 2442 | 78.6 | |
| Aboriginal or torres strait Islander | N = 11,146 | N = 8263 | N = 2883 | ||||
| Yes | 892 | 8.0 | 600 | 7.3 | 292 | 10.1 | 0.000 |
| Education | N = 11,158 | N = 8271 | N = 2887 | ||||
| High school or less | 4182 | 37.5 | 2945 | 35.6 | 1237 | 42.8 | 0.000 |
| Vocationala | 3418 | 30.6 | 2463 | 29.8 | 955 | 33.1 | |
| Undergraduate | 2664 | 23.9 | 2110 | 25.5 | 554 | 19.2 | |
| Postgraduate | 894 | 8.0 | 753 | 9.1 | 141 | 4.9 | |
| Employment | N = 11,110 | N = 8239 | N = 2871 | ||||
| Unemployed | 1317 | 11.8 | 768 | 9.3 | 549 | 19.1 | 0.000 |
| Employedb | 6243 | 56.2 | 4936 | 59.9 | 1307 | 45.5 | |
| Retired/Home duties | 2629 | 23.7 | 1981 | 24.1 | 648 | 22.6 | |
| Other | 921 | 8.3 | 554 | 6.7 | 367 | 12.8 | |
| Geographic location | N = 11,908 | N = 8807 | N = 3101 | ||||
| Major cities | 8100 | 68.0 | 6051 | 68.7 | 2049 | 66.1 | 0.007 |
| Regional/Rural | 3808 | 32.0 | 2756 | 31.3 | 1052 | 33.9 | |
| Index of disadvantage | N = 11,864 | N = 8780 | N = 3084 | ||||
| 1st Quintile | 2234 | 18.8 | 1702 | 19.4 | 532 | 17.3 | 0.132 |
| 2nd Quintile | 1286 | 10.8 | 943 | 10.7 | 343 | 11.1 | |
| 3rd Quintile | 2616 | 22.0 | 1923 | 21.9 | 693 | 22.5 | |
| 4th Quintile | 3143 | 26.5 | 2303 | 26.2 | 840 | 27.2 | |
| 5th Quintile | 2585 | 21.8 | 1909 | 21.7 | 676 | 21.9 | |
| Service details | |||||||
| Referral source | N = 11,312 | N = 8330 | N = 2982 | ||||
| General Practitioner | 884 | 7.8 | 635 | 7.6 | 249 | 8.4 | 0.166 |
| Other Health Professionalc | 4028 | 35.6 | 2906 | 34.9 | 1122 | 37.6 | |
| Otherd | 6400 | 56.6 | 4789 | 57.5 | 1611 | 54.0 | |
| Module | N = 11,925 | N = 8819 | N = 3106 | ||||
| Get Healthy (Standard Program) | 6034 | 50.6 | 4490 | 50.9 | 1544 | 49.7 | 0.000 |
| Diabetes Prevention | 3925 | 32.9 | 2834 | 32.1 | 1091 | 35.1 | |
| Aboriginal Strategy | 795 | 6.7 | 539 | 6.1 | 256 | 8.2 | |
| Pregnancy | 1138 | 9.5 | 934 | 10.6 | 204 | 6.6 | |
| Alcohol | 33 | 0.3 | 22 | 0.2 | 11 | 0.4 | |
| Health rating and goals | |||||||
| Self-rated heath | N = 8265 | N = 6241 | N = 2024 | ||||
| Excellent | 370 | 4.5 | 325 | 5.2 | 45 | 2.2 | 0.000 |
| Very good | 1526 | 18.5 | 1268 | 20.3 | 258 | 12.7 | |
| Good | 3757 | 45.5 | 2986 | 47.8 | 771 | 38.1 | |
| Fair | 1865 | 22.6 | 1237 | 19.8 | 628 | 31.0 | |
| Poor | 747 | 9.0 | 425 | 6.8 | 322 | 15.9 | |
| Primary health goal | N = 9510 | N = 7174 | N = 2336 | ||||
| Weight | 6251 | 65.7 | 4633 | 65.0 | 1588 | 68.0 | 0.035 |
| Waist Circumference | 379 | 4.0 | 292 | 4.1 | 87 | 3.7 | |
| Exercise | 1169 | 12.3 | 886 | 12.4 | 283 | 12.1 | |
| Healthy eating | 1711 | 18.0 | 1333 | 18.6 | 378 | 16.2 | |
Vocational includes Trade Certificate, Certificate II, Associate Diploma and Advanced Diploma.
