To the Editor:
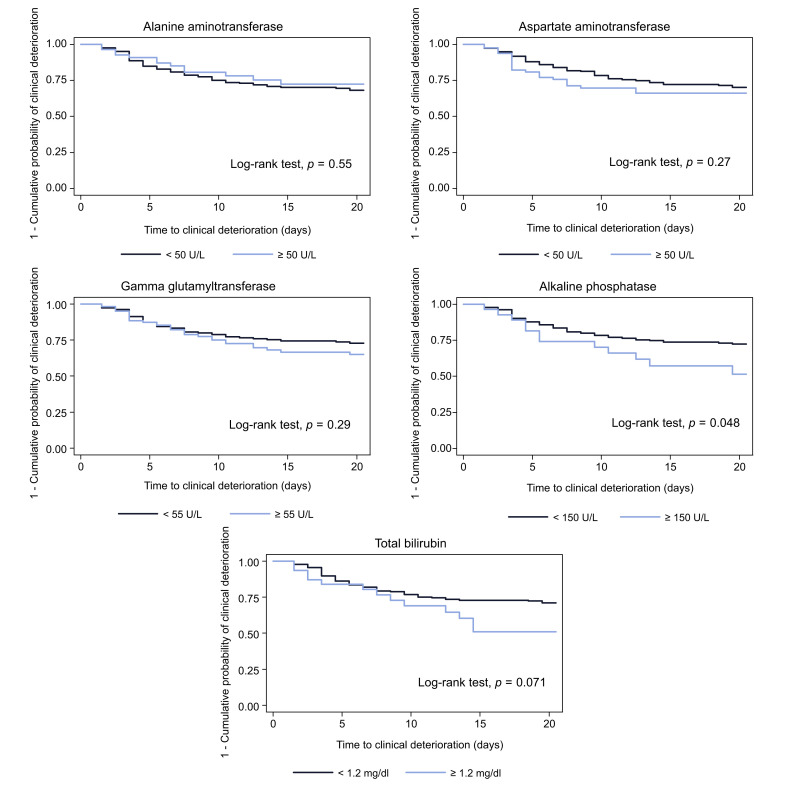
We read with interest the recent study by Cai et al.,1 which describes the role of liver function tests (LFTs) in a population of hospitalized patients with COVID-19. The authors' finding of a 41% prevalence of at least 1 elevated LFT in patients at admission appears to be higher than those previously reported in other cohorts of patients from Asia (25–30%).2 , 3 Similarly, when analyzing a consecutive cohort of 292 patients with RT-PCR-confirmed COVID-19 admitted to our center until 30 March 2020, we also noticed that the prevalence of elevated LFTs was lower in our cohort. Increased aspartate aminotransferase (AST) or alanine aminotransferase (ALT) values >50 UI/L were seen in 18.5% and 26.7% of patients, respectively. While an increase in gamma glutamyltransferase (GGT) >55 U/L was observed in 36.2%, alkaline phosphatase (ALP) >150 U/L in 9.6%, and total bilirubin >1.2 mg/dl in 10.6%.4 Pre-existing advanced liver disease was reported in 6 patients (2%), while antiviral treatment with lopinavir/ritonavir was administered in 250 patients (85.9%). In our case series we could not replicate the finding that patients presenting with abnormal LFTs at admission evolve towards a more severe form of pneumonia. Clinical deterioration occurred in 82 patients (28.1%), with 27 (9.2%) admitted to the intensive care unit (ICU) and 56 (19.2%) dying during observation. By performing univariable Kaplan-Meier survival analyses for any of the LFTs at admission, with the aim of assessing factors associated with death or admittance to the ICU, we did not find an association between markers of hepatocellular injury (AST or ALT), GGT and total bilirubin, and these endpoints. The only predictive factor associated with deterioration was the elevation of ALP above 150 IU/L (p = 0.048) (Fig. 1 ). This data is in line with other studies which reported a high prevalence of LFT abnormalities in COVID-19 but failed to demonstrate an association with worse outcomes.3 Interestingly, our observation on the clinical value of ALP as a marker of poor prognosis is in contrast with the finding by Cai and colleagues that the risk of progression to severe disease was associated with hepatocellular (AST and/or ALT >3× the upper limit of normal [ULN]) or mixed (a combination of AST/ALT >3× ULN and ALP/GGT >2× ULN) pattern of LFTs elevation, rather than a cholestatic pattern. While the prognostic value of ALP could be explained by SARS-CoV-2's tropism for the liver and angiotensin-converting enzyme 2 expression in hepatocytes and cholangiocytes, we cannot exclude the possibility that isolated ALP elevation may just be a marker of patient frailty or represent a stronger systemic inflammatory response to SARS-CoV-2 infection, rather than being a sign of cholestatic liver injury. A recent study from Asia showing a correlation between the increase in LFTs and other inflammatory markers supports this hypothesis.5
Fig. 1.
Predictors of clinical deterioration leading to ‘ICU transfer or death’ in hospitalized patients with COVID-19: Univariable Kaplan-Meier survival curves.
In conclusion, we think that although LFTs alterations are common in hospitalized patients with COVID-19, it is still unclear whether they carry any prognostic value. Laboratory LFTs should thus be interpreted with caution and always in the context of a complex multi-organ disease.
Financial support
The authors declare no financial support relevant to the study.
Authors' contribution
EV, NP, SD and AA contributed to the study concept and design; EV and NP acquired the data; all authors analyzed and interpreted the data; DP performed the statistical analysis; EV, NP and AA drafted the manuscript; all authors critically revised the manuscript.
Conflicts of interest
The authors declare no conflicts of interest relevant to the study.
Please refer to the accompanying ICMJE disclosure forms for further details.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhep.2020.05.033.
Supplementary data
References
- 1.Cai Q., Huang D., Yu H., Zhu Z., Xia Z., Su Y. COVID-19: abnormal liver function tests. J Hepatol. 2020;73(3):566–574. doi: 10.1016/j.jhep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fan Z., Chen L., Li J., Chen X., Yang J., Tian C. Clinical features of COVID-19-related liver functional abnormality. Clin Gastroenterol Hepatol. 2020;18(7):1561–1566. doi: 10.1016/j.cgh.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y., Zheng L., Liu L., Zhao M., Xiao J., Zhao Q. Liver impairment in COVID-19 patients: a retrospective analysis of 115 cases from a single center in Wuhan city, China. Liver Int. 2020 doi: 10.1111/liv.14455. [published online ahead of print, 2020 Apr 2] [DOI] [PubMed] [Google Scholar]
- 4.Aghemo A., Piovani D., Parigi T.L., Brunetta E., Pugliese N., Vespa E. Covid-19 digestive system involvement and clinical outcomes in a large academic hospital in Milan, Italy. Clin Gastroenterol Hepatol. 2020;18(10):2366–2368.e3. doi: 10.1016/j.cgh.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie H., Zhao J., Lian N., Lin S., Xie Q., Zhuo H. Clinical characteristics of non-ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. 2020;40(6):1321–1326. doi: 10.1111/liv.14449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.