Abstract
Introduction
Postlaparoscopic shoulder pain (PLSP) has been well documented to effect patients following an abdominal or thoracic laparoscopic surgery. PLSP is characterized by referred pain that can occur both unilaterally or bilaterally, and is typically caused by phrenic nerve irritation. Current literature has focused on pharmacological treatment; however, there is limited evidence for the use of nonpharmacological management of PLSP in the pediatric population.
Case Description
This retrospective case report study explores the use of a single-session massage therapy treatment for a 17-year-old patient with PLSP following laparoscopic abdominal surgery.
Intervention and Results
Therapy intervention included a 25 min Swedish massage involving the effected shoulder with an emphasis on passive touch to the shoulder and at the level of the diaphragm. Pain was assessed using the Visual Analog Scale (VAS) pre- and postintervention. Following therapy the patient reported 0/10 pain.
Conclusion
This case report provides evidence for the use of massage therapy treatment as a noninvasive, nonpharmacological approach to reducing or eliminating PLSP in a pediatric patient.
Keywords: case report, phrenic nerve, shoulder pain, massage therapy, postlaparoscopic shoulder pain, nonpharmacological
INTRODUCTION
The popularity of laparoscopic surgery has grown in the pediatric population as instrumentation, training, and techniques have evolved.(1–3) In one center, laparoscopic surgeries for pediatric appendectomies grew from 10% in 1997 to 95% in 2005.(4) Similar trends exist for other pediatric procedures including bowel, thoracic, and gynecological surgeries.
During a laparoscopic procedure, carbon dioxide (CO2) is pumped into the abdominal cavity to separate the abdominal wall from the peritoneum and organs. This is done to create working area for the surgical procedure. The temperature of the CO2 is colder than the temperature of the body, and residual CO2 may be left in the abdomen at the end of surgery. These two factors can contribute to phrenic nerve irritation and lead to spasms in the diaphragm.(5,6)
Phrenic nerve irritation, following a laparoscopic surgery, can impact both motor and sensory functions.(7) Multiple research studies have hypothesized that PLSP is due to phrenic nerve irritation at the diaphragmatic level, creating referred pain sensations around the shoulder unilaterally or bilaterally.(5,6,8,9–12) According to Lee et al.,(9) up to 80% of patients experience postlaparoscopic shoulder pain. The phrenic nerve originates at cervical nerve roots, C3, C4, and C5, and descends deep to the anterior scalene muscle. It then enters the thorax and travels between the pericardium and the parietal pleura, inserting bilaterally at the level of the diaphragm. This nerve’s motor role serves as the primary driver of respiration, controlling the diaphragm.(13) The sensory role provides the cutaneous, sensory innervation for the skin over the shoulder (dermatomes C3–C5).(5)
Current high-risk medical intervention for PLSP involves the use of analgesic administration, including opioids and various invasive techniques, to decrease or eliminate pain. These techniques may include the use of epidural analgesia,(5,14) nerve catheter placement surrounding the phrenic nerve in the neck,(12) ultrasound-guided analgesic injection into the phrenic nerve in the neck,(11) and use of saline to flush ports.(10) Risks of these interventions can include diaphragm paralysis,(14) potential motor blockage of the shoulder muscles,(12) and decrease of right-sided diaphragmatic excursion putting patients at risk for pulmonary insufficiency.(11)
In order to decrease medication use, massage therapy techniques have historically been utilized as a nonpharmacologic approach to address pain.(15,16) Research supports massage therapy as safe and effective for pediatric patients, including management of postprocedural pain.(17,18) Massage clinical reasoning utilizes two well-documented theories to address pain: the gate control theory and parasympathetic nervous system engagement.(15,19) The gate control theory suggests that massage may be effective at inhibiting the conduction of noxious stimuli by activating large nerve fibers, thereby closing the gate and changing the perception of pain as it is communicated to the brain.(15,20) In parasympathetic nervous system engagement, massage therapy techniques are used to disengage the overstimulated sympathetic nervous system and increase parasympathetic activity, thereby reducing pain.(19,21) Adams et al.(15) also suggest that, by engaging the parasympathetic nervous system, massage can decrease the body’s autonomic stress responses(19) and enhance the ability to rest.
Massage therapy intervention is a non-pharmacological modality utilized to treat pain in postoperative patients; however, the effect of treatment on postoperative phrenic nerve irritation is unknown. The objective of this case report is to describe the effect of a single-session massage therapy intervention for a pediatric patient experiencing PLSP after laparoscopic abdominal surgery.
METHODS
Case Description
A 17-year-old male experienced PLSP following abdominal surgery. Massage therapy was consulted by the patient’s primary medical team postoperatively Day One to assist with his reported shoulder pain.