Employed includes part time, full time and casual employment.
Examples of Other Health Professionals include Mental Health Services, Aboriginal Community Health Services and Pharmacies.
Examples of Other referral sources include Media, workplaces, family/friends and health campaigns.
For health risks (at risk/not at risk), groups were compared for each of the five behaviours (fruit consumption, vegetable consumption, physical activity, smoking and alcohol consumption), waist circumference and BMI (7 variables, Table 2). Logistic regression accounting for age, gender and education were conducted to determine any differences between those with and without a mental health condition on each of the seven risk variables (adjusted odds ratios; p < 0.01 to allow for multiple comparisons) and multiple linear regression accounting for the same demographic variables was conducted on continuous formats of the risk variables plus three confidence in behaviour change variables (Table 3).
Table 2.
Proportion of sample ‘at risk’ for health behaviours by presence of a mental health condition (MHC).
| All (N = 11,925) | No MHC (N = 8819) | MHC (N = 3106) | AOR (95% CI)a | p | ||||
|---|---|---|---|---|---|---|---|---|
| n/N | % | n/N | % | n/N | % | |||
| Nutrition | ||||||||
| Fruit – At Risk | 4237/8468 | 50.0 | 3144/6393 | 49.2 | 1093/2075 | 52.6 | 1.11 (1.00–1.24) | 0.047 |
| Vegetable – At Risk | 7426/8462 | 87.8 | 5575/6387 | 87.3 | 1851/2075 | 89.2 | 1.18 (1.00–1.40) | 0.046 |
| Physical activity | ||||||||
| Physical Activity – At Risk | 4771/8509 | 56.1 | 3452/6421 | 53.8 | 1319/2088 | 63.2 | 1.45 (1.30–1.61) | 0.000 |
| Smoking | ||||||||
| Smoking – At Risk | 723/8476 | 8.5 | 430/6388 | 6.7 | 293/2088 | 14 | 2.03 (1.72–2.40) | 0.000 |
| Alcohol | ||||||||
| AUDIT – At Risk | 231/5432 | 4.3 | 148/4052 | 3.7 | 83/1380 | 6.0 | 1.57 (1.17–2.10) | 0.002 |
| Waist circumference | ||||||||
| Waist Circumference – At Risk | 6176/6905 | 89.4 | 4603/5211 | 88.3 | 1573/1694 | 92.9 | 1.63 (1.31–2.03) | 0.000 |
| Body mass index | N = 3945 | N = 2957 | N = 988 | |||||
| Underweight/Acceptable (<24.99) | 686 | 17.4 | 574 | 19.4 | 112 | 11.3 | 1.63 (1.29–2.06)c | 0.000 |
| Overweight (25–29.99)b | 1171 | 29.7 | 931 | 31.5 | 240 | 24.3 | ||
| Obese (30 + ) b | 2088 | 52.9 | 1452 | 49.1 | 636 | 64.4 | ||
Adjusted Odds Ratio after accounting for Age, Gender and Education.
Considered at risk for BMI.
Odds of being at risk.
Table 3.
