Abstract
INTRODUCTION:
Today, it is important to use different indices to measure the performance of hospitals. This study aimed to investigate and evaluate the performance indicators of military hospitals and measurement of performance by using the Pabon Lasso model.
METHODS:
This was an applied and descriptive-analytical study that was conducted among five military hospitals affiliated to the Army of the Islamic Republic of Iran by using data from 2017 to 2018. Raw data related to performance indicators such as bed occupancy ratio (BOR), average length of stay (ALoS), and bed turnover rate (BTR) were collected by referring to the hospital medical record unit. After comparing performance indicators with the standards of the Ministry of Health, the Pabon Lasso model was used to measure hospitals' performance.
RESULTS:
In general, the average BOR and bed turnover interval rate are higher than that of the national standard in all hospitals and are in favorable status. However, the average length of stay in all hospitals was in unfavorable status. Furthermore, one and two hospitals were located in zone 3 in Pabon Lasso graph in the years 2017 and 2018, respectively. Overall, there was no change in the performance of the hospitals in the study time periods.
CONCLUSION:
In general, except for the average length of stay indicator, hospitals had a favorable performance level. Therefore, planning to improve performance indicators should be at the top of the programs.
Keywords: Military hospital, Pabon Lasso model, performance indicators, standard
Introduction
Today, hospitals are considered a key element in the provision of health in societies. In developing countries, these organizations are recognized as the largest and most expensive unit of health care and consume approximately 50%–80% of the total health resources.[1] However, the efficiency of these hospitals is <50% of their potential capacity and often have no proper performance level.[2] Therefore, in recent years, the health sector in most countries has experienced a significant increase in the health expenditures due to increase in hospital costs. Studies have shown that this increase in these costs can be partly due to inefficient use of resources.[3] Therefore, given the increasing hospital costs and low performance levels along with the scarcity of resources in most hospitals, it is clear that health system managers, planners, and decision makers are looking for ways to get out from the current situation and improve hospital performance.
In the meantime, measuring and evaluating the performance of hospitals is very useful, which shows how resources are used in hospitals. Performance evaluation of the different hospital wards provides information needed for managers to evaluate and monitor the current situation in hospitals.[4]
Various techniques from simple graphical models to complex mathematical and economical models have been considered to evaluate the health system performance and increase efficiency and productivity.[5] Calculation of performance indicators and comparison with standard levels as well as the use of the Pabon Lasso model are considered as the techniques used. The strengths and weaknesses of hospitals and their distance to optimal status (standard level) were determined by comparing hospital indicators with standards.[6]
Furthermore, Pabon Lasso model is one of the most used and important models for the evaluation of hospital performance. This graph was first introduced by Pabon Lasso in 1986 and used internationally to compare hospital performance. The graph assesses the hospital performance by the combination of the following three indicators: bed occupancy ratio (BOR), bed turnover rate (BTR), and average length of stay (ALoS).[7,8,9,10]
Simplicity, quick extraction and performance status analysis, as well as comprehensibility are some of the positive features of this model. Furthermore, these models due to the possibility of the combination of three indicators are more valid compared to performance measures that evaluate hospital performance by using only one indicator.[11] Therefore, these models are widely used in the performance evaluation of hospitals.
Many studies have investigated the performance of hospitals using the Pabon Lasso model. Studies conducted in the hospitals of East Azerbaijan and Kerman Provinces showed that almost half of the hospitals surveyed were located in zone 1 (reflecting the inefficiency and waste of resources).[9,12] Furthermore, in a hospital performance study that was conducted by using the Pabon Lasso model in Tunisia, the results showed that 50% of hospitals performed poorly.[13]
Because hospitals affiliated to the army play an important role in providing health care with the least prices for a significant percentage of the country's population, checking the performance of these hospitals is very important. Performance evaluation also plays an important role in increasing the efficiency of these hospitals and even the country's health system. In the past, no research has been conducted to evaluate the performance of army hospitals in Iran; hence, for the first time in this article, we review the army hospitals' performance indicators and compare them with the national standards. This study also compares the real performance status of hospitals by using Pabon Lasso model and presents appropriate strategies for improving the performance.
