FIGURE 1.
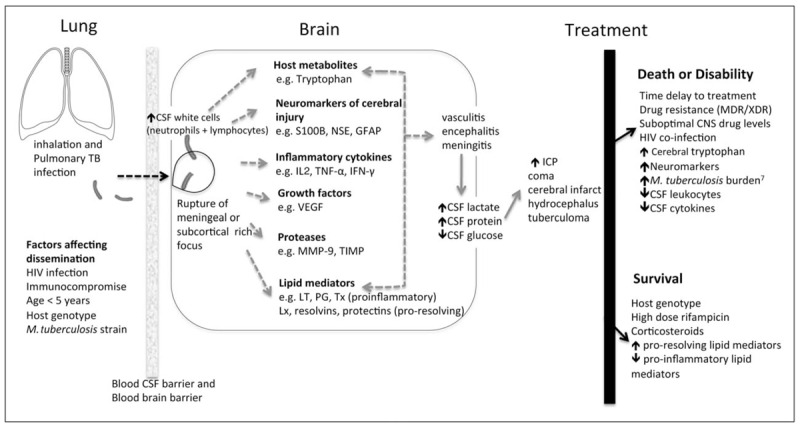
Overview of the pathophysiology of tuberculosis meningitis∗. Mortality of TBM is attributed to Mycobacterium tuberculosis and its interaction with the host immune response. Once M. tuberculosis enters the brain or meninges, a detrimental immunoinflammatory response including inflammatory cytokines, proteases, lipid mediators, neuromarkers and tryptophan metabolites, is triggered [1–6]. This leads to the cerebral disorder and complications known to occur in TBM. Knowledge gaps exist in the mechanism of bacterial invasion into the CNS and the underlying biologic pathways (dotted arrows) leading to the disease process. CSF, cerebrospinal fluid; GFAP, glial fibrillary acidic protein; HIV, human immunodeficiency virus; ICP, intracranial pressure; IFN, interferon; IL, interleukin; LT, leukotriene; Lx, lipoxins; MDR, multidrug-resistant; MMP, matrix metalloproteinases; NSE, neuron-specific enolase; PG, prostaglandin; TB, tuberculosis; TIMP, tissue inhibitor of matrix metalloproteinases; TNF, tumour necrosis factor; Tx, thromboxane; VEGF, vascular endothelial growth factor; XDR, extensively drug-resistant. Adapted from Thwaites and Tran [27]. Figure references [6,21,22▪▪,23–27].