Engagement in health behaviours and confidence in behaviour change by presence of a mental health condition (MHC).
| All (N = 11,925) |
No MHC (N = 8819) |
MHC (N = 3106) |
βa | p | ||||
|---|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | n | Mean (SD) | |||
| Nutrition | ||||||||
| Fruit serves daily | 8468 | 1.55 (1.31) | 6393 | 1.58(1.31) | 2075 | 1.46 (1.36) | −0.04 | 0.001 |
| Vegetable serves daily | 8462 | 2.49 (1.71) | 6387 | 2.55(1.68) | 2075 | 2.31 (1.80) | −0.06 | 0.000 |
| Physical activity | ||||||||
| PA Vigorousb | 8517 | 0.39 (1.18) | 6427 | 0.43(1.22) | 2090 | 0.29 (1.01) | −0.05 | 0.000 |
| PA Moderatec | 8525 | 1.01 (1.85) | 6434 | 1.06 (1.89) | 2091 | 0.88 (1.74) | −0.04 | 0.000 |
| PA Walkingc | 8523 | 2.79 (2.80) | 6431 | 2.90 (2.80) | 2092 | 2.45 (2.76) | −0.07 | 0.000 |
| Weight | ||||||||
| Weight (kg) | 8917 | 87.56 (22.39) | 6745 | 85.86 (21.62) | 2172 | 92.81 (23.87) | 0.130 | 0.000 |
| Waist circumference | ||||||||
| Waist Circumference (cms) – Men Only | 1799 | 108.26 (18.96) | 1383 | 106.86 (18.17) | 396 | 113.11 (20.76) | 0.095 | 0.000 |
| Waist Circumference (cms) – Women Only | 5126 | 101.07 (16.77) | 3828 | 99.58 (16.31) | 1298 | 105.44 (17.34) | 0.149 | 0.000 |
| BMI | ||||||||
| BMI | 3945 | 31.69 (7.65) | 2957 | 31.01 (7.30) | 988 | 33.73 (8.30) | 0.14 | 0.000 |
| Confidence in behaviour change | ||||||||
| Exercise | 6188 | 7.07 (1.93) | 4650 | 7.15 (1.89) | 1538 | 6.82 (2.05) | −0.08 | 0.000 |
| Diet | 6239 | 7.14 (1.74) | 4729 | 7.22 (1.70) | 1510 | 6.90 (1.83) | −0.09 | 0.000 0.000 |
| Weight | 5397 | 6.89 (1.97) | 4082 | 6.99 (1.93) | 1315 | 6.59 (2.07) | −0.09 | |
Standardised co-efficient of mental health condition after accounting for age, gender and education.
Number of 20 min sessions per week.
Number of 30 min sessions per week.
3. Results
3.1. Proportion of participants with a mental health condition
Of the 11,925 participants who enrolled in a coaching program between January 2015 and December 2017, 26% (n = 3106, 95% CI 25.2−26.8%) identified as having had a mental health condition. The proportion of participants with a mental health condition enrolled in each module were as follows: Standard 25.6% (1544/6034, 95% CI 24.5–26.7%); Type 2 Diabetes Prevention 27.8% (1091/3925, 95% CI 26.4−29.2%); Aboriginal and Torres Strait Islander 32.2% (256/795, 95% CI 30.0−35.4%); Pregnancy 17.9% (204/1138, 95% CI 15.7−20.1%); and Alcohol Reduction 33.3% (11/33, 95% CI 17.2−49.4%).
3.2. Demographics, service details, self-rated health and health goals
The mean age of participants did not differ between groups, however examining age as a categorical variable indicated that a larger proportion of participants with a mental health condition were between 40 and 59 years old (Table 1). There was greater representation of people residing in regional or rural areas and those who identified as being of Aboriginal or Torres Strait Islander heritage. Coaching participants with a mental health condition were more likely to have an education of high school or less and to be unemployed. Almost three quarters (73.3%) of coaching participants without a mental health condition self-rated their health positively (excellent, very good or good), compared to just over half (53%) of coaching participants with a mental health condition. Approximately two thirds of participants in both groups indicated that their primary health goal was weight-related.