The patient described new onset right shoulder pain, which was not present preoperatively. He denied any abdominal pain related to his procedure. His shoulder pain was described as a constant sharp ache that was global to his shoulder, with concentration of pain located along the superior portion of the trapezius muscle. For the purpose of this case report, the Visual Analog Scale (VAS) was used to measure the severity of his postoperative shoulder pain.
The VAS was located in the hospital room within the patient’s line of sight. The patient was asked to review the scale and report the pain number verbally. The score 0 on the VAS scale indicated “no pain” and the score 10 indicated the worst pain possible. He was asked to state a score from 0 to 10 both pre- and postmassage therapy session.
Utilizing the VAS, he rated his shoulder pain as a 5/10 at the beginning of massage therapy treatment. Interventions to address PLSP pain prior to massage therapy included opioids, nonsteroidal anti-inflammatory drugs (NSAIDS), ambulation, and position changes; however, the patient denied relief from any of these techniques.
Intervention
Patient was supine in his hospital bed during massage therapy. This position was chosen by the patient as being the most comfortable for his abdominal incision. Therapy was provided by a licensed massage therapist (LMT) with over 11 years of experience. The focus of this 25-minute treatment was to address the referred pain of his right shoulder.
The session started with the LMT providing passive touch to the right neck, right shoulder, and superior right arm. Effleurage was utilized from the midneck through superior and posterior shoulder in order to warm tissues for more specific massage (Table 1). The therapist then provided light-to-medium pressure effleurage, cross-fiber friction, and petrissage techniques on scalene and superior trapezius muscles. The purpose of these techniques was to relieve tension believed to be contributing to the phrenic nerve entrapment and irritation.
Table 1.
Massage Intervention
| MT Technique | Area | Time | Lotion Used |
|---|---|---|---|
| 1. Passive touch |
|
2 min | No lotion |
| 2. Effleurage |
|
3 min | Organic/unscented lotion |
| 3. Effleurage, petrissage, and cross fiber friction |
|
10 min | Organic/unscented lotion |
| 4. Trigger point therapy |
|
5 min | Organic/unscented lotion |
| 5. Passive touch |
|
5 min | No lotion |
During effleurage, the therapist noted multiple trigger points in the inferior trapezius and rhomboid major and minor muscles. Therefore, moderate pressure trigger point massage was given as individualized intervention.
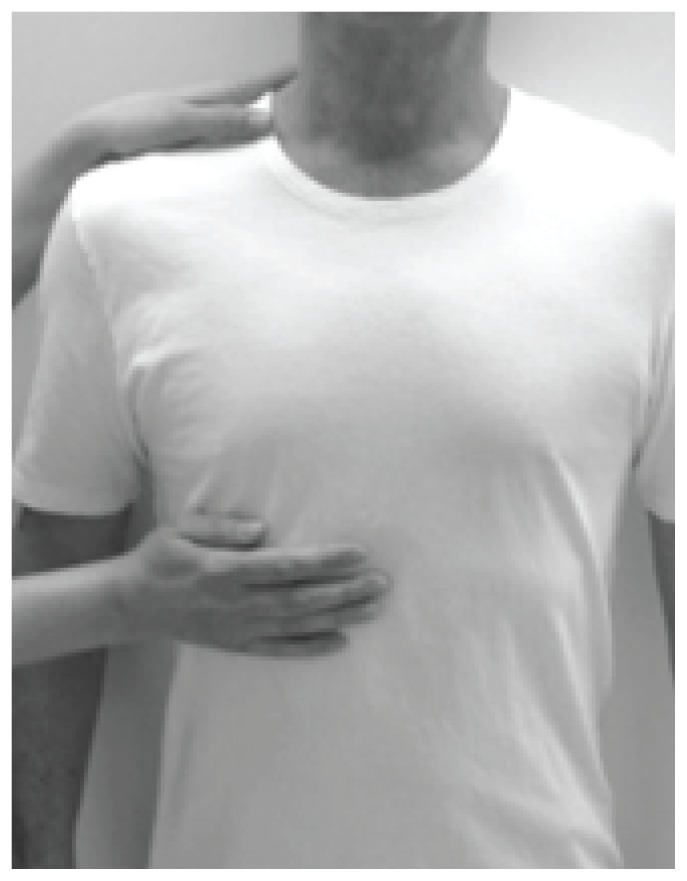
To address the referred shoulder pain, light passive touch was provided to the right shoulder and the level of right diaphragm, with care not to elicit pressure onto the diaphragm or abdomen. The therapist placed one hand on the right superior shoulder along the superior border of the trapezius. The other hand was held with the fingers positioned near the xiphoid process of the sternum and extending laterally toward the patient’s side at the level of the diaphragm, over the 7th to the 10th ribs (Figure 1). The therapist’s hands were sustained in this positional hold for 5 min.
Figure 1.