Methods
This descriptive-analytical study was carried out among five selected hospitals affiliated to the Army of the Islamic Republic of Iran in the years 2017 and 2018. To make the study sample more homogeneous, nonspecialized hospitals were selected for the sample. Due to confidentiality and ethical aspects, the names of the hospitals were not disclosed. After obtaining permission from the Ethics Committee, raw data were collected by referring to the medical record and statistics units in hospitals. Standard formulas were used to calculate BOR, BTR, and average length of stay (ALoS).[10]
BOR = Number of days occupied − number of beds/active day − number of active beds
BTR = Total number of admissions/average number of active beds
ALoS = Number of days occupied − number of beds/number of patients discharged and deceased.
Then, after calculating the indicators in each hospital, these indicators were compared with the standard values [Table 1] and classified into favorable, moderate, and unfavorable. The standard indicators of the Ministry of Health and Medical Education which are presented in Table 1 were considered as the criteria for judging the hospital indicators status in the present study.[10]
Table 1.
Hospitals’ performance indicators and their standards
| Indicator | Favorable | Moderate | Unfavorable |
|---|---|---|---|
| Active to fixed bed ratio (%) | 75-80 | 74-60 | 60< |
| Bed occupancy ratio (%) | <70 | 60-70 | 60< |
| Bed turnover rate | 2< | 2-3 | <3 |
| Average length of stay (day) | 3.5< | 3.5-4 | <4 |
| Number of surgeries to operating rooms ratio (surgery day) | 4 | 2-4 | 2< |
| Number of dead to hospitalized (%) | 2< | 2-3 | <3 |
Furthermore, after examining the data normality, paired t-test in SPSS software version 17 (SPSS Inc., Chicago, IL, USA) was used to compare performance indicators in 2 different years.
Then, the efficiency and performance of the hospitals were calculated and compared by using Microsoft Excel program and Pabon Lasso model. In this graph, BOR and BTR are located on the horizontal and vertical axes, respectively. Using the weighted average of BOR and BTR in hospitals, the optimal values of these two indicators were obtained. Thus, with the emergence of two crossover lines from the interconnection of two optimal values, four zones appear in the graph. Then, using the numerical value of each hospital's indicators (BOR and BTR), their location and the zone of each hospital's location were drawn. In this graph, the average length of stay can be determined by connecting the line drawn from the coordinate origin to the hospital's coordinate point and along the opposite side.[14] Table 2 shows the features of the four zones of the Pabon Lasso graph.
Table 2.
The features of four zones in the Pabon Lasso graph
| Zone 1: Low BOR and BTR and high ALoS (the supply of bed exceeds the demand. The performance of the hospital is poor) |
| Zone 2: Low BOR and ALoS and high BTR (represents unnecessary hospitalizations and extra bed capacity in hospitals) |
| Zone 3: High BOR and BTR and low ALoS (hospitals have appropriate efficiency though minimum number of beds have used) |
| Zone 4: Low BTR and ALoS and high BOR (represents long-term hospitalizations and underutilization of outpatient facilitates and imposes high costs) |
ALoS=Average length of stay, BOR=Bed occupancy ratio, BTR=Bed turnover rate
Results
Based on the data analysis presented in Table 3, the mean bed occupancy rates in the years 2017 and 2018 were 73.76% and 72.41%, respectively, which were in desirable status when compared with the standards of the Ministry of Health [Table 1]. Furthermore, the highest and lowest bed occupancy rates in both years were in hospital “2” and hospital “5,” respectively. Overall, BOR slightly decreased in all hospitals over time.
Table 3.
