To the editor:
We read with great interest the article of Hau, et al. regarding the “How about actively using telemedicine during the COVID-19 pandemic?” [1]. We are inspired to share our practical experience in using Telemedicine to deliver rehabilitation to vulnerable patients with chronic lung and heart diseases.
Since the COVID-19 was declared a global pandemic, and a US national emergency, many hospitals in the US began to limit or cancel face to face out-patient appointments to minimize the risk of transmission and to comply with US federal guidance on social distancing. At the Michael E DeBakey VA Medical Center, our team continued to provide telehealth rehabilitation for veterans suffering from chronic pulmonary and cardiac diseases.
In our program, patients connect to providers (e.g., physical and respiratory therapists, cardiologist, pulmonologist) through a secure Veterans Health Administration (VHA) internet connection (VA Video Connect, VVC) from their homes using iPADs, smart phones or computers. Providers use computer with webcams and microphones and are able to identify new or recurrent problems and establish plans of care through virtual examination. Patients can be coached by respiratory and physical therapists on proper use of inhalers, effective breathing, and how to perform exercises during the Telehealth rehabilitation appointment using direct observation and visual prompting [2].
Veterans are eligible for the Telehealth program if they: (1) are medically stable and receiving optimal medical management; (2) have no severe cognitive impairments; (3) able to use a computer and e-mail or have a family member to assist them; and (4) have correctable (glasses or hearing aids) visual and auditory impairments.
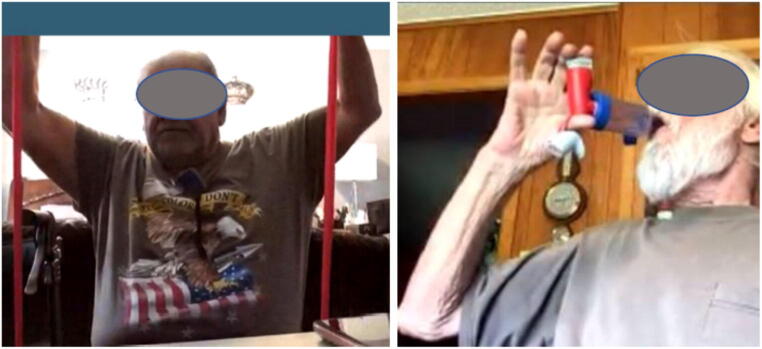
New patients are mailed a program package prior to program enrollment. Patients are also given an exercise pictorial booklet, an exercise compact disc (audio and video), small exercise apparatuses (e.g., resistance bands, ergometer, and pedometer), incentive spirometer, pulse oximeter, cough assistive device, blood pressure monitor, educational booklets about COPD or their cardiac disease, and a diary to track their progress and vitals, such as blood pressure, glucose, and weights (Fig. 1).
Fig. 1.
Patient performed exercise and learned proper inhaler technique during Telehealth VVC session
There are certain limitations in using Telehealth for cardiopulmonary rehabilitation; we cannot perform the physical tests such as 6-min walk test (6MWT), manual muscle, test grip strength, and gait that we typically use to tailor our rehabilitation program as described previously [2]. Therefore, we modified to use 1-min Sit-To-Stand test (1STS) to assess exercise capacity and cardiovascular responses instead of the 6MWT [3]. The 5 times STS test is used to assess strength [4] and to monitor improvement in muscle strength during the course of the program. We could assess balance impairment, risk of fall, limited range of motion and pain during the VVC appointments to guide any precautions for the rehabilitation prescription. Correct inhaler use, breathing patterns, coughing can be assessed easily with the virtual connection. Questionnaires including Dyspnea Modified Medical Research Council Scale, St. George Respiratory Questionnaire, the COPD Assessment Test, Cardiac Self-Efficacy Scale, Duke Activity Status Index, Rate Your Plate, Extent of Adherence Patient Health Questionnaire-9, and Activities of Daily Living can be administered through Telehealth without difficulty.
We did uncover several technical issues in using Telehealth for rehabilitation. There must be sufficient stability and speed of the internet connection. A telephone is always needed as an alternative means of communication in case of a poor Wi-Fi connection. Patients need some technical training because many of these patients have limited computer skills. Lastly, we needed to provide training for self-measurements of BP and oxygen saturation.
Telehealth had advantages during this period. We continued therapy with existing patients, and enrolled new patients despite the need to limit face-to-face patient contact. This continuity was appreciated by our patients, as one patient commented:” If I wasn’t in the program, I would be in bad shape. Now I can take deep breaths, get more oxygen and stay calm. The exercises gave me something to do inside, so I didn’t stress out during the lockdown. I learned to take breathing medications correctly and was able to keep from getting sick. I didn’t have to go to the VA and risk getting the bad virus. I was able to lose weight even while being stuck inside the house.”
We hope that our experience will encourage other providers to use Telehealth during COVID-19 and continue to use this new avenue thereafter. Telehealth can help to reduce the time and cost or travel for patients, and break down the geographic barriers for patients who live in remote or rural areas, or who are otherwise unable to come to the hospital with ease.
Funding Information
The clinical program was supported by a Veterans Health Administration, Department of Veterans Affairs (Sharafkhaneh, A & Bryant, MS). Grant No. 016ORH20.
Compliance with Ethical Standards
Conflict of Interest
All authors report no conflict of interest.
Human Participants and/or Animals
This study does not contain any studies with human participants or animals.
Informed Consent
Informed consents to use pictures were obtained and were attached.
Footnotes
This article is part of the Topical Collection on Mobile & Wireless Health
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hau YS, Kim JK, Hur J, Chang MC. How about actively using telemedicine during the COVID-19 pandemic? J. Med. Syst. 2020;44(6):108. doi: 10.1007/s10916-020-01580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bryant MS, Bandi VD, Nguyen CK, Lan C, Henson HK, Sharafkhaneh A. Telehealth Pulmonary Rehabilitation for Patients with Severe Chronic Obstructive Pulmonary Disease. Fed. Pract. 2019;36(9):430–435. [PMC free article] [PubMed] [Google Scholar]
- 3.Gephine S, Bergeron S, Tremblay-Labrecque PF, Mucci P, Saey D, Maltais F. Cardiorespiratory Response during the 1-min Sit-to-Stand Test in Chronic Obstructive Pulmonary Disease. Med. Sci. Sports Exerc. 2020 Jan 17. [Epub ahead of print]. [DOI] [PubMed]
- 4.Buatois S, Miljkovic D, Manckoundia P, Gueguen R, Miget P, Vançon G, Perrin P, Benetos A. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J. Am. Geriatr. Soc. 2008;56(8):1575–1577. doi: 10.1111/j.1532-5415.2008.01777.x. [DOI] [PubMed] [Google Scholar]