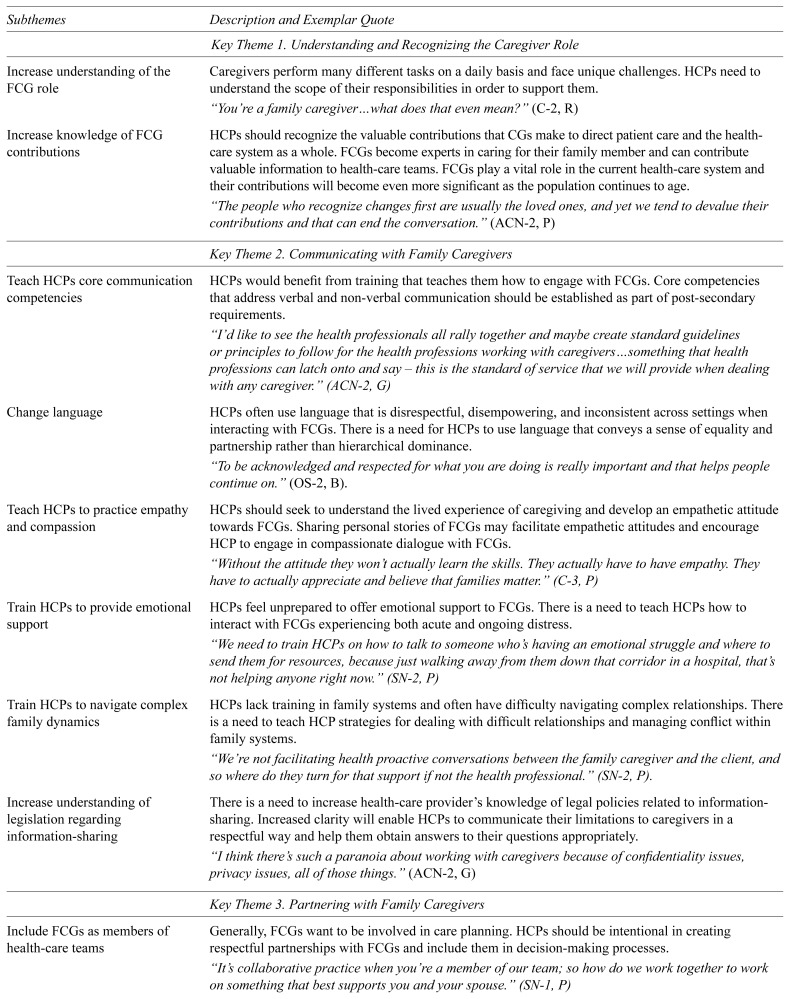
TABLE 2.
Key themes, subthemes, and descriptions for caregiver-centred care
| Subthemes | Description and Exemplar Quote |
|---|---|
| Key Theme 1. Understanding and Recognizing the Caregiver Role | |
|
| |
| Increase understanding of the FCG role | Caregivers perform many different tasks on a daily basis and face unique challenges. HCPs need to understand the scope of their responsibilities in order to support them. “You’re a family caregiver…what does that even mean?” (C-2, R) |
| Increase knowledge of FCG contributions | HCPs should recognize the valuable contributions that CGs make to direct patient care and the health-care system as a whole. FCGs become experts in caring for their family member and can contribute valuable information to health-care teams. FCGs play a vital role in the current health-care system and their contributions will become even more significant as the population continues to age. “The people who recognize changes first are usually the loved ones, and yet we tend to devalue their contributions and that can end the conversation.” (ACN-2, P) |
|
| |
| Key Theme 2. Communicating with Family Caregivers | |
|
| |
| Teach HCPs core communication competencies | HCPs would benefit from training that teaches them how to engage with FCGs. Core competencies that address verbal and non-verbal communication should be established as part of post-secondary requirements. “I’d like to see the health professionals all rally together and maybe create standard guidelines or principles to follow for the health professions working with caregivers…something that health professions can latch onto and say – this is the standard of service that we will provide when dealing with any caregiver.” (ACN-2, G) |
| Change language | HCPs often use language that is disrespectful, disempowering, and inconsistent across settings when interacting with FCGs. There is a need for HCPs to use language that conveys a sense of equality and partnership rather than hierarchical dominance. “To be acknowledged and respected for what you are doing is really important and that helps people continue on.” (OS-2, B). |
| Teach HCPs to practice empathy and compassion | HCPs should seek to understand the lived experience of caregiving and develop an empathetic attitude towards FCGs. Sharing personal stories of FCGs may facilitate empathetic attitudes and encourage HCP to engage in compassionate dialogue with FCGs. “Without the attitude they won’t actually learn the skills. They actually have to have empathy. They have to actually appreciate and believe that families matter.” (C-3, P) |
| Train HCPs to provide emotional support | HCPs feel unprepared to offer emotional support to FCGs. There is a need to teach HCPs how to interact with FCGs experiencing both acute and ongoing distress. “We need to train HCPs on how to talk to someone who’s having an emotional struggle and where to send them for resources, because just walking away from them down that corridor in a hospital, that’s not helping anyone right now.” (SN-2, P) |