Statistical information and performance indicators obtained in military hospitals affiliated to the Army of the Islamic Republic of Iran in 2017-2018
| Hospital | Indicator, 2017-2018 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bed occupancy ratio | Average length of stay | Bed turnover interval rate | Bed turnover rate | Average active bed | Net mortality | |||||||
| 1 | %77.2 | %73 | 5.7 | 4.4 | 1.6 | 1.7 | 74 | 72 | 149 | 159 | 3.36 | 2.95 |
| 2 | %78 | %76 | 4.02 | 4 | 1.6 | 1.9 | 70 | 66 | 118 | 130 | 3.22 | 2.98 |
| 3 | %70.6 | %70.01 | 5.3 | 5.2 | 2.01 | 2.1 | 79 | 77 | 133 | 146 | 3.39 | 3.14 |
| 4 | %74 | %73 | 4.4 | 3.9 | 1.1 | 1.3 | 69 | 71 | 112 | 122 | 3.01 | 2.94 |
| 5 | %69 | %70 | 4.2 | 3.8 | 1.5 | 2.1 | 61.4 | 63 | 138 | 151 | 2.87 | 2.74 |
| Mean (SD) |
%73.76 (3.95) |
%72.41 (2.5) |
4.7 (0.73) |
4.2 (0.57) |
1.5 (0.32) |
1.8 (0.33) |
70.6 (6.5) |
69.8 (5.4) |
130 (1.5) |
141.5 (1.52) |
3.17 (0.22) |
2.95 (0.14) |
| P | 0.18 | 0.11 | 0.051 | 0.48 | 0.00 | 0.02 | ||||||
SD=Standard deviation
The average length of stay in the years 2017 and 2018 were 4.7 and 4.2 days, respectively, which were in undesirable status when compared with the standards of the Ministry of Health. The highest average length of stay was 5.7 at hospital “1” in 2017, and the lowest was 3.8 at hospital “5” in 2018. Furthermore, the average of bed turnover interval rates were 1.5 and 1.8 in 2017 and 2018, respectively, which were in desirable status compared to the Ministry of Health standards. Hospital “3” had the highest bed turnover interval rate of 2.01 and 2.1 in 2017 and 2018, respectively. Furthermore, hospital “4” had the lowest bed turnover interval rate in 2017.
The average BTR was 70.6 and 69.8 in 2017 and 2018, respectively. Hospitals “3” and “5” had the highest and lowest BTR indicators, respectively. The average active bed indicator was 130 and 141.5 in 2017 and 2018, respectively. Hospital “1” with the active bed indicators of 159 and 149 had the highest indicator in both years, respectively. Whereas hospital “4” had the lowest number of active beds in both years. The average net death rates were 2.95 and 3.17 in 2017 and 2018, respectively, which decrease 0.06% overall. When comparing this indicator with the Ministry of Health standards, the findings showed that all hospitals have undesirable and poor status in 2017 (except hospital “5”). However, in 2018, in general, the average of net mortality indicator improved and was at an average status compared to the previous year. Hospitals “3” and “5” had the highest and lowest net mortality rates, respectively.
Furthermore, paired t-test results showed that only net mortality and active bed indicators experienced statistically significant changes (P < 0.05), and there were no statistically significant changes (P > 0.05) in other variables between the two time periods. Table 3 summarizes the hospitals' indicators covered by the study.
Then, after comparing and analyzing the performance indicators, the performance of the hospitals was evaluated by using Pabon Lasso model. According to the Pabon Lasso graph, only the hospital “5” was located in zone 1 in two time periods, indicating poor efficacy and limited use of hospitals' capacity. Only hospital “1” was located in zone 3 in 2017; meanwhile, hospitals “1” and “4” were located in this zone, which shows a better performance and thus a satisfactory level of productivity. Furthermore, hospital “3” due to lower BOR and a relatively high BTR was located in zone 2 in the both years. Hospital “2” with high bed occupancy and low BTR was located in the zone 4 of the Pabon Lasso model in both years of the study. Table 4 and Figure 1 shows hospitals' zone location and hospitals' performance in Pabon Lasso model in 2017 and 2018, respectively.