3.3. Health risks and confidence in behaviour change
Coaching participants with a mental health condition were significantly less likely to be achieving recommended levels of physical activity (Table 2). They were twice as likely to be daily or occasional smokers as those without a mental health condition (14% and 6.7%, respectively, p < .001), 1.67 times as likely to be at risk for harmful alcohol consumption based on AUDIT scores (6% and 3.7%, respectively, p = .002), and 1.63 times more likely to be at risk for waist circumference (p < .001) and for BMI (P.001). There was no significant difference between groups for fruit or vegetable consumption.
For analysis based on health risk variables treated as continuous measures, those with a mental health condition reported higher risk on all variables (Table 3). On average, women a mental health condition reported a waist circumference of 25 cm over the recommended level of 80 cm, while men report 19 cm over the recommended 94 cm. These measurements are greater than those of callers without a mental health condition, with women exceeding risk measurements by 19 cm on average, and men exceeding by 13 cm (p < .001 for both men and women). Participants with a mental health condition on average entered the program 7kgs heavier than participants without (p < .001), and were less confident in their ability to regularly exercise (p < .001), adjust their diet (p < .001), and achieve weight-related goals (p < .001).
4. Discussion
Based on routinely collected service information, 26% of participants who enrolled in a telephone-based coaching program to improve nutrition and physical activity self-reported having had a mental health condition. No significant differences were seen between service users with and without a mental health condition in terms of proportion at risk for fruit consumption, vegetable consumption, and primary health goal, however participants with a mental health condition rated their health as poorer, and were more likely to be at risk for physical activity, alcohol consumption, smoking, waist circumference and BMI. Similar trends can be seen when examining health measures in a continuous format, however considerations should be made around the practical interpretations of differences between groups in some measures, such as fruit and vegetable consumption, which although statistically significant, were very small.
The proportion of coaching participants engaging with the NSW Get Healthy Service® that report having had a mental health condition is consistent with estimates of the prevalence of mental health conditions measured in previous Australian national surveys (Slade et al., 2009), and similar to enrolment rates seen in an Australian telephone service for smoking cessation (Railton, 2015), suggesting that individuals with mental health conditions are seeking support to improve their physical health behaviours. Within the Aboriginal module a higher proportion of participants reported having a mental health condition. This may reflect the known challenges for this population, and is consistent with national survey data indicating higher levels of psychological distress reported by Indigenous Australians as compared to non-Indigenous Australians (Australian Institute of Health and Welfare, 2018), and also with Australian Quitline data reflecting a greater likelihood of having received mental health treatment among Indigenous callers (Cosh et al., 2013). This further emphasises the ongoing need for the NSW Get Healthy Service® to tailor the Aboriginal module to meet the specific cultural and clinical needs of this population and to optimise its delivery for those taking part (Quinn et al., 2017).
The increased prevalence of health risk is also consistent with previous research comparing individuals with specific mental health conditions to those without (Payne et al., 2012), and with the general population (Daumit et al., 2005). Participants with a mental health condition not only reported greater health risk, but also less confidence in changing health behaviour. Low confidence may inhibit engagement in behaviours such as physical activity (Marcus et al., 1992) and smoking cessation (Gwaltney et al., 2009) however, participation in programs facilitating positive health behaviours can also increase health-related self-efficacy (Yarborough et al., 2015, Clark et al., 2015), drawing attention to not only the benefits of connecting individuals with a mental health condition to health lifestyle programs, but also the importance of ensuring that such programs are effective in creating health behaviour change and increasing health-related self-efficacy.
No differences were seen in referral sources for coaching participants with and without a mental health condition, with approximately half of participants indicating that they had heard of or been directed to the service from sources other than a health professional. It has been suggested that behaviour change outcomes following telephone service use such as Quitlines is greater from active referrals, such as through health professionals, compared to passive or self-referrals (Guy et al., 2012). Active referrals to the NSW Get Healthy Service® through sources such as mental health services (Fehily et al., 2017) therefore present as an avenue for further consideration in the education and promotion of services to address client health risk behaviours. Similarly, the increased proportion of this group of participants residing outside of major cities, along with the increase in health risk among rural residents (Australian Institute of Health and Welfare, 2016), highlights the importance of easily accessible health support services such as the NSW Get Healthy Service® and the potential for further referrals and support to be made for individuals living in remote areas.