Hand position to address PLSP at shoulder and diaphragm.
RESULTS
The LMT observed the patient appeared more relaxed, with decreased muscle tension at the completion of his initial massage therapy session. The patient reported his right shoulder pain as 0/10 utilizing the VAS scale at the conclusion of massage therapy. The LMT returned the next date and the patient reported his right shoulder pain had not returned; therefore, massage therapy to address shoulder pain was no longer indicated. Per retrospective chart review, the patient’s shoulder pain did not return prior to discharge from the hospital, and the patient experienced no adverse events from therapy.
DISCUSSION
This article presents a case report which supports the use of massage therapy as a safe and feasible nonpharmacological technique to reduce PLSP in a pediatric patient following laparoscopic surgery. Both Kukimoto et al.(16) and Adams et al.(15) encourage the use of massage therapy as a safe form of treatment for postoperative pain management in the hospital setting. We also found this to be true, as no adverse events occurred during nor were reported after massage therapy for this patient. In regard to the feasibility of the use of a non-pharmacological approach for PLSP, we found one study which utilizes individualized acupuncture to address PLSP.(22) This article, like our case report, notes the feasibility of a nonpharmacologic approach; however, it also reports causality cannot be inferred due to confounding variables. Similar to our case report, this article notes that the patient’s PLSP was not relieved by postoperative analgesics, and found immediate pain relief was reported following the nonpharmacologic treatment.
Current research identifies the use of high-risk procedures and oral pain medications as the standard treatments to address PLSP. Current literature notes that opioid use in pediatrics is rising, and there is an urgent push by the Centers for Disease Control and Prevention to decrease use of opioids and pain medication and consider the use of more nonpharmacological methods to address pain.(17,23) Lee et al.(9) reports PLSP is not responsive to analgesics when compared to the patient’s surgical site pain, and our findings in this case report support this. Due to these findings, patients are at risk for excessive use of opioids and oral pain medication during this time in attempt to alleviate PLSP. We suggest considering the use of massage therapy as a nonpharmacological treatment in conjunction with standard medication administration, possibly reducing the need for excessive use of analgesics.
Although there was notable improvement in the patient’s PLSP, this case report does present with some limitations. As the patient continued to receive standard-of-care treatment analgesics for his postoperative pain during this time, we cannot conclusively infer that the pain relief was isolated to the massage treatment. Assessment of pain was only conducted pre- and posttreatment. The multiple treatment techniques during the session make it unclear whether the pain relief was due to the isolated passive diaphragm and shoulder hold. More frequent VAS assessments are needed throughout the session to determine the specific technique that may lead to pain relief. Finally, although a retrospective chart review was completed to track pain through the remainder of the admission, only one in-person follow-up was performed by the massage therapist to request specific feedback on shoulder pain. Future strategies could include obtaining daily feedback from each patient, specific to shoulder pain.
Despite these limitations, there was a notable improvement in the patient’s PLSP from pre- to postmassage therapy treatment. Further studies with a greater number of pediatric patients, as well as more consistent follow-up, are needed to determine if massage therapy is a suitable nonpharmacological approach to treating patients with PLSP.
CONCLUSION
The results of this case report provide evidence supporting the use of massage therapy intervention in the management of PLSP following a laparoscopic abdominal surgery on a pediatric patient. Massage therapy may provide a noninvasive, nonpharmacological approach to reducing or eliminating PLSP. Further studies evaluating a greater number of pediatric patients are needed to support massage therapy as an important nonpharmacological strategy in treating PLSP.
ACKNOWLEDGMENTS
We wish to acknowledge Jake Jurbank and Rachel Bican for their substantial contributions to this case report.
Footnotes
CONFLICT OF INTEREST NOTIFICATION
The authors declare there are no conflicts of interest.