| Train HCPs to navigate complex family dynamics | HCPs lack training in family systems and often have difficulty navigating complex relationships. There is a need to teach HCP strategies for dealing with difficult relationships and managing conflict within family systems. “We’re not facilitating health proactive conversations between the family caregiver and the client, and so where do they turn for that support if not the health professional.” (SN-2, P). |
| Increase understanding of legislation regarding information-sharing | There is a need to increase health-care provider’s knowledge of legal policies related to information-sharing. Increased clarity will enable HCPs to communicate their limitations to caregivers in a respectful way and help them obtain answers to their questions appropriately. “I think there’s such a paranoia about working with caregivers because of confidentiality issues, privacy issues, all of those things.” (ACN-2, G) |
|
| |
| Key Theme 3. Partnering with Family Caregivers | |
|
| |
| Include FCGs as members of health-care teams | Generally, FCGs want to be involved in care planning. HCPs should be intentional in creating respectful partnerships with FCGs and include them in decision-making processes. “It’s collaborative practice when you’re a member of our team; so how do we work together to work on something that best supports you and your spouse.” (SN-1, P) |
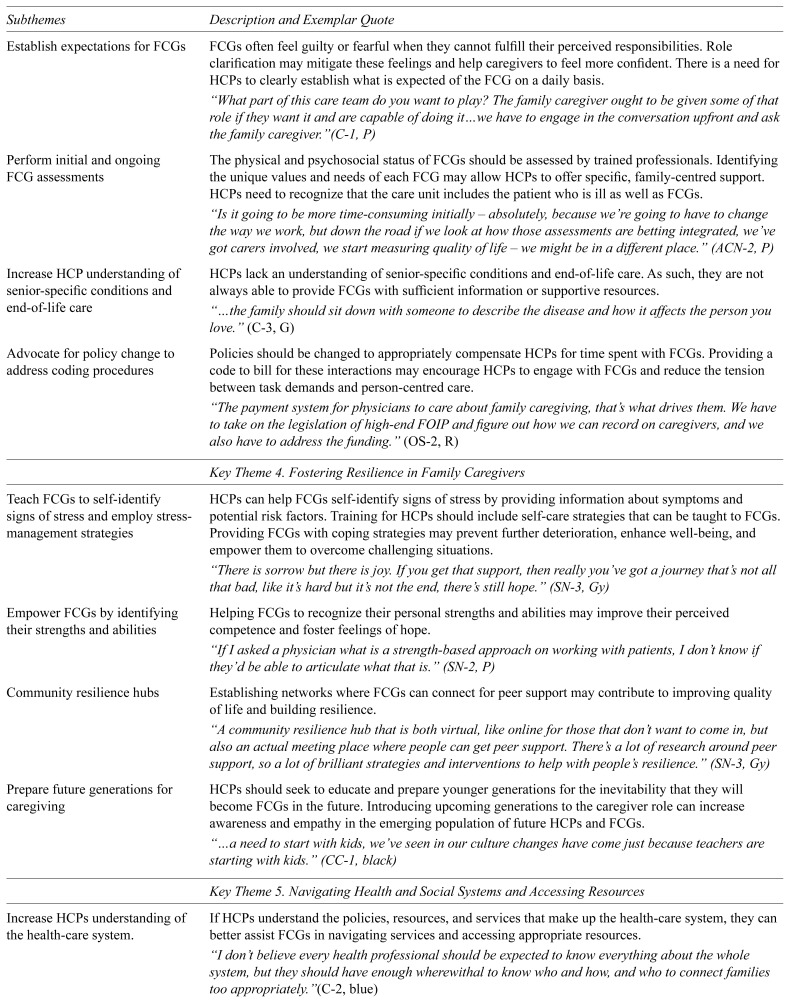
| Establish expectations for FCGs | FCGs often feel guilty or fearful when they cannot fulfill their perceived responsibilities. Role clarification may mitigate these feelings and help caregivers to feel more confident. There is a need for HCPs to clearly establish what is expected of the FCG on a daily basis. “What part of this care team do you want to play? The family caregiver ought to be given some of that role if they want it and are capable of doing it…we have to engage in the conversation upfront and ask the family caregiver.”(C-1, P) |
| Perform initial and ongoing FCG assessments | The physical and psychosocial status of FCGs should be assessed by trained professionals. Identifying the unique values and needs of each FCG may allow HCPs to offer specific, family-centred support. HCPs need to recognize that the care unit includes the patient who is ill as well as FCGs. “Is it going to be more time-consuming initially – absolutely, because we’re going to have to change the way we work, but down the road if we look at how those assessments are betting integrated, we’ve got carers involved, we start measuring quality of life – we might be in a different place.” (ACN-2, P) |
| Increase HCP understanding of senior-specific conditions and end-of-life care | HCPs lack an understanding of senior-specific conditions and end-of-life care. As such, they are not always able to provide FCGs with sufficient information or supportive resources. “…the family should sit down with someone to describe the disease and how it affects the person you love.” (C-3, G) |