Although the precision of mental health status in this sample is constrained by routine service data collection, the findings still indicate a substantial health risk difference between service users identifying having had a mental health condition and those who did not; and also highlights the benefits of fostering opportunities for collaboration between health services and researchers. Such collaborations allow for greater evaluation potential within health services, but also better quality of evidence in research. It should be noted that the impact of medications on a participant’s ability to make changes to heath behaviours or biomedical measures was not considered, and that all measures were limited to self-report. However, it has been suggested that self-report of health measures via telephone presents an underestimation of health risk (Taylor et al., 2006), with a validation study of the NSW Get Healthy Service® participant population finding self-reported weight on average 1.6kgs lower than when objectively measured (O’Hara et al., 2013), making the current data likely to be a conservative estimate. As this data includes residents in one Australian state, the generalisability of these findings in both a national and international context is also unknown.
Further research is required regarding the interaction and engagement of people with a mental health condition with behaviour change telephone support services for health behaviours other than smoking. At present, it is unclear if this group of service users perceive telephone-based coaching services to be useful and/or meeting their needs, if they encounter any unique difficulties in connecting with such services, as well as whether these services are equally effective in achieving and sustaining behaviour change across all participants. Suggestions have been made to tailor Quitlines around monitoring the withdrawal symptoms and medication side effects during the quit process (Segan et al., 2017), as well as providing more intensive counselling (Vickerman et al., 2015) over more frequent and shorter calls (Morris et al., 2009) in order to improve outcomes for service users with a mental health condition. Such information could be useful in considering whether program modifications or further staff training around mental health, could be beneficial for both this subgroup and service providers.
5. Conclusion
The present study contributes to the limited literature on the representation of individuals with a mental health condition using telephone-based coaching services to address health risk behaviours. A significant proportion of coaching participants within the NSW Get Healthy Service® reported having a mental health condition, with those participants more likely to be at risk for multiple health measures compared to participants without a mental health condition. Additionally, coaching participants with a mental health condition experienced lower confidence in their ability to engage in health risk behaviour change. Findings require confirmation through a larger, generalizable sample, however may identify a need for service providers and researchers to consider potential differences in the risk profiles of individuals with a mental health condition. Such considerations could inform future service planning and development to meet the needs of such service users.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Tegan Bradley: Conceptualization, Formal analysis, Writing - original draft, Writing - review & editing. Kate Bartlem: Conceptualization, Writing - review & editing, Supervision. Elizabeth Campbell: Conceptualization, Writing - review & editing, Supervision. Paula Wye: Conceptualization, Writing - review & editing, Supervision. Chris Rissel: Resources, Writing - review & editing. Kate Reid: Resources, Writing - review & editing. Timothy Regan: Formal analysis, Writing - review & editing. Jacqueline Bailey: Formal analysis, Writing - review & editing. Jenny Bowman: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Tegan Bradley, Email: Tegan.Bradley@uon.edu.au.
Kate Bartlem, Email: Kate.Bartlem@newcastle.edu.au.
Elizabeth Campbell, Email: Libby.Campbell@hnehealth.nsw.gov.au.
Paula Wye, Email: Paula.Wye@newcastle.edu.au.
Chris Rissel, Email: Chris.Rissel@health.nsw.gov.au.
Kate Reid, Email: Kate.Reid2@health.nsw.gov.au.
Timothy Regan, Email: Timothy.Regan@uon.edu.au.
Jacqueline Bailey, Email: Jacqueline.m.Bailey@uon.edu.au.
Jenny Bowman, Email: Jenny.Bowman@newcastle.edu.au.