Table 4.
Hospitals’ zone location in Pabon Lasso graph
| Hospital | Hospitals’ location zone in 2017 | Hospitals’ location zone in 2018 | Trend |
|---|---|---|---|
| 1 | 3 | 3 | Unchanged |
| 2 | 4 | 4 | Unchanged |
| 3 | 2 | 2 | Unchanged |
| 4 | 4 | 3 | Improved |
| 5 | 1 | 1 | Unchanged |
Figure 1.
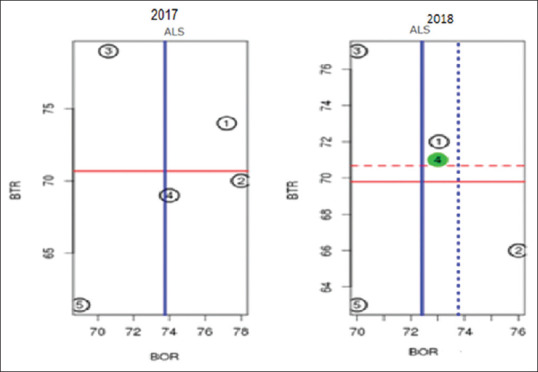
Hospitals' performance by Pabon Lasso model in 2017 and 2018
Discussion
The purpose of this study was to compare performance indicators with the existing standards and to evaluate the performance of military hospitals affiliated to the Army of the Islamic Republic of Iran in Tehran.
By comparison the performance hospitals indicators with national standards [Table 1] in both years, the results showed that some of the indicators are higher than standards and were in a favorable status. BOR in the hospitals of this study was above the standard level and the national average (70%) in both years 2017 and 2018, which is consistent with the study of Sadeghifar et al.[15] In Kavosi et al.'s study, the results showed that four out of 14 hospitals had BOR indicator higher than the standard level.[16] Furthermore, Arzamani et al. showed in their study that these indicators were higher than the national standard in hospitals of North Khorasan province in Iran and were in favorable status.[17] In some international studies, the BOR was much higher than the results of the present study; for example, according to the Zhu study in Singapore, the average BOR was reported to be around 90%.[18] Furthermore, a study conducted at a specialized hospital showed that the BOR increased from 54.3 to 86.3 during the study periods (2004–2013) in Egypt.[19] However, in a study conducted by Uy et al. in Cambodia's capital hospitals, the BOR indicator was 58.8%, which was much lower than the results of the present study.[20] This difference could be due to lower per capita public spending on health care, ineffective management, or hospitalization and treatment of long-term diseases.
In general, the favorable bed occupancy indicator status in hospitals indicating the proper use of beds in hospitals by managers. Managers can increase the BOR indicator by set up and use active beds in hospital wards, increase skilled treatment staff and provide facilities, create a systematic and advanced admission system to facilitate patient access, and ultimately increase patient satisfaction with hospitals' performance.
In the present study, the BTR and bed turnover interval rate were in favorable status compared with the standards. In Jonaidi et al.'s study, the bed turnover interval rate and average length of stay were in unfavorable status and other indicators were in favorable status.[21] However, in some national and international studies, these indicators were far from the standard values and were in unfavorable status.[22,23] This difference can be due to a lack of demand or there may be a defect in the patient admission procedure. Therefore, fixing these defects can improve these indicators in hospitals.