| Advocate for policy change to address coding procedures | Policies should be changed to appropriately compensate HCPs for time spent with FCGs. Providing a code to bill for these interactions may encourage HCPs to engage with FCGs and reduce the tension between task demands and person-centred care. “The payment system for physicians to care about family caregiving, that’s what drives them. We have to take on the legislation of high-end FOIP and figure out how we can record on caregivers, and we also have to address the funding.” (OS-2, R) |
|
| |
| Key Theme 4. Fostering Resilience in Family Caregivers | |
|
| |
| Teach FCGs to self-identify signs of stress and employ stress-management strategies | HCPs can help FCGs self-identify signs of stress by providing information about symptoms and potential risk factors. Training for HCPs should include self-care strategies that can be taught to FCGs. Providing FCGs with coping strategies may prevent further deterioration, enhance well-being, and empower them to overcome challenging situations. “There is sorrow but there is joy. If you get that support, then really you’ve got a journey that’s not all that bad, like it’s hard but it’s not the end, there’s still hope.” (SN-3, Gy) |
| Empower FCGs by identifying their strengths and abilities | Helping FCGs to recognize their personal strengths and abilities may improve their perceived competence and foster feelings of hope. “If I asked a physician what is a strength-based approach on working with patients, I don’t know if they’d be able to articulate what that is.” (SN-2, P) |
| Community resilience hubs | Establishing networks where FCGs can connect for peer support may contribute to improving quality of life and building resilience. “A community resilience hub that is both virtual, like online for those that don’t want to come in, but also an actual meeting place where people can get peer support. There’s a lot of research around peer support, so a lot of brilliant strategies and interventions to help with people’s resilience.” (SN-3, Gy) |
| Prepare future generations for caregiving | HCPs should seek to educate and prepare younger generations for the inevitability that they will become FCGs in the future. Introducing upcoming generations to the caregiver role can increase awareness and empathy in the emerging population of future HCPs and FCGs. “…a need to start with kids, we’ve seen in our culture changes have come just because teachers are starting with kids.” (CC-1, black) |
|
| |
| Key Theme 5. Navigating Health and Social Systems and Accessing Resources | |
|
| |
| Increase HCPs understanding of the health-care system. | If HCPs understand the policies, resources, and services that make up the health-care system, they can better assist FCGs in navigating services and accessing appropriate resources. “I don’t believe every health professional should be expected to know everything about the whole system, but they should have enough wherewithal to know who and how, and who to connect families too appropriately.”(C-2, blue) |