References
- Steel Z., Marnane C., Iranpour C. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014;43(2):476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Aguilar-Gaxiola S., Alonso J. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol. Psychiatric Sci. 2009;18(1):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Johnston A., Oakley Browne M.A., Andrews G., Whiteford H. 2007 national survey of mental health and wellbeing: methods and key findings. Aust. N. Z. J. Psychiatry. 2009;43(7):594–605. doi: 10.1080/00048670902970882. [DOI] [PubMed] [Google Scholar]
- Laursen T.M., Musliner K.L., Benros M.E., Vestergaard M., Munk-Olsen T. Mortality and life expectancy in persons with severe unipolar depression. J. Affect. Disord. 2016;193:203–207. doi: 10.1016/j.jad.2015.12.067. [DOI] [PubMed] [Google Scholar]
- Druss B.G., Zhao L., Von Esenwein S., Morrato E.H., Marcus S.C. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med. Care. 2011;599–604 doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D., Hancock K.J., Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ. 2013;346 doi: 10.1136/bmj.f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare 2018. Australia’s health 2018. Australia’s health series no. 16. AUS 221. Canberra: AIHW.
- World Health Organisation. WHO global report on trends in prevalence of tobacco smoking. 2015.
- Smith P.H., Mazure C.M., McKee S.A. Smoking and mental illness in the US population. Tobacco Control. 2014;23(e2):e147–e153. doi: 10.1136/tobaccocontrol-2013-051466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris C.D., Burns E.K., Waxmonsky J.A., Levinson A.H. Smoking cessation behaviors among persons with psychiatric diagnoses: results from a population-level state survey. Drug Alcohol Depend. 2014;136:63–68. doi: 10.1016/j.drugalcdep.2013.12.010. [DOI] [PubMed] [Google Scholar]
- Dierker L., Donny E. The role of psychiatric disorders in the relationship between cigarette smoking and DSM-IV nicotine dependence among young adults. Nicotine Tob. Res. 2008;10(3):439–446. doi: 10.1080/14622200801901898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê Cook B., Wayne G.F., Kafali E.N., Liu Z., Shu C., Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311(2):172–182. doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szatkowski L., McNeill A. Diverging trends in smoking behaviors according to mental health status. Nicotine Tob. Res. 2014;17(3):356–360. doi: 10.1093/ntr/ntu173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumit G.L., Goldberg R.W., Anthony C. Physical activity patterns in adults with severe mental illness. J. Nerv. Ment. Dis. 2005;193(10):641–646. doi: 10.1097/01.nmd.0000180737.85895.60. [DOI] [PubMed] [Google Scholar]
- Harris B, Duggan, M, Batterham, P, Bartlem, K, Clinton-McHarg, T, Dunbar, J, Fehily, C, Lawrence, D, Morgan, M & Rosenbaum, S,. Australia's Mental and Physical Health Tracker: Background Paper. 2018.
- Sforzo G.A., Kaye M.P., Todorova I. Compendium of the health and wellness coaching literature. Am. J. Lifestyle Med. 2017;12(6):436–447. doi: 10.1177/1559827617708562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S.-H., Anderson C.M., Tedeschi G.J. Evidence of real-world effectiveness of a telephone quitline for smokers. N. Engl. J. Med. 2002;347(14):1087–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- Hollis J.F., McAfee T.A., Fellows J.L., Zbikowski S.M., Stark M., Riedlinger K. The effectiveness and cost effectiveness of telephone counselling and the nicotine patch in a state tobacco quitline. Tobacco Control. 2007;16(Suppl 1):i53–i59. doi: 10.1136/tc.2006.019794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara B.J., Phongsavan P., Venugopal K., Bauman A.E. Characteristics of participants in Australia’s Get Healthy telephone-based lifestyle information and coaching service: reaching disadvantaged communities and those most at need. Health Educ. Res. 2011;26(6):1097–1106. doi: 10.1093/her/cyr091. [DOI] [PubMed] [Google Scholar]
- West R., Raw M., McNeill A. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Addiction. 2015;110(9):1388–1403. doi: 10.1111/add.12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickerman K.A., Schauer G.L., Malarcher A.M., Zhang L., Mowery P., Nash C.M. Quitline use and outcomes among callers with and without mental health conditions: a 7-month follow-up evaluation in three states. Biomed Res. Int. 2015 doi: 10.1155/2015/817298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Railton RS, C. 2013–2014 Evaluation of the Victorian Quitline. Cancer Council Victoria. Cancer Council Victoria,. 2015.