The results of the present study showed that the average length of stay and net mortality rate indicators in the hospitals were not in a favorable status in compared to the national standard indicators. The results of this study were consistent with those of the study by Barfar et al.[24] Furthermore, Kalhor et al. showed that the average length of stay in general hospitals was 4.3, 4.8, and 4.5 days, respectively, which were not in favorable status.[25] A study conducted by Ajlouni found that long-term hospital stay was a serious challenge in Jordanian public hospitals.[26] Unlike to the present study, the results of other studies conducted in Iran showed that the average length of stay in different hospitals was in a favorable status. Accordingly, in two studies conducted by Arzamani et al. and Sadeghifar et al., hospitals were in favorable status in terms of patient's average length of stay.[15,17] A study conducted by Pabon Lasso in Colombian hospitals found that the average length of stays in hospitals with beds <100 and ≥200 was 5.2 and 7.2 days, respectively.[27] According to the World Bank report, the average length of stay in countries such as Australia, Canada, Egypt, France, and Germany was 14, 12, 8, 11, and 14 days, respectively.[28] Furthermore, a study conducted in Indian and Egyptian hospitals showed that the mean hospital length of stay was 6.3 and 7.75 days, respectively.[19,29] However, the results of a study conducted by Iswanto in Indonesian hospitals showed that the average length of stay was 2–3 days, and it was at a favorable status.[30]
These differences in the study results could be due to differences in the type of population covered by hospitals, the type of hospital services provided, time period of the studies, and hospitalization of long-stay patients.
Furthermore, common problems such as the prolongation of different processes in the admission units and within the wards and paraclinics all lead to an increase in this indicator, which has led to differences in the results of the present study with others.
Furthermore, Pabon Lasso model results showed that except hospital “4,” all the other hospitals were located in the same zone in both years, and there was no change in the performance of the hospitals. Hospitals with BOR and BTR lower than the optimal level located in zone 1 in Pabon Lasso graph showed poor hospital performance. In this study, only hospital “5” was located in zone 1. In studies by Mohammadi et al. and Hafidz, 36.78% and 37% of hospitals were located in this zone, respectively.[31,32] In the study by Barfar et al., three hospitals were located in zone 1.[24] Hassan et al. showed that five, four, three, and two hospitals were located in zone 1 in Pabon Lasso graph in the years 2012–2015, respectively,[33] which is consistent with the present study results.
In addition, among the international studies, Nabukeera et al. and Nwagbara and Rasiah showed that 50% and 37.9% of hospitals were located in zone 1, respectively.[23,34] Although in some studies, no hospital was located in this zone[25] which could be due to better performance and differences in hospital management style.
The zone 2 in Pabon Lasso graph was dedicated to those hospitals that have a high BTR due to their specific type of activity (such as short-term inpatient centers or gynecological hospitals). In this study, only the hospital “3” was located in the zone 2; therefore, the hospital does not have a satisfactory performance, and it is recommended that improving hospital performance should be at the forefront of managers' planning to move the hospitals to the third zone. Zahiri and Keliddar showed that seven of the 26 hospitals studied were located in zone 2.[35] Furthermore, in the study by Mehralhasani et al., nine hospitals were located in this zone.[36] Furthermore, in a study conducted by Iswanto in Jakarta, Indonesia, the results showed that the health center was located in zone 2 in Pabon Lasso graph.[30] Due to outpatient admission and non-special ized services this health center, the BTR was high, so it had similar performance results to the present study.
Hospitals that have favorable performances were located in the third zone in Pabon Lasso graph. These hospitals have achieved good productivity with a certain number of beds used and are efficient in managing affairs. The present study results showed that only hospital “1” was located in the third zone in 2017. Furthermore, only hospitals “1” and “4” were located in this zone in 2018. In addition, Asbu et al. found that 39% and 27.5% of hospitals in their studies were located in zone 3.[22,37] Furthermore, Sajadi et al. showed that 45% of the hospitals in their study were located in zone 3.[38] In a study carried out among Egyptian hospitals in Cairo, the results showed that 46%, 60%, and 53% of hospitals were located in this zone during the survey period (2006–2008), respectively.[26] Furthermore, in the studies conducted by Nabukeera et al., Nwagbara and Rasiah, and Hafidz et al., 20%, 35.6%, and 37% of hospitals were located in this area, respectively.
In this study, the hospitals were able to make the maximum use of resources and attracted more customers due to some reasons such as being a trauma center in the city, having a reputation and experienced medical staff, use of advanced medical equipment and technologies, and easy access. Therefore, continuing to improve hospital performance and moving hospitals to the northeast of the Pabon Lasso graph should be a priority in the hospital managerial planning.