REFERENCES
- 1.Meehan JJ, Georgeson KE. The learning curve associated with laparoscopic antireflux surgery in infants and children. J Pediatr Surg. 1997;32(3):426–429. doi: 10.1016/S0022-3468(97)90597-2. [DOI] [PubMed] [Google Scholar]
- 2.Zitsman JL. Current concepts in minimal access surgery for children. Pediatrics. 2003;111(6 Pt 1):1239–1252. doi: 10.1542/peds.111.6.1239. [DOI] [PubMed] [Google Scholar]
- 3.Georgeson KE, Owings E. Advances in minimally invasive surgery in children. Am J Surg. 2000;180(5):362–364. doi: 10.1016/S0002-9610(00)00554-7. [DOI] [PubMed] [Google Scholar]
- 4.Zitsman JL. Pediatric minimal-access surgery: update 2006. Pediatrics. 2006;118(1):304–308. doi: 10.1542/peds.2005-2736. [DOI] [PubMed] [Google Scholar]
- 5.Scawn ND, Pennefather SH, Soorae A, Wang JY, Russell GN. Ipsilateral shoulder pain after thoracotomy with epidural analgesia: the influence of phrenic nerve infiltration with lidocaine. Anesth Analg. 2001;93(2):260–264. doi: 10.1097/00000539-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Yousefshahi F, Predescu O, Colizza M, Asenjo JF. Postthoracotomy ipsilateral shoulder pain: a literature review on characteristics and treatment. Pain Res Manag. 2016;2016 doi: 10.1155/2016/3652726. 3652726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arendt-Nielsen L, Fernandez-de-Las-Penas C, Graven-Nielsen T. Basic aspects of musculoskeletal pain: from acute to chronic pain. J Man Manip Ther. 2011;19(4):186–193. doi: 10.1179/106698111X13129729551903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lollino N, Brunocilla PR, Poglio F, Vannini E, Lollino S, Lancia M. Non-orthopaedic causes of shoulder pain: what the shoulder expert must remember. Musculoskelet Surg. 2012;96(1):S63–S68. doi: 10.1007/s12306-012-0192-5. [DOI] [PubMed] [Google Scholar]
- 9.Lee DH, Song T, Kim KH, Lee KW. Incidence, natural course, and characteristics of postlaparoscopic shoulder pain. Surg Endosc. 2018;32(1):160–165. doi: 10.1007/s00464-017-5651-5. [DOI] [PubMed] [Google Scholar]
- 10.Suginami R, Taniguchi F, Suginami H. Prevention of postlaparoscopic shoulder pain by forced evacuation of residual CO2. JSLS. 2009;13(1):56–59. [PMC free article] [PubMed] [Google Scholar]
- 11.Yi MS, Kim WJ, Kim MK, Kang H, Park YH, Jung YH, et al. Effect of ultrasound-guided phrenic nerve block on shoulder pain after laparoscopic cholecystectomy-a prospective, randomized controlled trial. Surg Endosc. 2017;31(9):3637–3645. doi: 10.1007/s00464-016-5398-4. [DOI] [PubMed] [Google Scholar]
- 12.Blichfeldt-Eckhardt MR, Laursen CB, Berg H, Holm JH, Hansen LN, Ørding H, et al. A randomised, controlled, double-blind trial of ultrasound-guided phrenic nerve block to prevent shoulder pain after thoracic surgery Anaesthesia 20167112: 1441–1448. 10.1111/anae.13621 [DOI] [PubMed] [Google Scholar]
- 13.Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics. 2012;32(2):E51–E70. doi: 10.1148/rg.322115127. [DOI] [PubMed] [Google Scholar]
- 14.Greene CL, Mainwaring RD, Sidell D, Yarlagadda VV, Patrick WL, Hanley FL. Impact of phrenic nerve palsy and need for diaphragm plication following surgery for pulmonary atresia with ventricular septal defect and major aortopulmonary collaterals. Semin Thorac Cardiovasc Surg. 2018;30(3):318–324. doi: 10.1053/j.semtcvs.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Adams R, White B, Beckett C. The effects of massage therapy on pain management in the acute care setting. Int J Ther Massage Bodywork. 2010;3(1):4–11. [PMC free article] [PubMed] [Google Scholar]
- 16.Kukimoto Y, Ooe N, Ideguchi N. The effects of massage therapy on pain and anxiety after surgery: a systematic review and meta-analysis. Pain Manag Nurs. 2017;18(6):378–390. doi: 10.1016/j.pmn.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Evans S, Tsao JC, Zeltzer LK. Complementary and alternative medicine for acute procedural pain in children. Altern Ther Health Med. 2008;14(5):52–56. [PubMed] [Google Scholar]
- 18.Jenkins BN, Vincent N, Fortier MA. Differences in referral and use of complementary and alternative medicine between pediatric providers and patients. Complement Ther Med. 2015;23(3):462–468. doi: 10.1016/j.ctim.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Diego MA, Field T. Moderate pressure massage elicits a parasympathetic nervous system response. Int J Neurosci. 2009;119(5):630–638. doi: 10.1080/00207450802329605. [DOI] [PubMed] [Google Scholar]
- 20.Mendell LM. Constructing and deconstructing the gate theory of pain. Pain. 2014;155(2):210–216. doi: 10.1016/j.pain.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan L, Collet JP, Yuskiv N, Skippen P, Brant R, Kissoon N. The effect of massage therapy on autonomic activity in critically ill children. Evid Based Complement Alternat Med. 2014;2014 doi: 10.1155/2014/656750. 656750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kreindler G, Attias S, Kreindler A, Han H, Haj B, Matter I, et al. Treating postlaparoscopic surgery shoulder pain with acupuncture. Evid Based Complement Alternat Med. 2014;2014 doi: 10.1155/2014/120486. 120486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]