- Tedeschi G.J., Cummins S.E., Anderson C.M., Anthenelli R.M., Zhuang Y.-L., Zhu S.-H. Smokers with self-reported mental health conditions: a case for screening in the context of tobacco cessation services. PLoS ONE. 2016;11(7) doi: 10.1371/journal.pone.0159127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode A.D., Reeves M.M., Eakin E.G. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am. J. Prev. Med. 2012;42(1):81–88. doi: 10.1016/j.amepre.2011.08.025. [DOI] [PubMed] [Google Scholar]
- O’Hara B.J., Phongsavan P., Eakin E.G. Effectiveness of Australia’s Get Healthy information and coaching service®: maintenance of self-reported anthropometric and behavioural changes after program completion. BMC Public Health. 2013;13(1):175. doi: 10.1186/1471-2458-13-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker A.L., Turner A., Kelly P.J. ‘Better Health Choices’ by telephone: a feasibility trial of improving diet and physical activity in people diagnosed with psychotic disorders. Psychiatry Res. 2014;220(1):63–70. doi: 10.1016/j.psychres.2014.06.035. [DOI] [PubMed] [Google Scholar]
- Lee H., Kane I., Brar J., Sereika S. Telephone-delivered physical activity intervention for individuals with serious mental illness: A feasibility study. J. Am. Psychiatric Nurses Assoc. 2014;20(6):389–397. doi: 10.1177/1078390314561497. [DOI] [PubMed] [Google Scholar]
- Temmingh H., Claassen A., van Zyl S. The evaluation of a telephonic wellness coaching intervention for weight reduction and wellness improvement in a community-based cohort of persons with serious mental illness. J. Nerv. Ment. Dis. 2013;201(11):977–986. doi: 10.1097/NMD.0000000000000036. [DOI] [PubMed] [Google Scholar]
- Health Change Australia. Health Change® Methodology http://www.healthchange.com/About_HealthChange_Methodology. Published 2020. Accessed.
- National Research Council . National Academies Press; 2010. Weight Gain During Pregnancy: Reexamining the Guidelines. [PubMed] [Google Scholar]
- Department of Health and Aged Care. Measuring Remoteness: Accessibility/Remoteness Index of Australia (ARIA). Occasional Papers: New Series Number 14. Canberra: Commonwealth of Australia. 2001.
- Australian Bureau of Statistics. SEIFA: Socio-economic indexes for areas. . 2008.
- Rutishauser I., Webb K., Abraham B., Allsopp R. Australian Government Department of Health and Ageing; Canberra: 2001. Evaluation of Short Dietary Questions from the 1995 National Nutrition Survey. [Google Scholar]
- Smith B.J., Marshall A.L., Huang N. Screening for physical activity in family practice: evaluation of two brief assessment tools. Am. J. Prev. Med. 2005;29(4):256–264. doi: 10.1016/j.amepre.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Chen L., Magliano D.J., Balkau B. AUSDRISK: an australian type 2 diabetes risk assessment tool based on demographic, lifestyle and simple anthropometric measures. Med. J. Aust. 2010;192(4):197–202. doi: 10.5694/j.1326-5377.2010.tb03507.x. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, Organization WH. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. 2001.
- IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.