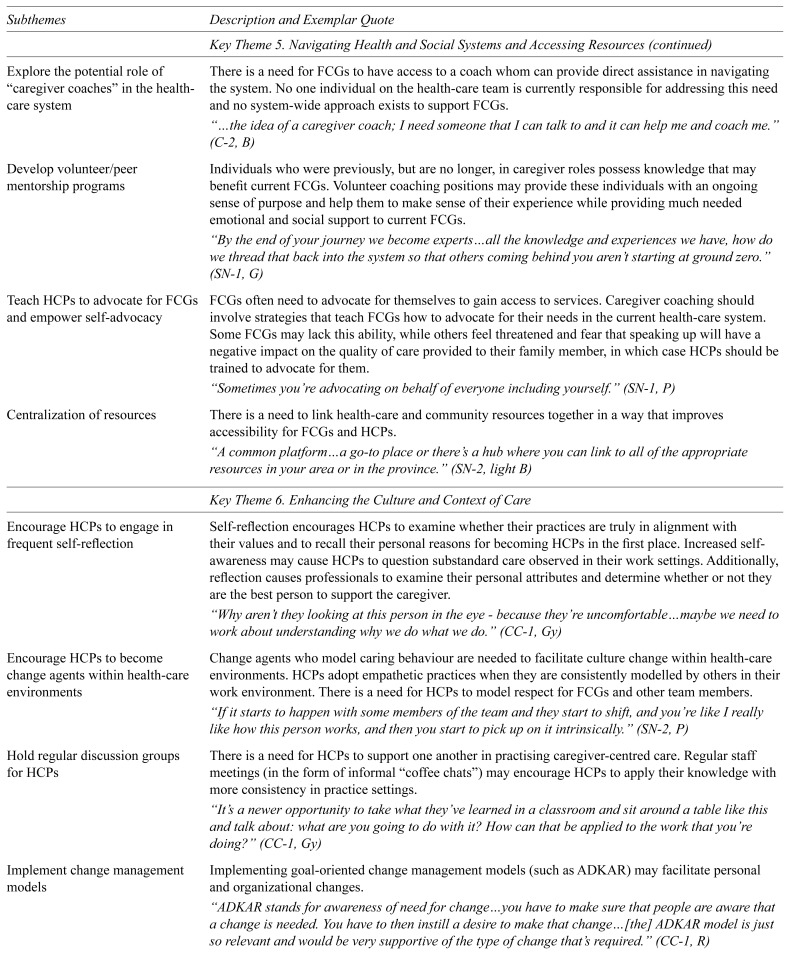
| Explore the potential role of “caregiver coaches” in the health-care system | There is a need for FCGs to have access to a coach whom can provide direct assistance in navigating the system. No one individual on the health-care team is currently responsible for addressing this need and no system-wide approach exists to support FCGs. “…the idea of a caregiver coach; I need someone that I can talk to and it can help me and coach me.” (C-2, B) |
| Develop volunteer/peer mentorship programs | Individuals who were previously, but are no longer, in caregiver roles possess knowledge that may benefit current FCGs. Volunteer coaching positions may provide these individuals with an ongoing sense of purpose and help them to make sense of their experience while providing much needed emotional and social support to current FCGs. “By the end of your journey we become experts…all the knowledge and experiences we have, how do we thread that back into the system so that others coming behind you aren’t starting at ground zero.” (SN-1, G) |
| Teach HCPs to advocate for FCGs and empower self-advocacy | FCGs often need to advocate for themselves to gain access to services. Caregiver coaching should involve strategies that teach FCGs how to advocate for their needs in the current health-care system. Some FCGs may lack this ability, while others feel threatened and fear that speaking up will have a negative impact on the quality of care provided to their family member, in which case HCPs should be trained to advocate for them. “Sometimes you’re advocating on behalf of everyone including yourself.” (SN-1, P) |
| Centralization of resources | There is a need to link health-care and community resources together in a way that improves accessibility for FCGs and HCPs. “A common platform…a go-to place or there’s a hub where you can link to all of the appropriate resources in your area or in the province.” (SN-2, light B) |
|
| |
| Key Theme 6. Enhancing the Culture and Context of Care | |
|
| |
| Encourage HCPs to engage in frequent self-reflection | Self-reflection encourages HCPs to examine whether their practices are truly in alignment with their values and to recall their personal reasons for becoming HCPs in the first place. Increased self-awareness may cause HCPs to question substandard care observed in their work settings. Additionally, reflection causes professionals to examine their personal attributes and determine whether or not they are the best person to support the caregiver. “Why aren’t they looking at this person in the eye - because they’re uncomfortable…maybe we need to work about understanding why we do what we do.” (CC-1, Gy) |