In this study, only hospitals “4” and “2” were located in zone 4 in 2017, although only hospital “2” was located in this area and hospital “4” was shifted to zone 3 in 2018. Although in these hospitals unused beds are low and have high BOR and work relatively well, they have a low BTR and high length of stay. The study by Mohammadkarim et al. showed that 17.5% of hospitals were located in this zone.[22] Moradi et al. showed that 1 and 3 hospitals were located in zone 4 before and after the implementation of the Iranian Health System Reform Plan, respectively.[12]
However, this study was restricted as most studies. Due to the difficulties and limitations in collecting data needed for other military hospitals, the results of the present study could not be generalized to other hospitals. Other limitations of this study are the lack of standard defined for each indicator in military hospitals apart from the Ministry of Health standards. On the other hand, the Pabon Lasso model only represents the utilization of the resources available to the hospitals and it does not consider the quality and importance of health care.
Conclusion
The results of the study showed that the status of the evaluated indicators in military hospitals was better than the standards set by the Ministry of Health, although some indicators were in unfavorable status in some hospitals. Furthermore, the Pabon Lasso graph results showed that 1, 1, 1, and 2 hospitals were located in zone 1, 2, 3, and 4 in 2017, respectively. Furthermore, only one hospital was shifted from zone 4 to 3 in 2018.
The results of this study are very useful for managers and policymakers in the military health sector who are looking for ways to improve performance and consume health resources.
By comparing performance indicators with standards and examining the performance of military hospitals by the Pabon Lasso model, managers can be aware from standard deviation and also identify inefficient hospitals with unfavorable performance. Therefore, it is necessary for military health sector managers to take corrective actions for hospitals located in zone 1, as well as indicators that are far from the standard levels. Also, managers should identify the factors that affecting improvement in hospital with favorable performance and by modeling and adjusting these factors for hospitals with unfavorable performance, they will make rapid improvements in performance indicators in military hospitals that located in inefficient zone.
Therefore, it is suggested that future studies use new qualitative approaches, especially Six Sigma, which is based on both quality and quantity improvement. Furthermore, it is recommended that this study be conducted over more time period and hospitals for future research.
Financial support and sponsorship
The present study is part of a research project number “91000368” funded by AJA University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the Vice-Chancellor of Research and Technology of AJA University of Medical Sciences, as well as all the hospital staff for their cooperation in this research.
References
- 1.Barnum H, Kutzin J. Public Hospitals in Developing Countries: Resource Use, Cost, Financing. Baltimore, MD: Johns Hopkins University Press; 1993. [Google Scholar]
- 2.Lotfi F, Bastani P, Hadian M, Hamidi H, Motlagh S, Delavari S. Performance assessment of hospitals affiliated with Iran university of medical sciences: Application of economic techniques in health care area. J Health Adm. 2015;18(59):43–54. [Google Scholar]
- 3.Strunk BC, Ginsburg PB, Gabel JR. Tracking health care costs: Growth accelerates again in 2001: Hospital costs have secured their place as the leading driver of health care cost increases, for the second straight year. Health Aff. 2002;21(Suppl 1):W299–310. doi: 10.1377/hlthaff.w2.299. [DOI] [PubMed] [Google Scholar]
- 4.Duma O, Munteanu L. The resources utilization pattern in a general university hospital. J Prev Med. 2002;10:3–11. [Google Scholar]
- 5.Goshtasebi A, Vahdaninia M, Gorgipour R, Samanpour A, Maftoon F, Farzadi F, et al. Assessing hospital performance by the Pabon Lasso model. Iran J Public Health. 2009;38:119–24. [Google Scholar]
- 6.Ministry of Health and Medical Education. 2018. [Last accessed on 2019 Sep 25]. cited 2019 September 07. Available from: http://medcare.behdasht.gov.ir/index.aspx?siteid=312&pageid=36125 .
