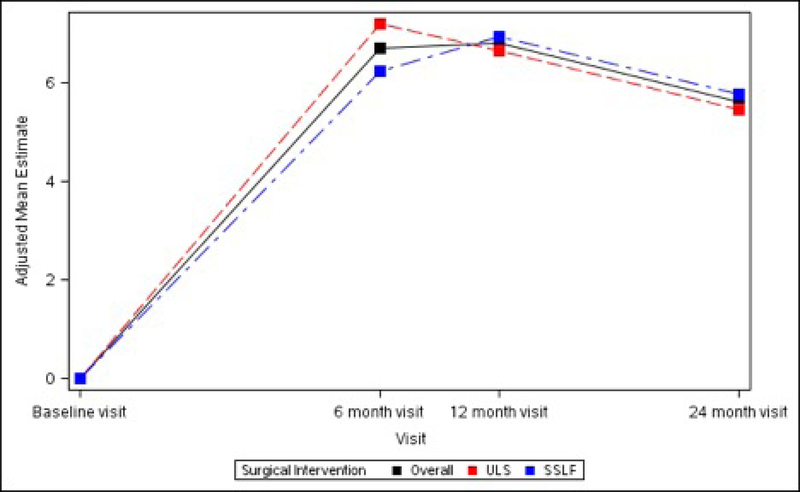
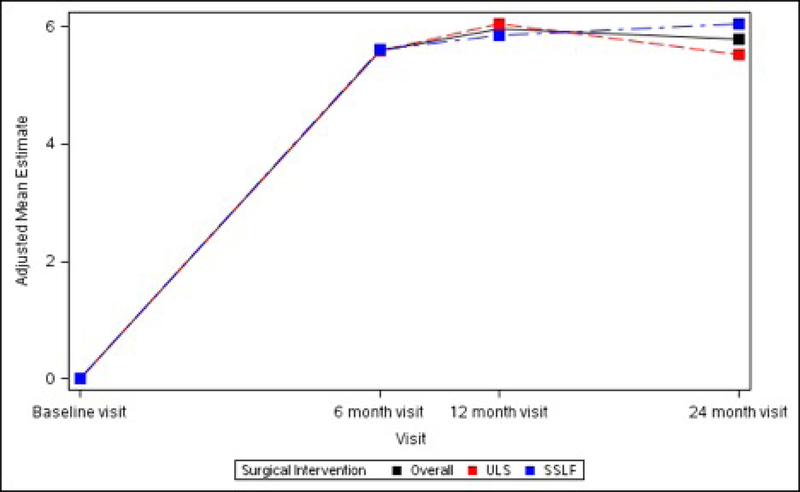
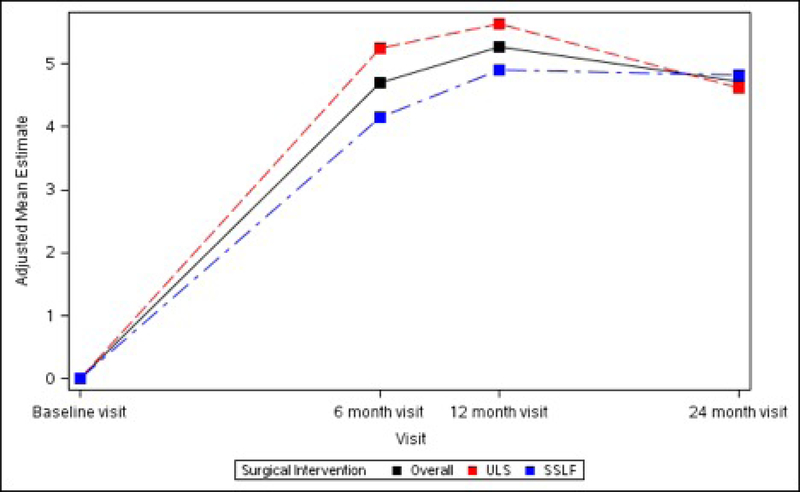
Figures 4A – 4C. Long-term Pain and Activity After Surgery SF36 Scale Changes from Baseline to 3 Months After Surgery Modeling Outcome as Change from Baseline1.
Figure 4A. SF-36 Bodily Pain Scale Change from Baseline across Visits by Surgical Interventions
Figure 4B. SF-36 Physical Functioning Scale Change from Baseline across Visits by Surgical Interventions
Figure 4C. SF-36 Role Physical Scale Change from Baseline across Visits by Surgical Interventions
1The analyses for each outcome of interest were performed on the modified intent to treat population (mITT) which includes all participants that were eligible, gave consent, were randomized to both the PMT and surgical interventions, and for whom the outcome was assessed (i.e. non-missing). For analyses assessing each outcome’s change from baseline to a follow-up visit, all adjusted means, mean differences, standard errors, 95% confidence intervals, and p-values for outcomes were obtained from general linear models adjusting for randomized surgical intervention, randomized PMT intervention, visit, interaction between visit and randomized surgical intervention, interaction between visit and randomized PMT intervention, and three-way interaction between visit and randomized surgical intervention and randomized PMT intervention, concomitant hysterectomy, age at surgical randomization, race (white, black, other), ethnicity, public insurance, and private insurance while controlling for a random surgeon effect (if found statistically significant) and repeated subject visits. All tests were conducted at a significance level of 0.05.