| Encourage HCPs to become change agents within health-care environments | Change agents who model caring behaviour are needed to facilitate culture change within health-care environments. HCPs adopt empathetic practices when they are consistently modelled by others in their work environment. There is a need for HCPs to model respect for FCGs and other team members. “If it starts to happen with some members of the team and they start to shift, and you’re like I really like how this person works, and then you start to pick up on it intrinsically.” (SN-2, P) |
| Hold regular discussion groups for HCPs | There is a need for HCPs to support one another in practising caregiver-centred care. Regular staff meetings (in the form of informal “coffee chats”) may encourage HCPs to apply their knowledge with more consistency in practice settings. “It’s a newer opportunity to take what they’ve learned in a classroom and sit around a table like this and talk about: what are you going to do with it? How can that be applied to the work that you’re doing?” (CC-1, Gy) |
| Implement change management models | Implementing goal-oriented change management models (such as ADKAR) may facilitate personal and organizational changes. “ADKAR stands for awareness of need for change…you have to make sure that people are aware that a change is needed. You have to then instill a desire to make that change…[the] ADKAR model is just so relevant and would be very supportive of the type of change that’s required.” (CC-1, R) |
| Improve communication between HCPs | There is a need for HCPs in different organizations and levels of care to accurately communicate information regarding FCGs. Doing so will reduce caregiver’s frustration and the need to repeatedly share information and advocate for their needs. “Communication [is needed] around how to engage with each other as care providers – which in the end extends to the family.” (CC-1, P) |
| Practice consistent language across health-care settings | Language creates culture. There is a need to eliminate language that invalidates and disrespects FCGs. Establishing guidelines for language may facilitate a culture shift that honours and respects FCGs. “We need to work towards consistent language, and that’s as simple as creating a definition document. We have to change our own language and the way we write, communicate, and speak, so that helps create change elsewhere.” (ACN-3, P) |
| Increase interdependence and multidisciplinary practice | There is a tendency for HCPs to operate in silos. Sharing knowledge and resources between HCPs facilitates more holistic patient care. There is a need to implement an interdisciplinary team approach that extends to community resources when working with FCGs. “I want health-care providers to get over their egos and the system to be less siloed so that people do really think about my needs and where I need to go, and integrated care so I don’t tell my story over and over again, so all my information is in one system that everybody shares – that would be ideal.” (C-2, B) |