- 7.Hadi M, Sajadi H, Sajadi Z. Is there any method to compare key indicators of hospital performance simultaneity? Health Inf Manage. 2011;8:8–75. [Google Scholar]
- 8.Gholipour K, Delgoshai B, Masudi-Asl I, Hajinabi K, Iezadi S. Comparing performance of Tabriz obstetrics and gynaecology hospitals managed as autonomous and budgetary units using Pabon Lasso method. Australas Med J. 2013;6:701–7. doi: 10.4066/AMJ.2013.1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehrtak M, Yusefzadeh H, Jaafaripooyan E. Pabon lasso and data envelopment analysis: A complementary approach to hospital performance measurement. Glob J Health Sci. 2014;6:107–16. doi: 10.5539/gjhs.v6n4p107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Health Indicators. Ministry of Health and Medical Education. 2nd ed. Tehran: Ministry of Health and Medical Education Publication; 2008. [Google Scholar]
- 11.Lotfi F, Kalhor R, Bastani P, Shaarbafchi Zadeh N, Eslamian M, Dehghani MR, et al. Various indicators for the assessment of hospitals' performance status: Differences and similarities. Iran Red Crescent Med J. 2014;16:e12950. doi: 10.5812/ircmj.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moradi G, Piroozi B, Safari H, Esmail Nasab N, Mohamadi Bolbanabad A, Yari A. Assessment of the efficiency of hospitals before and after the implementation of health sector evolution plan in Iran based on Pabon Lasso model. Iran J Public Health. 2017;46:389–95. [PMC free article] [PubMed] [Google Scholar]
- 13.Younsi M. Performance of Tunisian public hospitals: A comparative assessment using the Pabón Lasso model. Int J Hosp Res. 2014;3:66–159. [Google Scholar]
- 14.Dargahi H, Darrudi A, Rezaei Abgoli M. The effect of iran health system evolution plan on Tehran university of medical sciences hospitals' performance indicators: A case study using the Pabon Lasso model. J Sch Public Health Inst Public Health Res. 2018;16:228–39. [Google Scholar]
- 15.Sadeghifar J, Rezaee A, Hamouzade P, Taghavi-Shahri S. The relationship between performance indicators and hospital accreditation degree in Urmia university of medical sciences. Biomon J Nurs Midwifery Coll Urmia. 2011;9:270–6. [Google Scholar]
- 16.Kavosi Z, Goudarzi S, Almasian-Kia A. Evaluating of hospital efficiency by using of Paben Lasso model in Lorestan university of medical sciences. J All Health Sci Tehran Univ Med Sci. 2013;6:365–75. [Google Scholar]
- 17.Arzamani M, Pournaghi S, Seyed-Katooli S, Jafakesh-Moghadam A. The comparison of indicators in educational hospitals of North Khorasan universities of medical sciences with the standards of the country in 2011-2012. J North Khorasan Univ Med Sci. 2012;4:513–22. [Google Scholar]
- 18.Zhu Z. Impact of different discharge patterns on bed occupancy rate and bed waiting time: A simulation approach. J Med Eng Technol. 2011;35:338–43. doi: 10.3109/03091902.2011.595528. [DOI] [PubMed] [Google Scholar]
- 19.Elayyat AH, Sadek A. Hospital utilization pattern in a hepatogastroenterology department of a research institute hospital, from 2004 to 2013. J Egypt Public Health Assoc. 2016;91:59–64. doi: 10.1097/01.EPX.0000482537.88140.0c. [DOI] [PubMed] [Google Scholar]
- 20.Uy S, Akashi H, Taki K, Ito K. Current problems in national hospitals of Phnom Penh: Finance and health care. Nagoya J Med Sci. 2007;69:71–9. [PubMed] [Google Scholar]
- 21.Jonaidi N, Sadeghi M, Izadi M, Ranjbar R. Comparison of performance indicators in one of hospitals of Tehran with national standards. Iran J Mil Med. 2011;12(4):223–8. [Google Scholar]