- National Health & Medical Research Council . Commonwealth Department of Health and Ageing; Canberra: 2003. Dietary guidelines for Australian adults. [Google Scholar]
- Department of Health . Australian Government; In. Canberra: 2014. Australia's Physical Activity and Sedentary Behaviour guidelines for Adults (18–64 years) [Google Scholar]
- Ministerial Council on Drug Strategy . Commonwealth of Australia; Canberra: 2004. National Tobacco Strategy, 2004–2009: The Strategy. [Google Scholar]
- World Health Organization. Obesity: preventing and managing the global epidemic (2000). Report of a WHO consultation. WHO technical report series 894. Geneva. [PubMed]
- Cosh S., Maksimovic L., Ettridge K., Copley D., Bowden J.A. Aboriginal and Torres Strait Islander utilisation of the Quitline service for smoking cessation in South Australia. Austr. J. Primary Health. 2013;19(2):113–118. doi: 10.1071/PY11152. [DOI] [PubMed] [Google Scholar]
- Quinn E., O’Hara B.J., Ahmed N. Enhancing the get healthy information and coaching service for Aboriginal adults: evaluation of the process and impact of the program. Int. J. Equity Health. 2017;16(1):168. doi: 10.1186/s12939-017-0641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne M.E., Steck S.E., George R.R., Steffens D.C. Fruit, vegetable, and antioxidant intakes are lower in older adults with depression. J. Acad. Nutr. Dietetics. 2012;112(12):2022–2027. doi: 10.1016/j.jand.2012.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus B.H., Selby V.C., Niaura R.S., Rossi J.S. Self-efficacy and the stages of exercise behavior change. Res. Q. Exerc. Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- Gwaltney C.J., Metrik J., Kahler C.W., Shiffman S. Self-efficacy and smoking cessation: a meta-analysis. Psychol. Addict. Behav. 2009;23(1):56. doi: 10.1037/a0013529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarborough B.J.H., Leo M.C., Yarborough M.T. Improvement in body image, perceived health, and health-related self-efficacy among people with serious mental illness: the STRIDE study. Psychiatric Serv. 2015;67(3):296–301. doi: 10.1176/appi.ps.201400535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A., Bezyak J., Testerman N. Individuals with severe mental illnesses have improved eating behaviors and cooking skills after attending a 6-week nutrition cooking class. Psychiatr. Rehabil. J. 2015;38(3):276. doi: 10.1037/prj0000112. [DOI] [PubMed] [Google Scholar]
- Guy M.C., Seltzer R.G., Cameron M., Pugmire J., Michael S., Leischow S.J. Relationship between smokers' modes of entry into quitlines and treatment outcomes. Am. J. Health Behav. 2012;36(1):3–11. doi: 10.5993/ajhb.36.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehily C., Bartlem K., Wiggers J. Evaluating the effectiveness of a healthy lifestyle clinician in addressing the chronic disease risk behaviours of community mental health clients: study protocol for a randomised controlled trial. Trials. 2017;18(1):276. doi: 10.1186/s13063-017-2017-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare. Australia’s health 2016. Australia’s health series no. 15. Cat. no. AUS 199. Canberra: AIHW.
- Taylor A.W., Grande E.D., Gill T.K. How valid are self-reported height and weight? A comparison between CATI self-report and clinic measurements using a large cohort study. Aust. N. Z. J. Public Health. 2006;30(3):238–246. doi: 10.1111/j.1467-842x.2006.tb00864.x. [DOI] [PubMed] [Google Scholar]
- Segan C.J., Baker A.L., Turner A., Williams J.M. Nicotine withdrawal, relapse of mental illness, or medication side-effect? Implementing a monitoring tool for people with mental illness into quitline counseling. J. Dual Diagnosis. 2017;13(1):60–66. doi: 10.1080/15504263.2016.1276657. [DOI] [PubMed] [Google Scholar]
- Morris C.D., Tedeschi G.J., Waxmonsky J.A., May M., Giese A.A. Tobacco quitlines and persons with mental illnesses: perspective, practice, and direction. J. Am. Psychiatric Nurses Assoc. 2009;15(1):32–40. doi: 10.1177/1078390308330050. [DOI] [PubMed] [Google Scholar]