- 22.Mohammadkarim B, Jamil S, Pejman H, Seyyed MH, Mostafa N. Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso model. Australas Med J. 2011;4:175–9. doi: 10.4066/AMJ.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nabukeera M, Boerhannoeddin A, Raja Noriza RA. An evaluation of health centers and hospital efficiency in Kampala capital city authority Uganda; using Pabon Lasso technique. J Health Transl Med. 2015;18:12–7. [Google Scholar]
- 24.Barfar E, Khammarnia M, Baghbanian A, Panahi M. An investigation of performance at hospitals affiliated with Zahedan university of medical sciences; using Pabon Lasso technique. Medicine Public Health J. 2014;1:31–7. [Google Scholar]
- 25.Kalhor R. Assessing hospital performance using Pabon Lasso analysis. Int J Hosp Res. 2013;2:149–54. [Google Scholar]
- 26.Ajlouni M. The relative efficiency of Jordanian public hospitals using data envelopment analysis Pabon lasso diagram. Global J Bus Res. 2013;7:59–72. [Google Scholar]
- 27.Pabón Lasso H. Evaluating hospital performance through simultaneous application of several indicators. Bull Pan Am Health Organ. 1986;20:341–57. [PubMed] [Google Scholar]
- 28.SPG media. Dedicated to improving health care 2008. [Last accessed on 2019 Sep 18]. cited 2018 March 24. Available from : //WWWhospitalmanagement/netinfor/statisticalindexhtml .
- 29.Mahapatra P, Berman P. Using hospital activity indicators to evaluate performance in Andhra Pradesh, India. Int J Health Plann Manage. 1994;9:199–211. doi: 10.1002/hpm.4740090206. [DOI] [PubMed] [Google Scholar]
- 30.Iswanto A. Measuring Hospital Efficiency Through Pabon Lasso Analysis: An Empirical Study in Kemang Medical Care (KMC) Social Science Research Network. 2015 [Google Scholar]
- 31.Mohammadi M, Ziapour A, Mahboubi M, Faroukhi A, Amani N. Performance evaluation of hospitals under supervision of Kermanshah medical sciences using Pabon Lasso diagram of a five-year period (2008-2012) Life Sci J. 2014;11:77–81. [Google Scholar]
- 32.Hafidz F, Ensor T, Tubeuf S. Assessing health facility performance in indonesia using the Pabón-Lasso model and unit cost analysis of health services. Int J Health Plann Manage. 2018;33:e541–e556. doi: 10.1002/hpm.2497. [DOI] [PubMed] [Google Scholar]
- 33.Hasan Y, Parviz SS, Bahram N. Health system reform plan and performance of hospitals: An iranian case study. Mater Sociomed. 2017;29:201–6. doi: 10.5455/msm.2017.29.201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nwagbara VC, Rasiah R. Rethinking health care commercialization: Evidence from Malaysia. Global Health. 2015;11:44. doi: 10.1186/s12992-015-0131-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zahiri M, Keliddar I. Performance evaluating in hospitals affiliated in Ahwaz university of medical sciences based on Pabon Lasso model. Hospital. 2012;11:37–44. [Google Scholar]
- 36.Mehralhasani M, Yazdi-Feiz-Abadi V, Barfe-Shahrbabak T. Assessing performance of Kerman province's hospitals using Pabon Lasso diagram between 2008 and 2010. Q J Hosp. 2013;12:99–107. [Google Scholar]
- 37.Asbu E, Walker O, Kirigia J, Zawaira F, Magombo F, Zimpita P, et al. Technical efficiency of district hospitals in Malawi, an exploratory assessment using data envelopment analysis. Afr Health Monit. 2012;14(7):220–9. [Google Scholar]
- 38.Sajadi H, Sajadi Z, Hadi M. Is there any method to compare key indicators of hospital performance simultaneity? Health Inf Manage. 2011;8:71–81. [Google Scholar]


